Soothe Foot Pain Fast With These Simple SolutionsSoothe Foot Pain Fast With These Simple Solutions
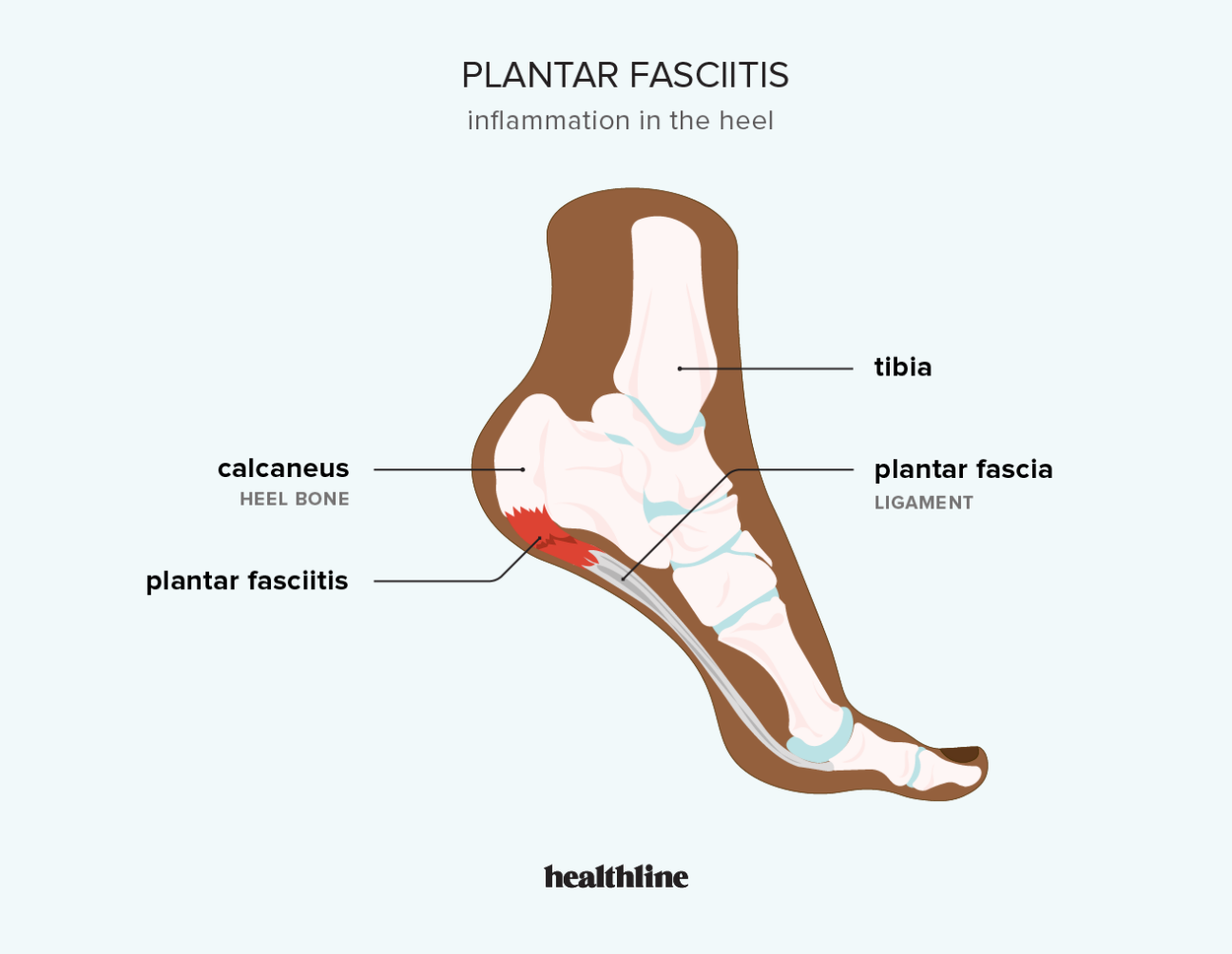
If you’ve ever felt a sharp, stabbing pain in your heel or arch after getting up from bed in the morning or standing up after sitting for awhile, you know how debilitating plantar fasciitis can be. This common condition stems from inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of your foot. When this connective tissue becomes irritated and inflamed, it causes pain and stiffness that can make every step excruciating. Luckily, there are many simple yet effective ways to find relief from plantar fasciitis flare-ups. Let’s explore some do-it-yourself home treatments, braces, lifestyle tweaks, and medical procedures that can help ease your heel and arch pain so you can get back on your feet comfortably.
Intro – What is plantar fasciitis and why does it cause foot pain?
The plantar fascia is a broad, thick band of fibrous connective tissue that runs along the bottom of your foot. It extends from your heel bone forward to the ball of your foot, helping form the arch and providing support and stability as you walk or run. When this tendon-like tissue becomes inflamed due to overuse or injury, the resulting condition is known as plantar fasciitis. Tiny tears or inflammation within the fascia cause irritation, swelling, and sharp stabbing pain. The pain is usually most pronounced with your first steps in the morning or after long periods of inactivity when the fascia tightens up. Continued stress and strain on the inflamed tissue leads to worsening discomfort and difficulty walking or standing. Understanding what causes the inflammation in the first place helps guide treatment.
Symptoms – Heel and arch pain that worsens after rest

The classic symptom of plantar fasciitis is pain and stiffness in your heel or arch, especially first thing in the morning when getting out of bed. The pain usually decreases somewhat with motion but worsens again after long periods of standing or sitting. Pain may radiate from your heel forward along the bottom of your foot. You may notice the pain after increases in activity levels like starting a new workout routine. Tenderness or pain when pressing along the plantar fascia is another common symptom. Left untreated, the pain can become persistent and interferes with daily activities.
Causes – Tight calf muscles, high arches, excess weight, repetitive stress
A variety of factors can contribute to developing plantar fasciitis including tight or weak calf muscles, high arches, being overweight, and repetitive stress or strain to the feet. Tight calf muscles cause excessive pulling on the plantar fascia leading to inflammation and pain. People with high arches are also more prone since their feet roll inward more excessively when walking. Excess weight puts added stress on the plantar fascia leading to inflammation. Runners or athletes who routinely pound their feet on hard surfaces without rest are also at risk, as are those whose jobs involve long hours of standing or walking like factory workers, nurses, teachers, etc. Identifying the underlying causes helps determine the best treatment approach.
Risk Factors – Runners, overweight, jobs requiring standing, flat feet
Certain groups are at higher risk of developing plantar fasciitis including runners, those who are overweight, people whose jobs require long hours of standing, and those with flat feet or high arches. Runners subject their feet to repetitive high impact stress during training, leading to irritation of the plantar fascia over time. Excess weight also strains the plantar fascia with every step. Occupations like nursing or factory work that involve prolonged standing and walking on hard surfaces commonly lead to plantar fasciitis. Those with flat feet or abnormally high arches are also more prone due to poor foot mechanics. Knowing your risk factors allows you to take preventative steps.
Diagnosis – Physical exam, medical history, imaging tests
To diagnose plantar fasciitis, your doctor will perform a physical exam of your foot, assess your medical history, and ask about your symptoms. They will palpate along the plantar fascia looking for areas of tenderness and check your range of motion. Be prepared to describe the exact location of your pain and what makes it better or worse. Your doctor may order imaging tests like x-rays or an MRI to rule out other potential causes of heel pain like stress fractures, bone spurs, or nerve issues. Plantar fasciitis can usually be diagnosed from the classic symptoms and exam findings alone.
Treatment – Rest, ice, OTC pain relievers, stretching, orthotics
Why does plantar fasciitis cause such intense foot pain?
The intensity of pain associated with plantar fasciitis is due to the constant stress placed on the affected area. Every time you take a step, the inflamed tissue is stretched and compressed, exacerbating the discomfort. Additionally, the plantar fascia has a poor blood supply, which means it heals slowly, prolonging the recovery process and potentially leading to chronic pain if left untreated.
Recognizing the Symptoms: Identifying Plantar Fasciitis
Identifying plantar fasciitis early is crucial for effective treatment and prevention of long-term complications. The most common symptoms include:
- Sharp, stabbing pain in the heel or arch of the foot
- Increased pain after periods of rest, especially in the morning
- Pain that worsens after prolonged standing or physical activity
- Tenderness along the bottom of the foot
- Difficulty walking or climbing stairs
It’s important to note that the pain associated with plantar fasciitis often diminishes as you move around and the fascia stretches out. However, it may return after long periods of standing or sitting, creating a cycle of discomfort throughout the day.
How does plantar fasciitis pain differ from other foot conditions?
Unlike other foot conditions, plantar fasciitis pain is typically localized to the heel and arch area. It’s often described as a sharp, stabbing sensation rather than a dull ache. The pain is most intense during the first steps after a period of rest, which is a distinguishing feature of this condition. This characteristic helps differentiate plantar fasciitis from other foot ailments such as stress fractures or nerve problems.
Underlying Causes: Factors Contributing to Plantar Fasciitis
Understanding the root causes of plantar fasciitis is essential for effective treatment and prevention. Several factors can contribute to the development of this condition:
- Tight calf muscles: Shortened calf muscles can put excessive strain on the plantar fascia.
- Foot structure: High arches or flat feet can increase the risk of developing plantar fasciitis.
- Obesity: Excess weight puts additional stress on the plantar fascia.
- Repetitive stress: Activities that involve prolonged standing, walking, or running can overload the fascia.
- Improper footwear: Shoes with inadequate support or poor cushioning can contribute to fascia strain.
- Age: The plantar fascia loses elasticity as we age, making it more susceptible to inflammation.
Can sudden changes in activity levels trigger plantar fasciitis?
Yes, sudden increases in physical activity or changes in exercise routines can trigger plantar fasciitis. This is often seen in individuals who abruptly start a new workout regimen or intensify their training without proper gradual progression. The plantar fascia needs time to adapt to increased stress, and rapid changes can overwhelm its capacity to recover, leading to inflammation and pain.

Identifying Risk Factors: Who’s Most Susceptible to Plantar Fasciitis?
While plantar fasciitis can affect anyone, certain groups are at higher risk of developing this condition. Understanding these risk factors can help individuals take proactive measures to prevent or manage plantar fasciitis:
- Runners and athletes: Regular high-impact activities put significant stress on the plantar fascia.
- Overweight individuals: Excess body weight increases the load on the feet with each step.
- Occupational hazards: Jobs requiring long hours of standing or walking on hard surfaces increase risk.
- Foot anatomy: People with flat feet or high arches are more prone to plantar fasciitis.
- Age group: The condition is most common in adults aged 40-60.
- Pregnancy: Weight gain and hormonal changes during pregnancy can contribute to plantar fasciitis.
How does occupational stress contribute to plantar fasciitis?
Occupations that involve prolonged standing or walking on hard surfaces, such as teaching, nursing, or factory work, can significantly increase the risk of developing plantar fasciitis. The constant pressure and repetitive stress on the feet can lead to micro-tears in the plantar fascia, resulting in inflammation and pain. Additionally, jobs that require frequent climbing, lifting heavy objects, or operating foot-controlled machinery can also contribute to the development of this condition by placing excessive strain on the plantar fascia.

Diagnostic Approaches: Confirming Plantar Fasciitis
Accurate diagnosis of plantar fasciitis is crucial for effective treatment. Healthcare professionals employ various methods to confirm the condition and rule out other potential causes of foot pain:
- Physical examination: The doctor will palpate the foot to identify areas of tenderness and assess flexibility.
- Medical history review: A detailed discussion of symptoms, lifestyle, and previous injuries helps pinpoint the cause.
- Gait analysis: Observing how a patient walks can reveal biomechanical issues contributing to plantar fasciitis.
- Imaging tests: X-rays, MRI, or ultrasound may be used to rule out other conditions or visualize the fascia.
Why are imaging tests sometimes necessary for diagnosing plantar fasciitis?
While plantar fasciitis can often be diagnosed based on symptoms and physical examination alone, imaging tests may be necessary in certain cases. These tests help rule out other conditions that can mimic plantar fasciitis symptoms, such as stress fractures, heel spurs, or tarsal tunnel syndrome. X-rays can reveal bone spurs or fractures, while MRI or ultrasound can provide detailed images of soft tissues, allowing doctors to assess the extent of inflammation or damage to the plantar fascia. This comprehensive approach ensures accurate diagnosis and appropriate treatment planning.
Effective Treatments: Alleviating Plantar Fasciitis Pain
Treating plantar fasciitis often involves a multifaceted approach, combining various strategies to reduce pain, promote healing, and prevent recurrence. Common treatment options include:
- Rest and ice: Reducing stress on the affected foot and applying ice can help alleviate pain and inflammation.
- Stretching exercises: Regular stretching of the calf muscles and plantar fascia can improve flexibility and reduce pain.
- Orthotics and supportive footwear: Custom orthotics or shoes with good arch support can help distribute pressure more evenly.
- Night splints: These devices keep the plantar fascia stretched overnight, reducing morning pain.
- Physical therapy: Targeted exercises and manual techniques can strengthen the foot and improve flexibility.
- Medications: Over-the-counter pain relievers or anti-inflammatory drugs can help manage pain and inflammation.
- Extracorporeal shock wave therapy: This non-invasive treatment uses sound waves to stimulate healing.
How effective are corticosteroid injections for treating plantar fasciitis?
Corticosteroid injections can be an effective short-term solution for severe plantar fasciitis pain. These injections deliver potent anti-inflammatory medication directly to the affected area, providing rapid relief. However, their use is typically limited due to potential side effects, including weakening of the plantar fascia with repeated injections. While corticosteroid injections can offer quick pain relief, they are often considered after conservative treatments have failed and are usually combined with other therapies for optimal long-term management of the condition.
Preventive Measures: Reducing the Risk of Plantar Fasciitis
Preventing plantar fasciitis is often easier than treating it. By adopting certain lifestyle changes and habits, individuals can significantly reduce their risk of developing this painful condition:
- Maintain a healthy weight: Excess weight puts additional stress on the plantar fascia.
- Choose appropriate footwear: Wear shoes with good arch support and cushioning, especially during physical activities.
- Gradually increase activity levels: Avoid sudden increases in exercise intensity or duration.
- Stretch regularly: Incorporate calf and foot stretches into your daily routine.
- Cross-train: Alternate high-impact activities with low-impact exercises to reduce stress on the feet.
- Use proper technique: Ensure correct form during exercise to minimize unnecessary strain on the feet.
- Replace worn-out shoes: Athletic shoes should be replaced every 400-500 miles to maintain proper support.
Can specific exercises help prevent plantar fasciitis?
Yes, targeted exercises can play a crucial role in preventing plantar fasciitis. Regular stretching of the calf muscles, Achilles tendon, and plantar fascia can improve flexibility and reduce the risk of developing this condition. Toe curls, heel raises, and rolling a tennis ball under the foot can strengthen the intrinsic foot muscles and promote better arch support. Additionally, exercises that focus on improving overall lower body strength and flexibility, such as lunges and squats, can contribute to better biomechanics and reduce strain on the plantar fascia during daily activities and physical exercise.

Long-Term Implications: Understanding Chronic Plantar Fasciitis
While many cases of plantar fasciitis resolve with proper treatment and care, some individuals may experience chronic or recurrent symptoms. Understanding the potential long-term implications of untreated or poorly managed plantar fasciitis is crucial:
- Chronic pain: Persistent inflammation can lead to ongoing discomfort and reduced quality of life.
- Altered gait: Compensating for foot pain can lead to changes in walking patterns, potentially affecting other joints.
- Reduced activity levels: Chronic pain may limit participation in physical activities and exercise.
- Psychological impact: Persistent pain and limitations can contribute to stress, anxiety, or depression.
- Increased risk of other injuries: Compensatory movements may lead to overuse injuries in other parts of the body.
- Plantar fascia rupture: In rare cases, severe or untreated plantar fasciitis can lead to a tear in the fascia.
How does chronic plantar fasciitis affect overall foot health?
Chronic plantar fasciitis can have far-reaching effects on overall foot health. Prolonged inflammation and micro-tears in the plantar fascia can lead to degenerative changes in the tissue, reducing its elasticity and strength. This can result in a flattening of the foot arch over time, altering the foot’s biomechanics and potentially leading to additional foot problems such as heel spurs or midfoot arthritis. The ongoing pain and discomfort may also cause individuals to adopt abnormal walking patterns, which can put stress on other parts of the foot, ankle, and lower leg, potentially leading to secondary injuries or conditions. Regular monitoring and proactive management are essential to prevent these long-term complications and maintain optimal foot health.

If you’ve ever felt a sharp, stabbing pain in your heel or arch after getting up from bed in the morning or standing up after sitting for awhile, you know how debilitating plantar fasciitis can be. This common condition stems from inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of your foot. When this connective tissue becomes irritated and inflamed, it causes pain and stiffness that can make every step excruciating. Luckily, there are many simple yet effective ways to find relief from plantar fasciitis flare-ups. Let’s explore some do-it-yourself home treatments, braces, lifestyle tweaks, and medical procedures that can help ease your heel and arch pain so you can get back on your feet comfortably.
Intro – What is plantar fasciitis and why does it cause foot pain?
The plantar fascia is a broad, thick band of fibrous connective tissue that runs along the bottom of your foot. It extends from your heel bone forward to the ball of your foot, helping form the arch and providing support and stability as you walk or run. When this tendon-like tissue becomes inflamed due to overuse or injury, the resulting condition is known as plantar fasciitis. Tiny tears or inflammation within the fascia cause irritation, swelling, and sharp stabbing pain. The pain is usually most pronounced with your first steps in the morning or after long periods of inactivity when the fascia tightens up. Continued stress and strain on the inflamed tissue leads to worsening discomfort and difficulty walking or standing. Understanding what causes the inflammation in the first place helps guide treatment.
Symptoms – Heel and arch pain that worsens after rest

The classic symptom of plantar fasciitis is pain and stiffness in your heel or arch, especially first thing in the morning when getting out of bed. The pain usually decreases somewhat with motion but worsens again after long periods of standing or sitting. Pain may radiate from your heel forward along the bottom of your foot. You may notice the pain after increases in activity levels like starting a new workout routine. Tenderness or pain when pressing along the plantar fascia is another common symptom. Left untreated, the pain can become persistent and interferes with daily activities.
Causes – Tight calf muscles, high arches, excess weight, repetitive stress
A variety of factors can contribute to developing plantar fasciitis including tight or weak calf muscles, high arches, being overweight, and repetitive stress or strain to the feet. Tight calf muscles cause excessive pulling on the plantar fascia leading to inflammation and pain. People with high arches are also more prone since their feet roll inward more excessively when walking. Excess weight puts added stress on the plantar fascia leading to inflammation. Runners or athletes who routinely pound their feet on hard surfaces without rest are also at risk, as are those whose jobs involve long hours of standing or walking like factory workers, nurses, teachers, etc. Identifying the underlying causes helps determine the best treatment approach.
Risk Factors – Runners, overweight, jobs requiring standing, flat feet
Certain groups are at higher risk of developing plantar fasciitis including runners, those who are overweight, people whose jobs require long hours of standing, and those with flat feet or high arches. Runners subject their feet to repetitive high impact stress during training, leading to irritation of the plantar fascia over time. Excess weight also strains the plantar fascia with every step. Occupations like nursing or factory work that involve prolonged standing and walking on hard surfaces commonly lead to plantar fasciitis. Those with flat feet or abnormally high arches are also more prone due to poor foot mechanics. Knowing your risk factors allows you to take preventative steps.
Diagnosis – Physical exam, medical history, imaging tests
To diagnose plantar fasciitis, your doctor will perform a physical exam of your foot, assess your medical history, and ask about your symptoms. They will palpate along the plantar fascia looking for areas of tenderness and check your range of motion. Be prepared to describe the exact location of your pain and what makes it better or worse. Your doctor may order imaging tests like x-rays or an MRI to rule out other potential causes of heel pain like stress fractures, bone spurs, or nerve issues. Plantar fasciitis can usually be diagnosed from the classic symptoms and exam findings alone.
Treatment – Rest, ice, OTC pain relievers, stretching, orthotics
There are many conservative treatment options to try for plantar fasciitis before considering more invasive procedures. Resting your feet, icing the area, using over-the-counter pain medication, doing foot stretches and exercises, and using custom orthotics or night splints are simple yet effective approaches. Limiting activity that aggravates your feet, applying ice packs to reduce inflammation, and taking anti-inflammatory meds like ibuprofen can provide symptom relief. Regular stretching keeps your plantar fascia flexible while orthotics support your arches. Talk to your doctor to develop a comprehensive treatment plan.
Braces & Wraps – Compression and support for the plantar fascia
Specialized braces and compression wraps provide targeted support and pain relief by stabilizing the foot and reducing strain on the inflamed plantar fascia. Options like Copper Fit compression sleeves, ice wraps, and arch supports use gentle compression and adjustable straps to ease pain. The Copper Fit Ice line combines compression with cooling copper-infused fabric to reduce inflammation. The arch supports relieve strain on the plantar fascia by supporting the foot’s arch. These braces can be worn under shoes or at night for continuous relief.
Night Splints – Keep the foot flexed during sleep to stretch fascia

Night splints are an effective treatment option because they gently stretch and lengthen the plantar fascia overnight while you sleep. They hold your foot in a flexed position which keeps the plantar fascia stretched mildly to prevent it tightening up overnight. Immobilizing the foot in this extended position helps reduce morning pain and stiffness. It may take several weeks of continuous night splint use to achieve noticeable improvement. Many types are adjustable to fit your specific needs.
Physical Therapy – Stretches, strengthening exercises, massage
Visiting a physical therapist can provide significant relief through tailored stretches and exercises that target the plantar fascia and calf muscles. They will show you specific foot and ankle strengthening moves. Manual techniques like deep tissue massage and trigger point therapy applied directly to the plantar fascia can also help release tightness and adhesions. Therapeutic ultrasound may also be used to stimulate blood flow and enhance healing. A customized therapy program improves flexibility and strengthens the supporting muscles.
Home Remedies – Roll foot over golf or tennis ball, contrast baths

You can start treating plantar fasciitis right at home using simple DIY techniques like rolling your foot over a golf or tennis ball to massage the plantar fascia. Sitting down, cross your affected leg over the opposite knee and roll the ball under your foot for a few minutes daily. Contrast baths also help by alternating soaking your foot in warm and then cold water to improve blood flow. Gentle calf and foot stretches done several times a day keep the tissues flexible. Little adjustments make a difference.
Lifestyle Changes – Lose weight, wear supportive shoes, avoid bare feet
Making certain lifestyle adjustments can help offload the plantar fascia and avoid reinjury. If overweight, losing some excess pounds reduces strain on your feet. Choose shoes with good arch support and shock absorption. Avoid going barefoot and use a supportive insert like Copper Fit arch wraps. Limit activities that aggravate your symptoms like running. Take frequent sitting breaks if you have a standing occupation. Small changes that reduce pressure on your feet go a long way.
Medical Procedures – Steroid injections, shockwave therapy, surgery
For patients whose symptoms do not improve with conservative treatment, medical procedures like steroid injections, shockwave therapy, or surgery may be considered. Cortisone injections can temporarily reduce inflammation. Shockwave therapy uses sound waves to stimulate healing. Surgery to detach a portion of the plantar fascia is a last resort option and requires an extended recovery period. Thoroughly discuss risks and benefits of these advanced treatments with your doctor before proceeding.
Prevention – Warm up before exercise, rest feet, wear arch support
You can take proactive steps to help prevent plantar fasciitis episodes including warming up slowly before exercise, taking frequent foot rest breaks, and wearing arch supporting insoles or wraps. Gently stretching and massaging your calves and feet before activity allows the tissues to limber up. Regularly resting your feet while sitting avoids prolonged standing or walking. Devices like Copper Fit arch wraps provide compression and support to take pressure off your feet.
Outlook – Most cases resolve with conservative treatment in months

The outlook for plantar fasciitis is generally very favorable with most cases resolving fully within 6 to 18 months using conservative home therapies. Symptoms tend to gradually improve over time with rest, arch supports, stretching exercises, and avoiding reinjury. More severe or unresponsive cases may require advanced treatments like physical therapy, cortisone shots, or surgery as a last resort. Seeking care early on leads to the best results long-term.
Conclusion – Seek medical care for persistent symptoms, early treatment prevents chronic pain
Living with constant foot pain and limited mobility from plantar fasciitis is frustrating and depressing. But the good news is there are many effective ways to ease your discomfort both at home and through medical care. From simple stretches and over-the-counter aids like Copper Fit compression sleeves to customized orthotics and physical therapy, relief is within reach. Seeking care early at the first sign of symptoms helps prevent them from becoming a chronic issue. Don’t let heel and arch pain keep you sidelined – take control of your plantar fasciitis so you can get back on your feet!
Symptoms – Heel and arch pain that worsens after rest

If you’ve ever felt a sharp, stabbing pain in your heel or arch after getting out of bed in the morning or sitting for a prolonged period, you’re not alone. This common condition is known as plantar fasciitis, and it affects millions of people. The pain arises from microtears and inflammation in the plantar fascia – the thick band of tissue that runs along the bottom of your foot.
While plantar fasciitis can be agonizing, especially first thing in the morning, there are ways to find relief fast. With a few simple at-home treatments, you can often soothe pain and inflammation to get your feet feeling better.
Rest and Ice
One of the best initial treatments for plantar fasciitis pain is rest. Take a break from any high-impact activities like running or jumping that may be overtaxing your plantar fascia. An ice pack can also help decrease inflammation – try icing for 10-15 minutes a few times per day on the most painful area.
Foot Stretches
Certain foot stretches can gently lengthen the plantar fascia and calf muscles to reduce tension and strain. Sitting with one leg crossed over the other, gently pull your toes back toward your shin until you feel a stretch in your arch. Hold for 30 seconds and repeat on the other side. Do this stretch several times per day.
Massage
Massaging your foot can promote blood flow and relax tight muscles. Use your thumbs or a tennis ball to apply firm pressure and rub small circles along your arch and heel. Focus on any knots or trigger points where you feel pain. A few minutes of massage per day may significantly ease discomfort.
Over-the-Counter Orthotics
Visiting a podiatrist for custom orthotic inserts is ideal, but over-the-counter orthotics can also provide arch support and heel cushioning. Look for orthotics designed specifically for plantar fasciitis, like Copper Fit Ice Plantar Fasciitis Compression Sleeves. Wear them in shoes whenever you’re on your feet.
Night Splints
Night splints gently stretch your plantar fascia and Achilles tendon overnight while you sleep. This prevents tightening and morning pain. Models like the Copper Fit Plantar Fasciitis Arch Wrap wrap around the arch and foot to provide a sustained, gentle stretch.
Heel Cups and Pads

Over-the-counter silicone heel pads or cups cushion your heel and absorb shock with each step. Place them directly inside your shoes to prevent heel pain. Look for specialized heel pads like Copper Fit Plantar Fasciitis Arch Support Inserts to target plantar fasciitis.
Footwear Modifications
Wearing supportive shoes with good arch support is crucial for managing plantar fasciitis pain. Avoid flat shoes like flip flops, and opt for well-cushioned athletic shoes or shoes with built-in arch support. You can also insert orthotics into shoes that lack arch support.
Weight Loss
If you’re overweight, losing even a modest amount of weight can significantly relieve strain on your plantar fascia to reduce pain. Aim to reach a healthy weight through a balanced diet and regular exercise. Low-impact activities like swimming or cycling are ideal.
Calf Stretches

Tight calf muscles put extra tension on the plantar fascia, so stretching them is key. Standing facing a wall with hands forward, lunge one leg back while keeping the front knee straight. Hold for 30 seconds before switching legs. Do this several times per day.
Physical Therapy
Working with a physical therapist can be incredibly beneficial, especially if you have severe or chronic plantar fasciitis. They can design an exercise program to stretch your plantar fascia and strengthen your foot. Techniques like massage, ultrasound therapy, and taping may also provide pain relief.
While plantar fasciitis can be frustrating, these at-home treatments can often provide rapid relief from heel and arch pain. With a little rest, stretching, orthotics, and footwear adjustments, you’ll hopefully be back on your feet feeling fabulous in no time.
Causes – Tight calf muscles, high arches, excess weight, repetitive stress
If you’ve ever hobbled out of bed and felt like someone was stabbing you in the heel, you’ve experienced the excruciating pain of plantar fasciitis. While the exact cause is often unclear, there are several common contributing factors that put excessive strain on the plantar fascia ligament along the bottom of the foot.
Tight Calf Muscles
The calf muscles attach to the heel bone via the Achilles tendon. When the calf muscles are chronically tight and shortened, they pull excessively on the heel and put added tension on the plantar fascia. Gentle calf and Achilles stretches are key to relieving this tension.
High Arches
Those with high arches or overly rigid feet are more prone to plantar fasciitis pain. The arched shape and lack of shock absorption in the foot overly strains the plantar fascia. Arch supports, orthotics, and shoes with good cushioning can prevent excessive strain.
Excess Weight
Being overweight significantly increases stress on the plantar fascia with each step. Losing weight helps take pressure off the feet. Even a 10-15 pound weight reduction can make a noticeable difference in plantar fascia pain.
Repetitive Stress
Certain activities like long-distance running, dancing, or aerobics can cause repetitive microtrauma to the plantar fascia. Sudden increases in activity levels can trigger plantar fasciitis in athletes or those with active jobs. Rest and cross-training helps provide relief.
Flat Feet

Individuals with flat feet and low arches are at greater risk for plantar fasciitis. Their feet roll inward excessively while walking, overstretching the plantar fascia. Orthotics and arch support shoes help prevent overpronation and reduce strain.
Aging
As we get older, the tissues in our feet become less flexible. The fat pad on the heel also starts to thin out, resulting in less shock absorption. Using cushioned insoles and supportive footwear can help compensate.
Foot Mechanics
Certain foot mechanics like excess pronation (rolling in) or supination (rolling out) overload specific areas and lead to plantar fascia strain. Custom orthotics from a podiatrist can help correct these imbalances and redistribute pressure.
Weak Foot Muscles
The small muscles along the bottoms of the feet play a big role in stabilization. Weakness in these muscles causes more strain on the plantar fascia. Intrinsic foot exercises to strengthen the foot muscles help provide support.
Tight Achilles Tendon

Limited flexibility in the Achilles tendon negatively affects the ability of the ankle to move through its full range of motion. This puts more stress on the plantar fascia. Regular calf and Achilles stretching improves flexibility.
Genetics
Research shows some people may have genetically predisposed foot structures that increase risk for plantar fasciitis. These include high arches and excessive foot pronation. Wearing proper footwear can help mitigate risks.
Poor Footwear
Shoes that lack arch support, have thin soles, or provide poor shock absorption can overload the plantar fascia. Switch to well-cushioned athletic shoes or shoes with built-in arch support.
Occupation
Jobs that involve long periods of standing or walking on hard surfaces are associated with a higher incidence of plantar fasciitis due to repetitive strain on the feet. Anti-fatigue mats and supportive insoles can help.
In most cases, plantar fasciitis arises from multiple factors that all contribute to increased tension along the plantar fascia ligament. Identifying and addressing these causes through stretches, footwear changes, weight loss, and activity modifications can help get your feet feeling fabulous.
Risk Factors – Runners, overweight, jobs requiring standing, flat feet
Plantar fasciitis can strike anyone, but certain activities, occupations, and physical characteristics put you at greater risk. Understanding the risk factors allows early intervention to prevent heel and arch pain.
Runners
The repetitive pounding from running, especially on hard or uneven surfaces, commonly leads to plantar fasciitis in runners. Gradual training, good shoes, and strength exercises help prevent injury.
Overweight
Excess weight causes added stress and strain on the plantar fascia with each step. Losing weight helps reduce tension and pressure on the feet to relieve pain.
Jobs Requiring Prolonged Standing
Occupations that involve long hours of standing on hard floors – like factory workers, servers, retail clerks – have high plantar fasciitis rates. Anti-fatigue mats and supportive shoes are preventative.
Flat Feet
The stretched plantar fascia from pronated, flat feet are up to 15 times more likely to develop plantar fasciitis due to overextension. Arch supports and orthotics help avoid overstretching.
Age

Plantar fasciitis most commonly occurs between ages 40-60. The plantar fascia loses elasticity with age while protective foot fat pads also diminish.
Achilles Tendon Tightness
Limited ankle and Achilles flexibility increases strain on the plantar fascia with walking. Regular calf stretching aids full ankle range of motion.
Sudden Increases in Activity
Ramping up activity levels too quickly raises injury risk. Gradually increasing duration and intensity prevents overstressing the plantar fascia.
High Arches
The rigid, poorly shock-absorbing feet of those with high arches are more vulnerable to plantar fasciitis through excessive pulling on the plantar fascia.
Weak Foot Muscles
Plantar fasciitis frequently occurs when the small intrinsic muscles of the feet are weak. Strengthening exercises provide stability and support.
Improper Footwear
Shoes lacking arch support, cushioning, or shock absorption increase strain on the plantar fascia ligament.
Obesity

The extra weight carried by those who are obese causes excessive tension and stretching of the plantar fascia, especially during activities like walking and running.
Pregnancy
Hormonal changes and extra weight gained during pregnancy raise plantar fascia strain. Fascia stretching may also occur to accommodate pregnancy-related foot spreading.
Diabetes
Poor blood sugar control in diabetics negatively impacts connective tissues. The plantar fascia becomes less elastic and easier to tear.
Rheumatoid Arthritis
Inflammation from rheumatoid arthritis can cause thickening and weakening of the plantar fascia. Supportive footwear helps offload stress.
Foot Structure
Certain foot shapes like excessively flat or high arched feet increase plantar fascia tension and likelihood of injury.
Lead an Active Lifestyle
Highly active individuals like runners and dancers are vulnerable to plantar fasciitis from repetitive impact. Rest and cross-training provides relief.
Being aware of these common risk factors allows you to take preventative measures through arch supports, shoe choices, activity modifications and weight control to keep your feet feeling great.
Diagnosis – Physical exam, medical history, imaging tests
Plantar fasciitis can often be diagnosed based on symptoms alone, but your doctor may run tests to confirm and determine the exact cause of heel and arch pain.
Physical Exam
During a physical exam, your doctor will press and massage areas of your foot to pinpoint the location of pain. They’ll also assess your ankle and foot flexibility and evaluate your gait and posture to identify any abnormalities placing strain on your feet.
Medical History
Your doctor will ask about your medical history, including any past foot problems. They’ll want to know when the pain started, what activities aggravate it, and what treatments you’ve already tried. This comprehensive history helps guide treatment.
Foot X-rays
X-rays allow your doctor to visualize the structure of the foot and heel bone. They can assess alignment and look for fractures, bone spurs, arthritis or other issues that may be causing pain.
Ultrasound
Ultrasound uses soundwaves to create images of the plantar fascia. It can reveal areas of thickening, inflammation, tears or other abnormalities causing your symptoms.
MRI

An MRI scan provides a highly detailed view of the soft tissues of the foot. Your doctor may order one to confirm a partial plantar fascia tear or rule out other soft tissue problems behind your pain.
Nerve Tests
Sometimes heel pain actually arises from nerve dysfunction rather than the plantar fascia. Electromyography tests measure nerve conduction to identify any nerve issues.
Blood Tests
Your doctor may order blood tests to look for markers of inflammation or autoimmune diseases like rheumatoid arthritis that could contribute to plantar fasciitis.
Foot Examination
Your podiatrist will thoroughly examine your feet, looking closely at their structure, range of motion, and points of tenderness. They’ll evaluate your high/low arches, ankle flexibility, and gait.
Assessment of Activities
Your doctor will want to know about your exercise routines, occupation, and any activities that seem to aggravate your heel pain. Identifying strain-inducing actions is key.
Previous Injuries

Past foot, ankle or leg injuries can sometimes increase risk of plantar fasciitis. Your podiatrist will gather information on any prior injuries.
Response to Treatment
Your doctor will ask about any at-home treatments you’ve tried like stretching, ice, or OTC orthotics. This helps guide next steps.
While a physical exam and medical history are often sufficient to diagnose plantar fasciitis, additional testing can provide confirmation as well as valuable information on the exact cause of heel pain to optimize treatment.
Treatment – Rest, ice, OTC pain relievers, stretching, orthotics
Plantar fasciitis can be challenging to treat, but incorporating rest, ice, over-the-counter options, stretches, and orthotic devices often helps reduce heel and arch pain.
Rest
Scaling back activity levels to allow the inflamed plantar fascia to rest is vital, especially avoiding activities like running that exacerbate pain. Low-impact exercises like swimming can continue.
Ice
Applying ice packs to the most painful spot on the heel for 10-15 minutes several times per day helps decrease inflammation and foot pain.
OTC Pain Relievers
Anti-inflammatory over-the-counter medications like ibuprofen can temporarily alleviate plantar fasciitis pain and swelling. Use as directed.
Foot Stretches
Gently stretching the plantar fascia and Achilles tendon loosens tightness and relieves tension. Hold stretches like calf and arch stretches for 30 seconds.
Night Splints
Night splints keep the foot passively flexed overnight to prevent morning tightness. Models like the Copper Fit Plantar Fasciitis Arch Wrap help.
Orthotics
Inserts like Copper Fit Arch Support Insoles support the arch to offload tension on the plantar fascia.
Heel Pads

Heel pads and cups like Copper Fit Heel Protectors cushion the heel and absorb shock with each step.
Better Footwear
Wearing supportive athletic shoes with good arch support helps treat and prevent plantar fasciitis pain.
Lose Weight
Shedding excess weight through diet and exercise alleviates pressure on the feet and plantar fascia.
Physical Therapy
Working with a physical therapist can provide specialized stretching and strengthening exercises as well as other modalities to reduce pain.
Calf Raises
Doing calf raise exercises helps strengthen the calf and Achilles tendon to better support the arch.
Using a combination of at-home remedies, over-the-counter products, stretches, footwear changes, and activity modifications helps provide plantar fasciitis pain relief.
Braces & Wraps – Compression and support for the plantar fascia

Specialized braces and wraps provide effective relief from plantar fasciitis pain by delivering targeted compression and support to the inflamed plantar fascia ligament.
Night Splints
Night splints are worn while sleeping to provide a gentle, prolonged stretch to the plantar fascia and Achilles tendon. This prevents painful morning tightness. The Copper Fit Plantar Fasciitis Arch Wrap is an excellent option.
Compression Sleeves
Compression sleeves like the Copper Fit Ice Plantar Fasciitis Sleeves wrap around the arch and foot, increasing circulation and reducing inflammation.
Strapping Tape
Specialized kinesiology tape applied in a crossing pattern over the plantar fascia can help take tension off the tissue and improve mobility.
Arch Supports
Arch inserts like Copper Fit Arch Supports provide compression while supporting the foot’s arch to offload the plantar fascia.
Heel Lifts
Heel lifts fit inside the shoe to reduce strain on the plantar fascia by lifting and cushioning the heel. The Copper Fit Heel Protectors help.
Orthotics
Custom-made rigid orthotics from a podiatrist control overpronation and support the arch to prevent plantar fascia overstretching.
Taping
Specialized physical therapists can tape the foot in a way that supports the arch and takes tension off the plantar fascia.
Posterior Night Splints
These night splints keep the foot and ankle flexed downwards to gently and continuously stretch the calf and Achilles overnight.
Socks
Well-fitted plantar fasciitis socks with arch support also provide mild daytime compression to help reduce pain.
Using braces, wraps, splints and supports provides an easy, convenient way to support and offload the plantar fascia whether at home, work, or during activities to effectively alleviate heel pain.
Night Splints – Keep the foot flexed during sleep to stretch fascia

Night splints are a commonly recommended treatment for plantar fasciitis. Worn during sleep, they gently stretch and lengthen the plantar fascia to alleviate early morning heel pain.
How They Work
Night splints hold the foot in a gently flexed position overnight. This provides a prolonged, low-load stretch to the plantar fascia and Achilles tendon to relieve tightness. Reducing fascia tightness prevents first step heel pain.
Types of Night Splints
Dorsal night splints support the foot in a flexed position by keeping the toes and ankle pointing up. Other options include posterior splints that keep the foot bent downwards to stretch the Achilles and calf.
Benefits
Regular night splint use can help gradually lengthen tight plantar fascia tissues. This allows the foot to flatten more easily with weight bearing to relieve strain and heel pain.
Considerations
It takes consistent nightly use to see benefits. Some find night splints uncomfortable for sleeping. Low profile, cushioned options like the Copper Fit Plantar Fasciitis Arch Wrap increase comfort.
Who Should Use Them

Those with tightness or shrinking of the plantar fascia can benefit most from night splints. Patients with chronic, first step morning heel pain are ideal candidates.
Improved Mobility
Night splints gently stretch tightened tissues around the foot and ankle, gradually restoring mobility to these restricted joints.
Increased Flexibility
Keeping the plantar fascia elongated overnight prevents fascia shrinkage. Over time, flexibility increases allowing smoother foot flattening.
How to Wear Them
Clean and dry feet before applying splints. Start by wearing for just 1-2 hours before bed, then gradually increasing to all night as tolerated. Periodic re-adjustment may be needed.
Reduced Stiffness
Continuous stretching while sleeping minimizes morning stiffness and limping caused by tight plantar fascia and calf tissues.
Effective Stretching
Night splints provide a prolonged, gentle stretch not achievable with standard daytime stretching. This makes them highly effective at loosening tight plantar fascia.
Though awkward at first, nightly use of splints leads to marked improvement in morning heel pain by combatting plantar fascia tightness.
Physical Therapy – Stretches, strengthening exercises, massage
Working with a physical therapist can provide significant relief from plantar fasciitis pain through specialized stretches, strengthening, gait training, and hands-on techniques.
Stretches
Physical therapists teach stretches that target tight plantar fascia, calf, and hamstring tissues. Holding stretches for 30-60 seconds aids flexibility and arch mobility.
Strengthening Exercises
Exercises to strengthen weak foot and leg muscles are prescribed. Stronger muscles provide better support to prevent overloading the plantar fascia.
Massage
Manual soft tissue massage applied to the plantar fascia, arch, calf, and hamstrings helps improve blood flow and break up adhesions.
Gait Retraining
Abnormal walking patterns that strain the feet are corrected through gait retraining to prevent re-injury.
Taping
Specialized taping techniques support the foot arch and offload tension on the plantar fascia.
Pain Relief Modalities
Modalities like ultrasound, e-stim, and iontophoresis help reduce plantar fascia inflammation and discomfort.
Night Splint Instruction
Your physical therapist will demonstrate proper night splint positioning to provide effective overnight stretching.
Footwear Recommendations
They can provide specific shoe and insert suggestions tailored to your foot type and activities.
Activity Modification
Guidance is given on adjusting exercise routines to allow proper healing and prevent re-injury.
Home Exercise Program
You’ll be given a customized set of foot stretches and strengthening exercises to continue your progress at home.
A skilled physical therapist has many tools to alleviate plantar fasciitis pain and speed recovery. Hands-on PT is often the key to getting back on your feet pain-free.
Home Remedies – Roll foot over golf or tennis ball, contrast baths
Soothe Foot Pain Fast With These Simple Solutions:
If you’re suffering from aching, throbbing feet, you know just how debilitating foot pain can be. It can prevent you from standing for long periods, make walking uncomfortable, and generally zap your energy and vitality. While there are medical solutions for foot pain like plantar fasciitis, heel spurs, and arthritis, you may want to try some home remedies first. Often simple lifestyle changes, over-the-counter products, and do-it-yourself treatments can provide relief quickly and without the need for medications or costly specialist visits.
Here are 10 easy home remedies you can try to soothe foot pain fast:
1. Rest and Ice

One of the simplest yet most effective remedies is to stay off your feet as much as possible and ice the painful areas several times a day. Icing reduces inflammation and swelling to provide temporary pain relief. Try icing for 10-15 minutes a few times a day, especially after activities that aggravate your feet.
2. Contrast Baths
Alternating between hot and cold soaking can stimulate blood flow to your feet and ease muscular tension and soreness. Try soaking your feet in warm water for 3-4 minutes followed by 30 seconds in cold water. Repeat this cycle 3-5 times to get the benefits.
3. Massage
Massaging your feet increases circulation and relaxes tight muscles and connective tissue. Use your thumbs to apply firm pressure and rub in circles over the sole and arch of your foot. Stretch your foot by gently pulling each toe back and forth to loosen up the tissue. You can also use a tennis ball or roller under your foot to massage sore spots.
4. Strengthening Exercises
Simple foot exercises can stretch and strengthen the muscles, tendons and ligaments in your feet. Try exercises like toe points, toe spreads, ankle rolls and writing the alphabet with your toes. These will improve flexibility and support your arches.
5. Proper Footwear
Supportive, well-cushioned shoes are crucial for minimizing foot pain. Look for shoes with good arch support, shock absorption and a roomy toe box. Avoid high heels, flats and worn-out shoes. You may also benefit from custom orthotic inserts prescribed by a podiatrist.
6. Night Splint
Wearing a night splint keeps your foot stretched overnight to gently lengthen the plantar fascia and Achilles tendon and prevent morning stiffness. These splints are effective for plantar fasciitis and heel pain.
7. Over-the-Counter Pain Relievers
Anti-inflammatory medications like ibuprofen, naproxen and aspirin can temporarily reduce inflammation and discomfort associated with foot conditions like plantar fasciitis and arthritis. Use as directed for a short period for pain relief.
8. Apply Heat

Applying a heating pad, warm compress or taking a warm bath can improve blood circulation, relax muscles and temporarily diminish foot pain. Try using heat for 15-20 minutes a few times per day to relieve soreness and tension.
9. Roll a Ball Under Foot
Using a tennis ball, golf ball or other rubber ball to roll under your sore foot can massage tissue, stretch the plantar fascia and provide temporary relief. Focus on rolling over tender areas for a few minutes several times a day.
10. Epsom Salt Bath
Soaking your feet in a warm Epsom salt bath can reduce swelling, inflammation and foot pain. The magnesium in the salts helps relax muscles. Add 2 cups of Epsom salts to a foot bath and soak for 15-20 minutes as needed.
While home remedies don’t replace medical treatment for chronic foot problems, they can provide temporary relief and are worth trying before resorting to medications, injections or surgery. Be patient and give each remedy several tries before assessing its effectiveness. With some trial and error, you’re likely to find a DIY solution that brings you rapid relief.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
Don’t let foot pain slow you down. Try resting your feet, icing, massaging, stretching, supportive footwear, night splints, pain relievers, heat, and Epsom salt soaks to find the home remedies that offer you the most relief. With some TLC and experimentation, you can usually manage common foot problems like arthritis, tendinitis, heel spurs and plantar fasciitis at home without the need for medical intervention in many cases. Make your feet feel better fast with these do-it-yourself solutions!
Lifestyle Changes – Lose weight, wear supportive shoes, avoid bare feet

Soothe Foot Pain Fast With These Simple Solutions:
If you suffer from chronic foot pain, you know it can be debilitating and greatly impact your daily life. Conditions like plantar fasciitis, arthritis, tendinitis, and heel spurs can make every step agonizing. While there are many medical treatments available, making certain lifestyle changes can also help relieve foot pain and prevent it from getting worse.
Here are 10 lifestyle changes you can make to find relief from foot pain:
1. Lose Weight
If you are overweight or obese, losing even a modest amount of weight can significantly reduce stress and pressure on your feet. Every extra pound puts additional strain on your feet and contributes to problems like plantar fasciitis.
2. Wear Supportive Shoes
Ditch flimsy flats and shoes with little cushioning and support. Opt for well-made shoes with good arch support, shock absorption, and a roomy toe box. Proper footwear can alleviate pain associated with conditions like arthritis, heel spurs and tendinitis.
3. Stretch and Strengthen
Simple foot stretches and exercises to strengthen your feet can improve flexibility, circulation, and support. Try toe curls, toe spreads, calf raises, and using resistance bands. Also roll a tennis ball under your foot to massage sore spots.
4. Rest Your Feet
Make an effort to stay off your feet as much as possible when they are painful. Take breaks from standing and walking to allow the tissue in your feet to recover. Elevate your feet to reduce swelling.
5. Alternate Hot and Cold
An easy home remedy is to alternate soaking your feet in hot and cold water. The hot water improves blood flow while the cold water reduces inflammation and swelling. Repeat for 5-10 minutes for temporary relief.
6. Avoid Going Barefoot
Wear shoes, sandals or slippers as much as possible, even indoors. Going barefoot, especially on hard surfaces, can aggravate many common foot problems. The extra padding helps minimize impact and irritation.
7. Massage Your Feet

Gently massaging your feet can relax muscles, increase circulation, and temporarily reduce pain. Use your thumbs to work in small circles and apply pressure to tender spots. Stretch each toe back and forth too.
8. Over the Counter Pain Relievers
Medications like ibuprofen, aspirin and naproxen sodium can help relieve temporary foot pain and inflammation related to conditions such as arthritis and plantar fasciitis. Use as directed.
9. Night Splint
Wearing a night splint gently stretches your plantar fascia and Achilles tendon overnight. This prevents painful morning tightness associated with plantar fasciitis and heel spurs.
10. Lose the High Heels
Avoid regularly wearing high heels, which put extreme pressure on the balls of your feet and toes. Opt for low heels under 2 inches when possible. Give your feet a break from heels as often as you can.
Making lifestyle adjustments like losing weight, choosing proper shoes, resting your feet, and doing foot exercises and stretches can complement medical treatment for chronic foot problems. While not a cure, these changes can provide gradual, cumulative relief over time. Be patient and give each alteration a few weeks to take effect.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
Don’t just cope with painful feet – be proactive. Lose weight, wear proper footwear, massage, stretch, rest your feet, alternate hot and cold therapy, avoid going barefoot, and pop an OTC pain reliever to tame foot pain naturally. Along with professional treatment, simple lifestyle remedies can often provide soothing relief and help you get back on your feet!
Medical Procedures – Steroid injections, shockwave therapy, surgery

Soothe Foot Pain Fast With These Simple Solutions:
Ongoing foot pain from conditions like plantar fasciitis, arthritis, and heel spurs can be hard to resolve. While home remedies and lifestyle changes help some people, others need more aggressive medical treatment to find relief. Procedures like steroid injections, shockwave therapy, and surgery are options your doctor may recommend for stubborn foot pain.
Here are some common medical procedures to consider for relieving foot pain:
Cortisone Injections
Cortisone is a powerful steroid medication that decreases inflammation and pain. It can be injected directly into problem areas like the heel and ball of the foot. Cortisone shots may provide relief for several months at a time for conditions like plantar fasciitis.
Orthotics
Custom orthotic inserts fit inside your shoes to support the arch, improve alignment, and take pressure off areas like the heel. Prescribed by a podiatrist, orthotics can provide relief for pain caused by flat feet, plantar fasciitis, arthritis and more.
Extracorporeal Shockwave Therapy
This treatment uses sound waves directed at the heel or other areas to stimulate healing, decrease inflammation, and reduce pain associated with chronic conditions like plantar fasciitis. Several sessions may be needed initially.
Iontophoresis
A mild electrical current drives a corticosteroid medication into the tissue of the heel and foot. This method may be used to treat inflammatory conditions like plantar fasciitis when injections are not effective.
Physical Therapy
Specific foot exercises and stretches guided by a physical therapist can strengthen muscles, improve mobility, and reduce foot pain. Therapy may also include modalities like ultrasound, heat, ice and gentle massage.
Orthotic Devices
Night splints, boot casts, controlled motion walking boots and other devices can protect the foot, improve alignment, take pressure off the plantar fascia and promote healing. These are often used for plantar fasciitis and heel pain.
Nerve Blocks

Anesthetic medication can be injected around nerves in the foot to temporarily numb sensation and provide pain relief. This may help with pain from arthritis, neuromas and other neuropathic conditions.
Platelet-Rich Plasma (PRP) Injections
Concentrated platelets from your own blood are injected into the foot to stimulate healing and tissue regeneration. PRP shows promise for treating plantar fasciitis and arthritis pain.
Surgery
If more conservative treatments fail, surgery can repair or detach damaged tissue and bone spurs causing chronic foot pain. This includes procedures like plantar fascia release and heel spur removal.
Discuss the benefits and risks of medical procedures with your doctor to determine if they are appropriate for your type of foot pain. While not always warranted, they can provide lasting pain relief when other conservative measures fail. Some procedures like cortisone shots may be used in combination with at-home remedies, footwear changes and orthotics.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
Get long-lasting relief from foot pain. Explore medical procedures like steroid injections, shockwave therapy, orthotics, and surgery if home remedies aren’t providing sufficient relief. Under a doctor’s supervision, these options can help resolve persistent foot problems so you can get back on your feet pain-free.
Prevention – Warm up before exercise, rest feet, wear arch support
Soothe Foot Pain Fast With These Simple Solutions:
Persistent foot pain from conditions like plantar fasciitis, arthritis, and tendinitis can be frustrating. While there are many treatment options available, preventing foot problems before they start is ideal. With some simple preventative measures, you can help keep your feet pain-free.
Here are 10 tips to help prevent common foot pain:
1. Warm Up Before Exercise
Always warm up with 5-10 minutes of gentle walking or marching in place before engaging in vigorous exercise. This increases blood flow and prepares the muscles and tissue of the feet for activity, preventing injury.
2. Cool Down and Stretch After Exercise
Gently stretch your calves, ankles and feet after a workout when muscles are warm. Hold each stretch for 20-30 seconds. This prevents tightness and next-day soreness.
3. Wear Supportive Athletic Shoes
Ensure athletic and walking shoes have adequate cushioning, shock absorption and arch support. Replace shoes every 300-500 miles. Proper footwear prevents irritation and overuse injuries.
4. Cross Train
Vary your workouts and avoid repetitive stress on your feet. For example, alternate between walking and swimming instead of just walking daily. This reduces overuse strain.
5. Lose Excess Weight
Extra weight puts more pressure on your feet and can contribute to problems like plantar fasciitis. Even losing 10 pounds can make a big difference in preventing and relieving foot pain.
6. Rest Your Feet
Make sure to take regular breaks from standing and walking to allow your feet time to recover. Elevate your feet periodically throughout the day to promote circulation.
7. Avoid Going Barefoot
Wear supportive footwear as much as possible, especially on hard surfaces. The extra padding helps prevent irritation and overuse issues.
8. Stretch Your Feet
Perform stretches like pointing your toes up and down, curling your toes, and gently pulling each toe to maintain flexibility and range of motion in your feet.
9. Wear Orthotics or Arch Supports

Over-the-counter or custom orthotic inserts support your arches and evenly distribute weight through your feet. This prevents many problems.
10. Stay Hydrated
Drink plenty of water before, during and after exercise to keep your muscles and tissue hydrated. Dehydration can contribute to cramping and soreness.
Making some simple adjustments like wearing proper footwear, keeping your weight down, resting your feet, stretching and staying hydrated can go a long way towards keeping foot problems at bay. While not guaranteed to prevent all foot pain, these tips can reduce your risk significantly.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
Don’t take healthy feet for granted. Be proactive and make simple lifestyle changes to keep your feet in top shape. Preventing problems in the first place is much easier than trying to treat them after they develop. Take steps now to walk comfortably for miles and miles.
Outlook – Most cases resolve with conservative treatment in months
Soothe Foot Pain Fast With These Simple Solutions:
If you’re struggling with ongoing foot pain from conditions like plantar fasciitis, arthritis, tendinitis or heel spurs, you may feel discouraged about the prognosis. However, while these problems can be nagging, the outlook with conservative at-home care and medical treatment is generally positive.
Here’s an overview of what you can expect with common foot pain:
Plantar Fasciitis
With Plantar fasciitis, the outlook is usually good. About 80% of cases resolve within 10 months with conservative treatment like arch supports, stretching, icing and activity modification. Cortisone injections may provide temporary relief when needed. Surgery to detach the plantar fascia is a last resort.
Arthritis
There is no cure for arthritis, but prognosis is variable. Anti-inflammatory medications, shoe inserts, assistive devices, and sometimes surgery can effectively manage pain and retain mobility long-term. Losing weight also helps take pressure off arthritic joints.
Heel Spurs
Bone spurs themselves are not necessarily painful. The associated inflammation where they form causes discomfort. With stretching, orthotics, rest, icing and medication, pain often improves within several months. Surgery removes painful spurs only when other treatments fail.
Tendinitis
Cases of tendinitis generally resolve fully with rest, activity modification, shoe inserts, braces, icing, and anti-inflammatory medication. Physical therapy exercises can strengthen the tendons and prevent recurrence. Surgery repairs tears only when conservative treatment fails.
Neuromas
These benign nerve tumors cause pain between the toes. Custom orthotics relieve pressure and anti-inflammatory medication eases discomfort in many cases. Steroid injections provide temporary relief. Surgery removes the tumor if symptoms persist despite other treatments.
Stress Fractures
With rest, immobilization, and refraining from weight-bearing activity, stress fractures in the foot typically heal within 6-8 weeks. Surgery repairs serious fractures that do not mend properly with conservative treatment.
Hammertoes
Using toe spacers and customized shoe inserts can help straighten hammertoes and relieve discomfort in many cases. Surgery realigns the toe only if non-surgical options fail to provide adequate relief.
While the specific prognosis depends on the particular foot problem and its severity, most common conditions improve substantially within several months with conservative at-home care and non-invasive medical treatment. More aggressive options like surgery are usually a last resort.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet as part of a conservative treatment plan. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
While frustrating, most foot pain does not persist indefinitely. Have patience, work with your doctor, and try various conservative treatments to find the right combination that brings you relief. Consistency is key. With time, care and persistence, you can successfully manage your foot pain and get back on your feet.
Conclusion – Seek medical care for persistent symptoms, early treatment prevents chronic pain

Soothe Foot Pain Fast With These Simple Solutions:
If you’re dealing with ongoing foot discomfort, don’t assume you just have to live with it. There are many effective solutions to provide relief from common problems like plantar fasciitis, arthritis, heel spurs and tendinitis. While home remedies and lifestyle adjustments help some people, it’s important to see your doctor if symptoms persist.
Here are key takeaways on managing foot pain:
Proper Footwear is Crucial
Supportive, well-cushioned shoes with good arch support are vital for minimizing foot pain issues. Replacing worn-out athletic shoes regularly can prevent overuse injuries.
Lose Excess Weight
Extra weight strains your feet and can directly contribute to problems like plantar fasciitis. Even a modest weight loss of 5-10 pounds can make a noticeable difference.
Stretching is Important
Simple foot stretches to increase flexibility and range of motion, as well as calf and hamstring stretches can help prevent tightness that causes foot pain.
Rest is Key
Take breaks from prolonged standing and walking to allow overused tissue in the feet time to heal. Periodically elevate your feet above your heart to reduce swelling.
Alternate Hot and Cold
Rotating between soaking your feet in warm and cold water, or using heating pads and ice packs, can alleviate pain and swelling.
Medications Temporarily Relieve Pain
Over-the-counter non-steroidal anti-inflammatory drugs like ibuprofen can temporarily reduce discomfort and inflammation.
See Your Doctor for Severe or Persistent Pain
While home remedies help with mild pain, promptly consult a podiatrist or orthopedist if you have severe discomfort that lasts more than a week or two.
Ignoring chronic foot pain and failing to get medical care can lead to permanent mobility issues over time. But with early diagnosis and treatment, problems like plantar fasciitis often resolve without surgery.
Some over the counter products like copper fit ice plantar fasciitis compression sleeves, copper fit ice plantar fascia arch wraps, and copper fit plantar fasciitis compression foot sleeves can also help provide compression, support, and pain relief for aching feet as part of a conservative treatment plan. The copper infused fabric may also help improve circulation. Reviews indicate many people find these sleeves and wraps effective for reducing heel and arch pain from conditions like plantar fasciitis.
Don’t assume foot pain is just a normal part of aging or being active. With some diligence about proper footwear, exercise, weight, home treatment, and seeking medical care when needed, you can get back on your feet and live pain-free.

