How does SCAT5 help assess concussions on the sidelines. What are the key components of a sideline concussion evaluation. Why is standardized assessment crucial for concussion management. How can clinicians improve their sideline concussion assessment skills.
Understanding the Sport Concussion Assessment Tool 5 (SCAT5)
The Sport Concussion Assessment Tool 5 (SCAT5) is a standardized instrument used for evaluating concussions in athletes aged 13 years and older. Developed by experts in the field of sports medicine and neurology, SCAT5 provides a comprehensive approach to assessing potential concussions on the sidelines during sporting events.
SCAT5 is designed to be administered by healthcare professionals and includes several key components:
- Immediate on-field assessment
- Symptom evaluation
- Cognitive screening
- Neurological examination
- Balance testing
By utilizing SCAT5, medical professionals can make more informed decisions about an athlete’s condition and whether they should be removed from play for further evaluation.

The Challenges of Sideline Concussion Assessment
Assessing concussions on the sideline presents several unique challenges for healthcare providers. These include:
- Variable presentations of concussion symptoms
- Limited sensitivity and specificity of available assessment tools
- Time pressure in making decisions
- Evolving nature of concussion symptoms over time
- Reliance on athlete-reported symptoms
How can clinicians overcome these challenges? By using a standardized approach like SCAT5, combined with clinical experience and familiarity with the athlete, medical professionals can improve their ability to accurately assess and manage concussions in a high-pressure sideline environment.
Key Components of a Sideline Concussion Evaluation
A comprehensive sideline concussion evaluation should include the following components:
1. Initial Assessment for Serious Injuries
Before focusing on concussion symptoms, clinicians must first rule out more severe injuries such as:
- Cervical spine injuries
- Intracranial bleeding
- Other traumatic injuries that may present similarly to concussions
2. Symptom Assessment
Evaluating the athlete’s self-reported symptoms is crucial. SCAT5 includes a comprehensive symptom checklist that covers various physical, cognitive, and emotional symptoms commonly associated with concussions.
3. Neurological Examination
A brief neurological exam should assess:
- Cognitive function
- Cranial nerve function
- Balance and coordination
4. Cognitive Screening
SCAT5 incorporates cognitive tests that evaluate memory, concentration, and information processing speed. These tests can help identify subtle cognitive deficits that may not be immediately apparent.
5. Balance Testing
Assessing an athlete’s balance is an important component of concussion evaluation. SCAT5 includes the modified Balance Error Scoring System (BESS) to objectively measure balance performance.
The Importance of Baseline Testing in Concussion Management
Why is baseline testing valuable in concussion assessment? Baseline testing involves administering SCAT5 or other concussion assessment tools to athletes before the start of a sports season. This provides a point of comparison for post-injury evaluations, allowing clinicians to more accurately detect changes in an athlete’s cognitive function, balance, and symptom reporting.

Benefits of baseline testing include:
- Improved sensitivity in detecting concussion-related changes
- Personalized assessment based on the athlete’s normal functioning
- Enhanced ability to make return-to-play decisions
- Increased confidence in concussion management protocols
While baseline testing is not always feasible, it can significantly enhance the accuracy of sideline concussion assessments when available.
Emerging Technologies in Sideline Concussion Assessment
As research in concussion management advances, new tools and technologies are being developed to complement traditional assessment methods. Some promising emerging technologies include:
1. Visual Tracking Systems
These systems assess an athlete’s ability to track moving objects, which can be impaired following a concussion. How do visual tracking systems work? They typically use eye-tracking technology to measure smooth pursuit eye movements and saccades, providing objective data on visual-motor function.
2. Portable Neuroimaging Devices
While not yet widely available for sideline use, portable neuroimaging technologies such as functional near-infrared spectroscopy (fNIRS) show promise in detecting brain activity changes associated with concussions.

3. Vestibular-Ocular Motor Screening (VOMS)
VOMS assesses vestibular and ocular motor impairments commonly seen in concussions. This screening tool can provide valuable information about an athlete’s visual and balance systems.
While these emerging technologies show promise, it’s important to note that they should be used in conjunction with, not as a replacement for, established assessment tools like SCAT5 and clinical judgment.
Making Same-Day Return-to-Play Decisions
One of the most challenging aspects of sideline concussion management is deciding whether an athlete can safely return to play on the same day as a suspected concussion. Current consensus guidelines generally recommend against same-day return to play for athletes with diagnosed concussions.
Factors to consider when making return-to-play decisions include:
- Severity and duration of symptoms
- Results of neurocognitive testing
- Balance assessment outcomes
- The athlete’s concussion history
- The potential risk of further injury in the specific sport
When in doubt, it’s always safer to err on the side of caution and remove an athlete from play for further evaluation and monitoring.

The Role of Serial Assessments in Concussion Management
Why are serial assessments important in concussion management? Concussion symptoms can be dynamic and may evolve over time. Some athletes may not exhibit immediate signs or symptoms of a concussion, only to develop them hours or even days later.
Serial assessments involve repeating concussion evaluations at regular intervals following the initial injury. This approach offers several benefits:
- Detection of delayed-onset symptoms
- Monitoring of symptom progression or resolution
- Identification of subtle changes in cognitive function or balance
- Informed decision-making regarding return to play and academic accommodations
Healthcare providers should educate athletes, coaches, and parents about the importance of reporting any new or worsening symptoms that may develop after the initial assessment.
Improving Sideline Concussion Assessment Skills
How can healthcare providers enhance their ability to assess concussions on the sideline? Here are some strategies to improve sideline concussion assessment skills:

1. Familiarize Yourself with SCAT5
Practice administering SCAT5 regularly to become proficient in its use. This will help you conduct assessments more efficiently and accurately under pressure.
2. Stay Updated on Current Guidelines
Concussion management guidelines are continually evolving. Stay informed about the latest research and recommendations from leading sports medicine organizations.
3. Develop a Standardized Protocol
Create a consistent approach to sideline concussion assessment that can be implemented across your organization or team. This ensures all athletes receive the same level of care.
4. Practice Scenario-Based Training
Engage in simulated sideline assessments to improve your decision-making skills in high-pressure situations.
5. Collaborate with Other Healthcare Providers
Work closely with neurologists, neuropsychologists, and other specialists to enhance your understanding of concussion assessment and management.
6. Emphasize Athlete Education
Educate athletes about the importance of honest symptom reporting and the potential long-term consequences of playing through a concussion.
By implementing these strategies, healthcare providers can improve their ability to accurately assess and manage concussions on the sideline, ultimately ensuring better outcomes for athletes.
The Importance of Clinical Judgment in Concussion Assessment
While standardized assessment tools like SCAT5 are invaluable in concussion management, they should not replace clinical judgment. Experienced healthcare providers often develop an intuitive sense for when an athlete is “not right,” even if formal assessments appear normal.
Factors that contribute to effective clinical judgment in concussion assessment include:
- Familiarity with the individual athlete’s baseline behavior and performance
- Understanding of the specific sport and its associated risks
- Recognition of subtle changes in an athlete’s demeanor or behavior
- Ability to integrate multiple sources of information, including observation, testing results, and athlete reports
Healthcare providers should trust their instincts when something seems amiss, even if standardized assessments don’t indicate a clear problem. In these cases, it’s always better to err on the side of caution and remove the athlete from play for further evaluation.

By combining standardized assessment tools with clinical experience and judgment, healthcare providers can optimize their ability to identify and manage concussions effectively in the challenging sideline environment.
%PDF-1.4
%
170 0 obj
>>>
endobj
169 0 obj
>stream
2017-04-26T18:23:33+05:302021-11-09T15:18:07-08:002021-11-09T15:18:07-08:00Adobe InDesign CS6 (Windows)uuid:cef3549b-1dd1-11b2-0a00-88007826ccffxmp.did:B2C59A163194E611BD009A7CB80B8EC7xmp.id:652671407F2AE711B241A810463E44EFproof:pdfxmp.iid:642671407F2AE711B241A810463E44EFxmp.did:A56D12349EF5E61182DCE2D7A38F01F5xmp.did:B2C59A163194E611BD009A7CB80B8EC7default
application/pdfAdobe PDF Library 10.0.1False
endstream
endobj
15 0 obj
>
endobj
168 0 obj
>/ExtGState>/Font>/ProcSet[/PDF/Text/ImageC/ImageI]/Properties>/XObject>>>/Rotate 0/TrimBox[0.0 0.0 595.276 793.701]/Type/Page>>
endobj
1 0 obj
>/Font>/ProcSet[/PDF/Text]/Properties>/XObject>>>/Rotate 0/TrimBox[0.0 0.0 595.276 793.701]/Type/Page>>
endobj
27 0 obj
>/Font>/ProcSet[/PDF/Text]/Properties>/XObject>>>/Rotate 0/TrimBox[0.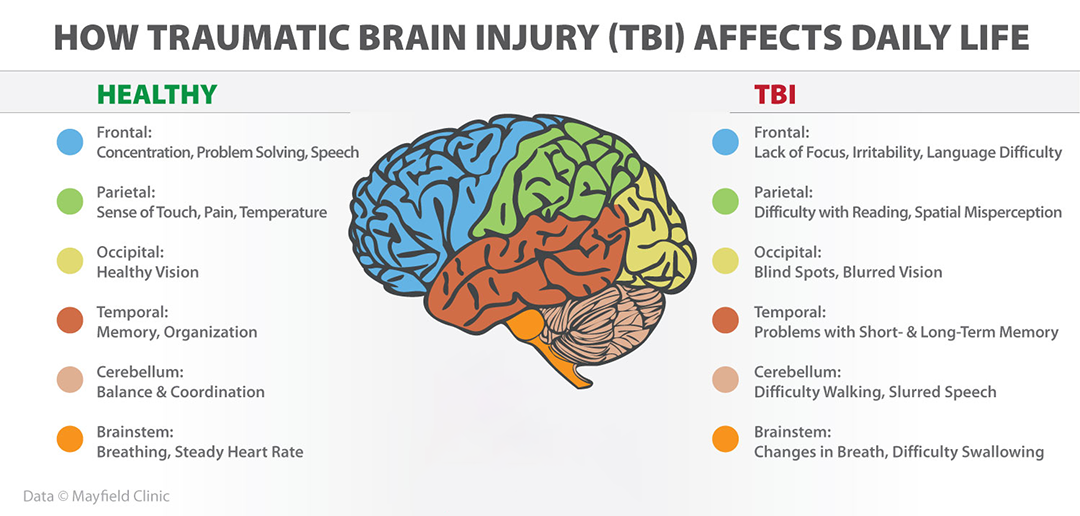 ϓJ>8>ttӹQWWwF~9z9>2
ϓJ>8>ttӹQWWwF~9z9>2
eKc7_5بKU&Ѡߏ~Rxqr:&߷jz8|y6RJUkjHR?NW]em3\+_Z[k=UrlZ,jU?W{MbϷ|+ufd*ni2VEZϏ>%!W)k|FS3x,3~]p
A View From the Sideline
Abstract
Context:
The sideline assessment of concussion is challenging, given its variable presentations, the limited sensitivity and specificity of sideline assessment tools, and how the presentation of the injury evolves over time. In addition, the diagnostic process, as well as the tools used to assess and manage concussion, continue to progress as research and what we know about concussion advance. This paper focuses on the initial assessment on the sideline by reviewing the concussion-evaluation literature, drawing from clinical experience to emphasize a standardized approach, and underscoring the importance of both familiarity with the athlete and clinical judgment.
Objective:
To review the evidence regarding the clinical assessment of sport-related concussion on the sideline. Additional considerations included making same-day return-to-play decisions, the sensitivity and specificity of sideline testing, and the importance of ongoing assessment and follow-up of injured athletes.
Data Sources:
I conducted a systematic literature review of the assessment of concussion on the sideline. The PubMed and MEDLINE databases were searched using the key term athletic injuries with concussion and mild traumatic brain injury. The search was refined by adding the key terms sideline assessment and on-field assessment. In addition, select additional position statements and guidelines on concussion were included in the review.
Results:
The PubMed search using athletic injuries and concussion as key terms produced 1492 results. Refining the search by sideline assessment and on-field assessment produced 29 and 35 results, respectively. When athletic injuries and traumatic brain injury were combined, 1912 results were identified. Refining the search by sideline assessment and on-field assessment led to 28 and 35 results, respectively. Only papers that were English-language titles, original work, and limited to human participants and included sideline assessments of sport-related concussion in athletes older than 13 years were considered for this discussion. A total of 96 papers were reviewed, including systematic reviews, consensus guidelines, and position statements.
A total of 96 papers were reviewed, including systematic reviews, consensus guidelines, and position statements.
Conclusions:
The sideline assessment of sport-related concussion is challenging given the elusiveness and variability of presentation, reliance on athlete-reported symptoms, and the varying specificity and sensitivity values of sideline assessment tools. In addition, the recognition of injury and assessment often occur in a time-pressured environment, requiring rapid disposition and decision making. Clinicians should begin the evaluation by assessing for cervical spine injury, intracranial bleeding, and other injuries that can present in a similar fashion or in addition to concussion. The sideline concussion evaluation should consist of a symptom assessment and a neurologic examination that addresses cognition (briefly), cranial nerve function, and balance. Emerging tools that assess visual tracking may provide additional information. The sensitivity and specificity of commonly implemented sideline assessment tools are generally good to very good, especially for symptom scores and cognitive evaluations performed within 48 hours of injury, and they are improved when a baseline evaluation is available for comparison. Serial assessments are often necessary as objective signs and symptoms may be delayed. A standardized assessment is paramount in evaluating the athlete with a suspected concussion, but there is no replacement for being familiar with the athlete and using clinical judgment when the athlete seems “not right” despite a “normal” sideline assessment. Ultimately, the clinician should err on the side of caution when making a return-to-play decision.
Serial assessments are often necessary as objective signs and symptoms may be delayed. A standardized assessment is paramount in evaluating the athlete with a suspected concussion, but there is no replacement for being familiar with the athlete and using clinical judgment when the athlete seems “not right” despite a “normal” sideline assessment. Ultimately, the clinician should err on the side of caution when making a return-to-play decision.
Key Words: traumatic brain injuries, assessment, return to play
Recognizing and assessing a player with a sport-related concussion (SRC) on the sideline of an athletic event is a challenging responsibility for the athletic trainer and sideline team physician. This often requires a rapid assessment in the midst of competition; the athlete is focused on returning to play and the clinician has a limited time to complete an evaluation and make disposition decisions. Given the importance of early recognition and removal of the concussed athlete from play, a standardized assessment should be practiced and perfected by the sideline health care clinician. As with much of the science of concussive injury, sideline assessment tools and techniques continue to evolve. Questions about the athlete’s orientation and short-term and remote memory are important parts of the initial sideline screen. The existing standardized sideline assessment tools, such as the Standardized Assessment of Concussion (SAC)1,2 and Sideline Concussion Assessment Tool (SCAT2, SCAT3, and child SCAT3),3–5 have been shown to be useful.6–9 The SCAT5,10 modified from SCAT3, was developed at the Fifth International Concussion in Sport Consensus Meeting11 and will likely prove to be useful. Emerging tools incorporating visual tracking12,13 and reaction time14 may provide additional beneficial information. Familiarity with the athlete can be instrumental in making a decision about return to or removal from play, as none of these tools, either alone or in combination, should take the place of clinical judgment.
As with much of the science of concussive injury, sideline assessment tools and techniques continue to evolve. Questions about the athlete’s orientation and short-term and remote memory are important parts of the initial sideline screen. The existing standardized sideline assessment tools, such as the Standardized Assessment of Concussion (SAC)1,2 and Sideline Concussion Assessment Tool (SCAT2, SCAT3, and child SCAT3),3–5 have been shown to be useful.6–9 The SCAT5,10 modified from SCAT3, was developed at the Fifth International Concussion in Sport Consensus Meeting11 and will likely prove to be useful. Emerging tools incorporating visual tracking12,13 and reaction time14 may provide additional beneficial information. Familiarity with the athlete can be instrumental in making a decision about return to or removal from play, as none of these tools, either alone or in combination, should take the place of clinical judgment.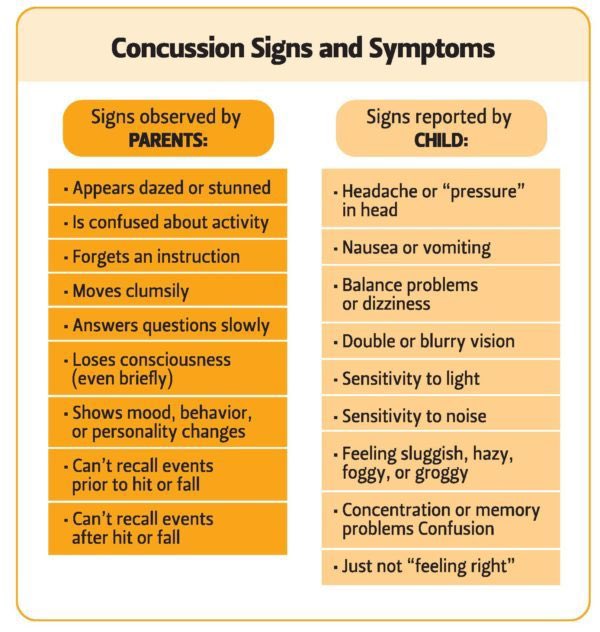 Rather, these tools should be combined with clinical judgment to make the diagnosis.
Rather, these tools should be combined with clinical judgment to make the diagnosis.
The objective of this paper, therefore, is to review the available evidence for the sideline assessment of concussion from the perspective of the health care provider: typically an athletic trainer, either with or without the team physician. It will address current knowledge, recent advances in sideline assessment tools, and the sensitivity and specificity of such tools where available. These findings will be discussed in relation to clinical experience, which ultimately yields a commonsense approach to evaluating an athlete with a concussion, erring on the side of caution, given the serious nature of this injury as well as its potential complications.
METHODS
For the review of literature, a PubMed search between 1968 and 2015 using athletic injuries and concussion as key words yielded 1492 results; using the same database with the key terms athletic injuries and traumatic brain injury instead generated 1912 results. Each search was filtered by adding the search terms sideline assessment and on-field assessment, resulting in 28 and 35 articles, respectively. Only papers that were English-language titles, original work, and limited to humans and included sideline assessments for SRC in athletes older than 13 years were considered. These along with systematic reviews, consensus guidelines, and position statements published since 2004 were reviewed and form the basis of this discussion.15–22
Each search was filtered by adding the search terms sideline assessment and on-field assessment, resulting in 28 and 35 articles, respectively. Only papers that were English-language titles, original work, and limited to humans and included sideline assessments for SRC in athletes older than 13 years were considered. These along with systematic reviews, consensus guidelines, and position statements published since 2004 were reviewed and form the basis of this discussion.15–22
RESULTS
Sideline assessment or on-field assessment refers to the acute evaluation of an injured athlete shortly after injury under a time limit or with the understanding that a disposition decision needs to be made in a time-constrained environment.23 For the purposes of this paper, I have divided the sideline assessment into an initial screening, signs and symptoms, cognitive function, balance assessment, combined tests, and additional tests. Where sideline assessments are combined tools (eg, the SCAT2 and SCAT3 are derived in part from the SAC, modified Balance Error Scoring System [m-BESS], and symptoms), information regarding the utility of these as combined or individual components are discussed.
Where sideline assessments are combined tools (eg, the SCAT2 and SCAT3 are derived in part from the SAC, modified Balance Error Scoring System [m-BESS], and symptoms), information regarding the utility of these as combined or individual components are discussed.
Initial Screening Assessment
At the time of a suspected injury, the provider begins the screening process by evaluating the athlete for cervical spine and more serious brain injury (such as intracranial hemorrhage or skull fracture) and implementing the emergency action plan.15,16,24 If the athlete is unconscious, he or she should be managed as if a coexisting catastrophic cervical spine or more serious brain injury is present. The player should not be moved, and manual in-line stabilization should be maintained to protect the cervical spine. If the athlete is responsive, the Glasgow Coma Scale (GCS) should be part of the initial screening assessment; although its reliability has been criticized, it can be useful in ruling out moderate to severe brain injury.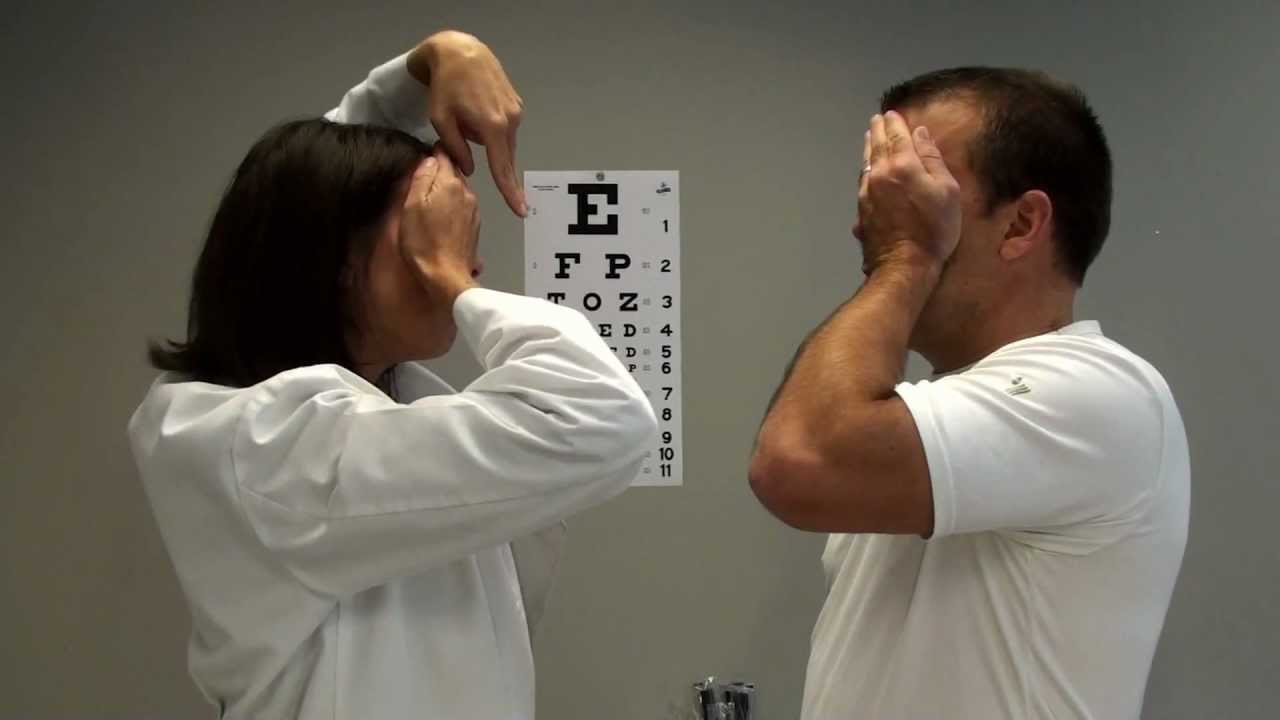 Observer agreement ranges from low to high, with κ indices ranging from 0.32 to 0.85.25,26 A recent review concluded that “findings using the scale have shown strong associations with those obtained by use of other early indices of severity and outcome.”27(p844)
Observer agreement ranges from low to high, with κ indices ranging from 0.32 to 0.85.25,26 A recent review concluded that “findings using the scale have shown strong associations with those obtained by use of other early indices of severity and outcome.”27(p844)
In the injured athlete who is not rendered unconscious, performing the initial screening assessment may be challenging, especially in sports that do not include play stoppages for medical assessments. Recently however, World Rugby28 and National Collegiate Athletic Association soccer29 guidelines were changed to allow a team to substitute for the injured player while he or she is being evaluated for concussion. The initial screening assessment should include questions that assess the athlete’s orientation and both immediate and remote memory. Asking the athlete what he or she remembers about the play before or after the injury can help the provider determine how the athlete is processing information. Inquiring about the day, date, month, and year can also be helpful. Asking for the venue name or location, the score, who scored last, the team’s last opponent, and the outcome of the game can easily be done on the sideline.30 This initial interaction between the health care provider and the athlete on the sideline is an important one and often indicates whether an athlete is concussed. If he is struggling to answer the questions or is clearly confused or having trouble with memory (or both), it may become obvious that he has sustained a concussion, even if subsequent sideline test results are “normal.” A complete evaluation should be subsequently performed whenever possible, even when it is clear that the athlete is concussed, as it may provide information regarding the severity of injury and prognosis. Evaluating for other or additional serious brain injury, as outlined by the Advanced Trauma Life Support guidelines,31 can be done by evaluating cranial nerve function, mental status, and other signs or symptoms ().
Inquiring about the day, date, month, and year can also be helpful. Asking for the venue name or location, the score, who scored last, the team’s last opponent, and the outcome of the game can easily be done on the sideline.30 This initial interaction between the health care provider and the athlete on the sideline is an important one and often indicates whether an athlete is concussed. If he is struggling to answer the questions or is clearly confused or having trouble with memory (or both), it may become obvious that he has sustained a concussion, even if subsequent sideline test results are “normal.” A complete evaluation should be subsequently performed whenever possible, even when it is clear that the athlete is concussed, as it may provide information regarding the severity of injury and prognosis. Evaluating for other or additional serious brain injury, as outlined by the Advanced Trauma Life Support guidelines,31 can be done by evaluating cranial nerve function, mental status, and other signs or symptoms (). 32 The management of other serious brain injuries, such as intracranial hemorrhage, cervical spine injury, or skull fracture, is beyond the scope of this review.
32 The management of other serious brain injuries, such as intracranial hemorrhage, cervical spine injury, or skull fracture, is beyond the scope of this review.
Table 1.
When to Refer an Athlete to an Emergency Facility for a Possible Concussiona
| Worsening or severe headache |
| Very drowsy or not easily awakened |
| Unable to recognize people or places |
| Significant nausea or vomiting |
| Behaves unusually or is unusually confused or irritable |
| Develops seizures |
| Develops weakness or numbness in arms or legs |
| Slurred speech or unsteady gait |
Signs and Symptoms
Several symptom scales are available to clinicians, but many have been put together without evaluation of psychometric properties33,34 or are modifications or derivatives of others, including the Post-Concussion Scale Revised,35 Head Injury Scale,36 Concussion Resolution Index,37 SCAT postconcussive symptom scale38 (also used in the SCAT2 and SCAT3),4,5 and Concussion Symptom Inventory.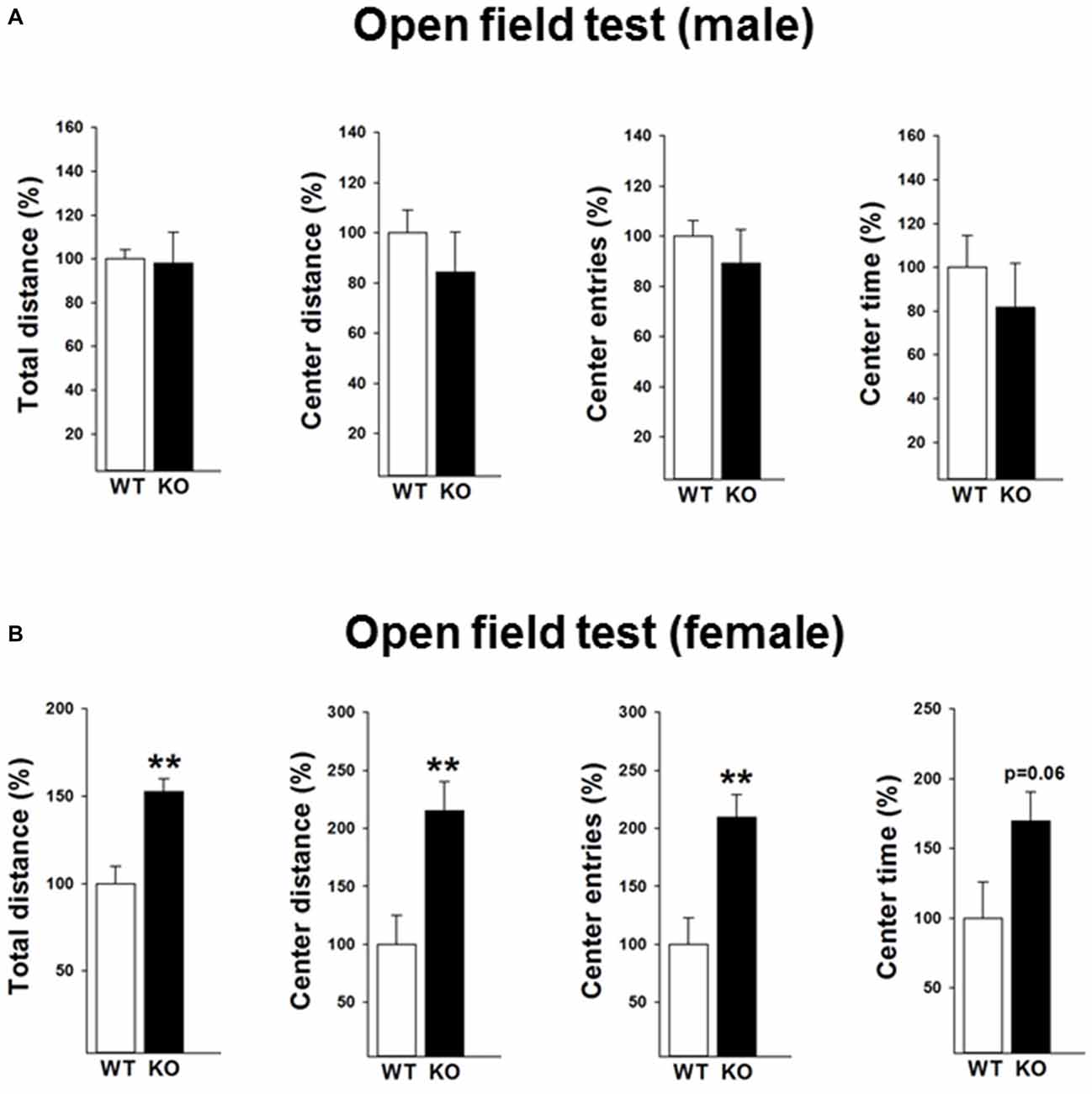 39 Concussion symptoms vary, and several groups19,40–44 have evaluated the capacity of symptom scales to accurately identify SRC. In general, the Graded Symptom Checklist or Post-Concussive Symptom Score accurately identifies SRC with a sensitivity of 64% to 89% and a specificity of 91% to 100%.35,36,45–51
39 Concussion symptoms vary, and several groups19,40–44 have evaluated the capacity of symptom scales to accurately identify SRC. In general, the Graded Symptom Checklist or Post-Concussive Symptom Score accurately identifies SRC with a sensitivity of 64% to 89% and a specificity of 91% to 100%.35,36,45–51
However, challenges arise when relying solely on symptoms during the evaluation process. Some athletes may have symptoms at baseline, or the reported symptoms may not be concussion specific. For example, despite not being injured, nearly 60% of collegiate varsity football, wrestling, and ice hockey athletes evaluated at baseline with the SCAT symptom scale reported symptoms, with mean scores of 3.52 for men and 6.39 for women.52 Sex differences in baseline symptom reports have also been noted for symptoms such as headache and emotional lability.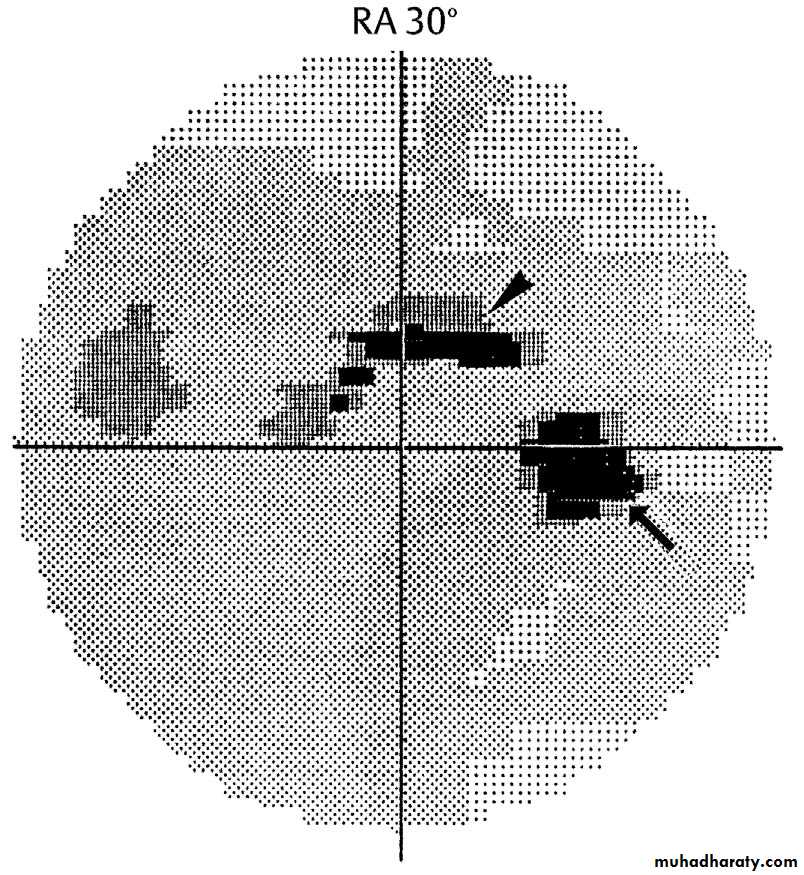 54 Concussion history has been cited as a modifying factor in baseline symptom reports: those with a history of concussion reported a larger number of symptoms than those without a history of concussion (5.25 versus 3.75, respectively).52 In that study, the most common baseline symptoms were fatigue and low energy (37%), drowsiness (23%), and neck pain (20%). A significant number of athletes also reported baseline symptoms of difficulty concentrating (18%) and difficulty remembering (18%).52 The differences in baseline symptoms between sexes as well as between athletes with or without a concussion history have been noted in other studies.54,55 Lastly, though the hallmark of concussion is confusion, other symptoms that occur frequently with concussion but are less specific include headache, dizziness, and drowsiness,19 which may also be associated with conditions such as febrile illness, cardiac disease, and heat illness ().
54 Concussion history has been cited as a modifying factor in baseline symptom reports: those with a history of concussion reported a larger number of symptoms than those without a history of concussion (5.25 versus 3.75, respectively).52 In that study, the most common baseline symptoms were fatigue and low energy (37%), drowsiness (23%), and neck pain (20%). A significant number of athletes also reported baseline symptoms of difficulty concentrating (18%) and difficulty remembering (18%).52 The differences in baseline symptoms between sexes as well as between athletes with or without a concussion history have been noted in other studies.54,55 Lastly, though the hallmark of concussion is confusion, other symptoms that occur frequently with concussion but are less specific include headache, dizziness, and drowsiness,19 which may also be associated with conditions such as febrile illness, cardiac disease, and heat illness ().
Table 2.
Examples of Signs and Symptoms Seen After Concussion (Acute and Delayed) in Athletesa
| Domain | |||
| Sleep | Affective | Somatic | Cognitive |
| Trouble falling asleep | Labile mood, increased emotionality | Headache (most common) | Confusion (hallmark of concussion) |
| Sleeping more than usual | Sadness | Dizziness | Disorientation |
| Sleeping less than usual | Fatigue | Balance dysfunction | Memory dysfunction (anterograde or retrograde amnesia or both) |
| Irritability | Nausea or vomiting or both | Loss of consciousness | |
| Anxiety | Visual complaints (double vision, blurry vision, photosensitivity) | Feeling “out of it,” “foggy,” “not right” | |
| Phonosensitivity | Vacant stare | ||
| Trouble focusing | |||
| Slow verbal or motor response or both | |||
| Incoherent or slurred speech | |||
| Excessive drowsiness | |||
When a provider evaluates an athlete for concussion on the sideline, interpreting the presence or absence of symptoms can be challenging, especially if no baseline is available, and when taking into account the lack of specificity of symptoms. This can be especially difficult during certain times of the year; for example, during the preseason, many athletes are practicing more than once per day, starting school, and participating in the heat. It is not unusual for athletes to be fatigued and have headaches and other symptoms that may or may not be related to concussion. The challenge is to try and decipher whether the symptoms are new and related to a blow to the head or body versus those that might be related to another process (eg, medical or emotional). In the sideline setting, it is again preferable to err on the side of caution and treat symptoms as concussion related until determined otherwise, removing the athlete from play for a more comprehensive evaluation.
This can be especially difficult during certain times of the year; for example, during the preseason, many athletes are practicing more than once per day, starting school, and participating in the heat. It is not unusual for athletes to be fatigued and have headaches and other symptoms that may or may not be related to concussion. The challenge is to try and decipher whether the symptoms are new and related to a blow to the head or body versus those that might be related to another process (eg, medical or emotional). In the sideline setting, it is again preferable to err on the side of caution and treat symptoms as concussion related until determined otherwise, removing the athlete from play for a more comprehensive evaluation.
Cognitive Tests
The SAC is a brief evaluation of cognitive function and includes standard questions of orientation (place, time, date, month, year), working memory via the immediate recall of 5 words, concentration by recalling a list of digits and the months backward, and remote memory via delayed recall. 1 The SAC has been useful in detecting SRC immediately after injury.1,8,46,56–59 In a large study31 of collegiate football players, the SAC score dropped, on average, 2.94 points below baseline (95% confidence interval = –4.39, –1.50) immediately after concussion and returned to baseline within 5 to 7 days. In another investigation of collegiate athletes,56 the sensitivity of the SAC was 95%, with a specificity of 76% in accurately diagnosing concussion immediately after injury, and significant improvements in SAC scores 48 hours after injury. Both practice and ceiling effects may occur on the SAC, so although immediate postinjury use is recommended, its ability to differentiate concussed from nonconcussed athletes is limited if used more than 48 hours after injury.1,46,59 Similar to evaluating symptoms on the sideline, interpreting the SAC in an athlete who lacks a baseline result can be challenging.
1 The SAC has been useful in detecting SRC immediately after injury.1,8,46,56–59 In a large study31 of collegiate football players, the SAC score dropped, on average, 2.94 points below baseline (95% confidence interval = –4.39, –1.50) immediately after concussion and returned to baseline within 5 to 7 days. In another investigation of collegiate athletes,56 the sensitivity of the SAC was 95%, with a specificity of 76% in accurately diagnosing concussion immediately after injury, and significant improvements in SAC scores 48 hours after injury. Both practice and ceiling effects may occur on the SAC, so although immediate postinjury use is recommended, its ability to differentiate concussed from nonconcussed athletes is limited if used more than 48 hours after injury.1,46,59 Similar to evaluating symptoms on the sideline, interpreting the SAC in an athlete who lacks a baseline result can be challenging. If available, group-based norms for athletes (eg, other athletes of the same age, sex, or sport at the same school or in the same league) may be useful. The SAC does not take the place of clinical judgment, and the results should be used as supportive information for the clinical assessment, especially when no baseline is available.
If available, group-based norms for athletes (eg, other athletes of the same age, sex, or sport at the same school or in the same league) may be useful. The SAC does not take the place of clinical judgment, and the results should be used as supportive information for the clinical assessment, especially when no baseline is available.
Balance Assessment
The utility of balance testing in evaluating concussive injury, with deficits returning to baseline within 3 to 7 days, has been well demonstrated.6,60–63 Swaying or falling and being unable to maintain balance after injury are common symptoms after concussion and are often worsened with eyes closed, due to the loss of vision as a reference for where one stands in space.6,60–63 Given the utility of balance in assessing SRC, the m-BESS was included in the SCAT2 assessment.3 This assessment consists of 3 stances: feet together, 1-legged stance, and tandem stance with the eyes closed. Each stance is to be held for 20 seconds, and the errors for each are counted. The complete BESS consists of these 3 stances plus 3 additional trials using a foam surface and is more sensitive than the modified version,60–63 which prompted its inclusion in the SCAT3.4 Even so, balance testing is limited by the effects of fatigue and exercise, practice effects with serial assessments, and concerns regarding reliability.43,63–65 The sensitivity of balance testing was highest within 24 hours of injury (0.34), and specificity on days 1 through 7 after injury was between 0.91 and 0.96.45 Completing the BESS on the sideline and interpreting the results can sometimes be a challenge, especially if no baseline evaluation is available. The timing of this complete assessment may need to be modified, such that it is performed at half time or in the locker room after the practice or game. Despite the low sensitivity of balance testing in isolation, the high specificity achieved by combining balance testing with other assessments justifies its use in the sideline evaluation of athletes with concussion.
Each stance is to be held for 20 seconds, and the errors for each are counted. The complete BESS consists of these 3 stances plus 3 additional trials using a foam surface and is more sensitive than the modified version,60–63 which prompted its inclusion in the SCAT3.4 Even so, balance testing is limited by the effects of fatigue and exercise, practice effects with serial assessments, and concerns regarding reliability.43,63–65 The sensitivity of balance testing was highest within 24 hours of injury (0.34), and specificity on days 1 through 7 after injury was between 0.91 and 0.96.45 Completing the BESS on the sideline and interpreting the results can sometimes be a challenge, especially if no baseline evaluation is available. The timing of this complete assessment may need to be modified, such that it is performed at half time or in the locker room after the practice or game. Despite the low sensitivity of balance testing in isolation, the high specificity achieved by combining balance testing with other assessments justifies its use in the sideline evaluation of athletes with concussion.
Combined Tests
The SCAT2 was developed in 2008 by the International Concussion in Sport (CIS) group3 and included an assessment of signs and symptoms (ie, Graded Symptom Checklist), cognitive function (ie, SAC), the Maddock questions, and balance (ie, m-BESS) as well as the GCS, a signs score (loss of consciousness and balance dysfunction), and a coordination examination (finger to nose). The maximum score is 100, with 22 points for no symptoms, 30 points for a perfect SAC, 30 points for no errors on the m-BESS, 2 points for no loss of consciousness or balance dysfunction, 15 points for a normal GCS, and 1 point for normal coordination. The National Football League later modified the SCAT2 for use in professional American football and incorporated additional “no-go” criteria that highlight when immediate removal from play or screening for cervical spine and more serious brain injury is indicated.19 The SCAT3 was developed in 2012 by the CIS group.4 The SCAT3 kept the main subcomponents of the SCAT2 (Graded Symptom Checklist, SAC, Maddocks questions, and GCS) but incorporated subtle differences: allowing a test of tandem gait as an “and/or” option with the full BESS, changing the order of assessments, abandoning the scoring system, moving the signs of loss of consciousness and balance dysfunction to a separate section in order to identify signs that would lead to immediate removal from play, and adding a cervical spine evaluation. Simultaneously, for children ages 5 to 12 years, the CIS group created the child SCAT, despite recognizing that minimal data thus far exist for its components.5 Even with the integration of objective measures, the National Football League and SCAT2 and SCAT3 assessments emphasize the clinician’s judgment; knowing the athlete and often the subtleties of his or her personality may lead to a diagnosis of concussion despite “normal” performance on these standardized assessments. Indeed, the clinician’s judgment remains the criterion standard for concussion diagnosis, and as such, if there is evidence for or suspicion of concussive injury, the athlete should be removed from play and followed serially to monitor both deterioration and the development of new signs or symptoms of injury.
Simultaneously, for children ages 5 to 12 years, the CIS group created the child SCAT, despite recognizing that minimal data thus far exist for its components.5 Even with the integration of objective measures, the National Football League and SCAT2 and SCAT3 assessments emphasize the clinician’s judgment; knowing the athlete and often the subtleties of his or her personality may lead to a diagnosis of concussion despite “normal” performance on these standardized assessments. Indeed, the clinician’s judgment remains the criterion standard for concussion diagnosis, and as such, if there is evidence for or suspicion of concussive injury, the athlete should be removed from play and followed serially to monitor both deterioration and the development of new signs or symptoms of injury.
A prospective study46 evaluating concussion in collegiate athletes using baseline measures of symptoms, cognitive function, and postural stability (ie, BESS) immediately after injury and serially up to 90 days postinjury showed increases in symptoms and errors on the BESS and decreased cognitive function immediately after injury, with gradual resolution over 7 days. The utility of a multimodal assessment and comparison of the individual postinjury evaluations with each person’s unique baseline were also demonstrated.
The utility of a multimodal assessment and comparison of the individual postinjury evaluations with each person’s unique baseline were also demonstrated.
As discussed previously, many factors influence symptom reports and performance on cognitive and balance testing. These factors, which include sex, concussion history, acute fatigue, physical illness, and orthopaedic injury, are discussed in detail elsewhere.*
A limited number of studies8,52,68–70 using the SCAT2 established individual differences in baseline assessments, and only a single study8 has evaluated the sensitivity and specificity of the SCAT2 for identifying concussion. In this prospective research on collegiate male and female varsity athletes, the SCAT2 was administered at baseline and repeated if a concussive injury occurred. Contact-sport athletes who had not sustained concussions (control group) repeated the SCAT2 to match the experimental group’s timeframe postinjury. When a baseline assessment was available, the SCAT2 had a sensitivity of 96% and a specificity of 84%.8 If no baseline was available, 83% sensitivity and 91% specificity were obtained by using a cutoff value of 74.5 out of a possible maximum score of 100. This study demonstrated the utility of the SCAT2, and therefore the SCAT3, in the assessment of SRC in collegiate athletes. Postinjury, significant changes were noted for the symptom score and m-BESS. Although the SAC score of the concussed athletes did not change after injury from their baseline score, when compared with the control group, who showed an improvement in their repeat test versus their baseline, the difference was significant. This underscores that the lack of improvement in the concussed group suggests concussive injury and the lack of a practice effect, which has been discussed previously.5 In addition, this prospective study of the SCAT2 in collegiate athletes did not demonstrate a sex difference in baseline performance, nor did it demonstrate a difference in baseline scores for athletes with a history of concussion or other modifiers such as a history of migraines or headaches, depression, anxiety, or learning disability.
When a baseline assessment was available, the SCAT2 had a sensitivity of 96% and a specificity of 84%.8 If no baseline was available, 83% sensitivity and 91% specificity were obtained by using a cutoff value of 74.5 out of a possible maximum score of 100. This study demonstrated the utility of the SCAT2, and therefore the SCAT3, in the assessment of SRC in collegiate athletes. Postinjury, significant changes were noted for the symptom score and m-BESS. Although the SAC score of the concussed athletes did not change after injury from their baseline score, when compared with the control group, who showed an improvement in their repeat test versus their baseline, the difference was significant. This underscores that the lack of improvement in the concussed group suggests concussive injury and the lack of a practice effect, which has been discussed previously.5 In addition, this prospective study of the SCAT2 in collegiate athletes did not demonstrate a sex difference in baseline performance, nor did it demonstrate a difference in baseline scores for athletes with a history of concussion or other modifiers such as a history of migraines or headaches, depression, anxiety, or learning disability. 8
8
In a similar prospective study evaluating the SCAT3 in high school and collegiate athletes at baseline and after concussion (published after the initial PubMed search for this article was conducted), Chin et al71 identified similar findings related to the utility of a standardized sideline assessment of concussion. Female sex, high school level of competition (versus college), and attention-deficit/hyperactivity disorder were associated with higher baseline symptom ratings. Male sex, attention-deficit/hyperactivity disorder, and learning disability were associated with lower baseline SAC scores. Male sex, high school level of competition, attention-deficit/hyperactivity disorder, and learning disability were associated with poorer baseline BESS performance. After concussive injury, the symptom score showed the largest effect size at the 24-hour assessment. Effect sizes for the SAC and BESS were small to moderate at 24 hours and nonsignificant at days 8 and 15. 71 This study confirms the utility of a standardized assessment that combines several tools, such as the SCAT2 or SCAT3, in evaluating athletes with SRC.
71 This study confirms the utility of a standardized assessment that combines several tools, such as the SCAT2 or SCAT3, in evaluating athletes with SRC.
As with each component of the SCAT2 or SCAT3, when no baseline evaluation is available, it is challenging to determine if an athlete’s sideline performance represents a decline. Given the findings of the studies referenced earlier, using published normative data can help, but ultimately it is often the clinician’s assessment of an athlete’s responses and behaviors that determines whether a concussive injury has occurred. As unappealing as it may be for the scientific community to admit, the sideline assessment and diagnosis of concussion are often more art than science, with no clear biomarker currently available for this injury.
Additional Tests
New to the concussion-assessment field are tools that evaluate saccadic eye movements in individuals who may be concussed. The utility of 1 such test has been explored in mixed martial arts athletes, youth and collegiate athletes, and professional hockey players and holds promise in assessing concussive injury. 12,13,72–75 Specifically, the King-Devick (KD) test uses numbers placed in a standardized fashion, spaced at varying intervals on 3 cards. The athlete is timed as he or she reads off the numbers from each card over 1 to 2 minutes. Research12,13,73–75 on the KD test has demonstrated that visual-scanning ability decreases (ie, takes longer) after concussion. As with other sideline assessment tools, the KD test is also associated with a practice effect in nonconcussed controls, whereby they perform better after having been exposed to it.13,73 This underscores the importance of having either specific individual baseline scores or group-based norms (or both) available for comparison if using this test on the sideline.
12,13,72–75 Specifically, the King-Devick (KD) test uses numbers placed in a standardized fashion, spaced at varying intervals on 3 cards. The athlete is timed as he or she reads off the numbers from each card over 1 to 2 minutes. Research12,13,73–75 on the KD test has demonstrated that visual-scanning ability decreases (ie, takes longer) after concussion. As with other sideline assessment tools, the KD test is also associated with a practice effect in nonconcussed controls, whereby they perform better after having been exposed to it.13,73 This underscores the importance of having either specific individual baseline scores or group-based norms (or both) available for comparison if using this test on the sideline.
A few investigators have compared more common sideline assessments with the KD test. One preliminary study13 demonstrated that the KD test may be more useful than the SAC immediately postinjury. In this prospective study of youth and collegiate ice hockey and lacrosse players, the KD test was used along with the SAC and a timed gait analysis at baseline and after concussion, with nonconcussed athletes as controls. When receiver operating curves from regression models were used to compare changes between the postinjury and baseline assessments, the KD test had a value of 0.92 versus 0.87 for the tandem gait and 0.68 for the SAC.13
In this prospective study of youth and collegiate ice hockey and lacrosse players, the KD test was used along with the SAC and a timed gait analysis at baseline and after concussion, with nonconcussed athletes as controls. When receiver operating curves from regression models were used to compare changes between the postinjury and baseline assessments, the KD test had a value of 0.92 versus 0.87 for the tandem gait and 0.68 for the SAC.13
In another prospective study76 of emergency room patients, the KD test was used along with the SCAT2 to evaluate patients with mild traumatic brain injury (mTBI) compared with control patients who had acute ankle injuries. The mTBI patients differed from controls on components of the SCAT2, including the symptom score (Cohen d = 1.02–1.15, P < .001) and SAC (d = 0.81, P = .0004) but not on the KD test (d = 0.40, P = .148). In logistic regression analysis, the KD test did not contribute more than these 2 measures in predicting group membership (mTBI versus control, P = . 1991).76 This study had limitations in that it was not restricted to patients with SRC; patients with mTBI from other mechanisms were included, as well as a broad age range. More research is necessary to determine how long these deficits persist, how they correlate with other measures of function, and the multitude of factors that may affect how these tests are implemented in the assessment of SRC.12,13,72–75
1991).76 This study had limitations in that it was not restricted to patients with SRC; patients with mTBI from other mechanisms were included, as well as a broad age range. More research is necessary to determine how long these deficits persist, how they correlate with other measures of function, and the multitude of factors that may affect how these tests are implemented in the assessment of SRC.12,13,72–75
Another novel area of concussion assessment is measurement of reaction time. Although sideline challenges exist, a measuring stick attached to a hockey puck has been used to measure reaction time; performance is based on how quickly and where the athlete grasps the stick when it is dropped.14 In a study of collegiate athletes, reaction time differentiated concussed from nonconcussed athletes, with a significant decline in postinjury versus baseline time in the concussed group compared with a trend toward improvement in the nonconcussed group. 14 The sensitivity and specificity of the reaction-time test were 75% and 68%, respectively, with a reliable change index of 65%.14 The reaction-time test has also been shown to remain stable during acute exercise77 and provide acceptable reliability.78 Additional investigations of the sideline reaction-time test to evaluate concussion are needed.
14 The sensitivity and specificity of the reaction-time test were 75% and 68%, respectively, with a reliable change index of 65%.14 The reaction-time test has also been shown to remain stable during acute exercise77 and provide acceptable reliability.78 Additional investigations of the sideline reaction-time test to evaluate concussion are needed.
Challenges for the Sideline Clinician
The sideline clinician should be confident in erring on the side of safety: that is, pulling an athlete out when no concussion is present is a better scenario than allowing a concussed athlete to continue based on a negative or normal standardized sideline test score. Allowing an athlete with a concussion to return to play if the symptoms were mild or had resolved and were not exacerbated by exertion was accepted clinical practice before 2006.38,79–81 Since that time, however, the pendulum has swung toward a philosophy of no return to play in the same game or on the same day, given that concussion can be a subtle injury and many athletes who are initially asymptomatic develop signs and symptoms in the first 24 hours. 46,82,83 The National Collegiate Athletic Association84 instituted a no-return-to-play-on-the-same-day policy in 2010, and many international organizations and professional sports now have similar policies.85–90 This shift in policy is supported by a study91 of collegiate football players that identified delayed onset of symptoms in 33% of those with a suspected concussion who returned to the same game compared with only 12.6% of players who did not return.
46,82,83 The National Collegiate Athletic Association84 instituted a no-return-to-play-on-the-same-day policy in 2010, and many international organizations and professional sports now have similar policies.85–90 This shift in policy is supported by a study91 of collegiate football players that identified delayed onset of symptoms in 33% of those with a suspected concussion who returned to the same game compared with only 12.6% of players who did not return.
Similar to policy changes among sporting organizations, legislation affecting youth athletes began in Washington with the Lystedt law, which mandates removal from play and no return to the same game of athletes younger than 18 years old with any signs or symptoms of concussion.92 Legislation similar to the Lystedt law now exists in each of the 50 United States and Washington, DC, and is under consideration in Canada.
A Common-Sense Approach
If an athlete has sustained a blow to the head and the athletic trainer and team physician (if available) find the athlete does not demonstrate any signs or endorse any symptoms of concussion and the cognitive, balance, and neurologic examinations are normal, then he or she can be returned to play (ie, a concussion is not suspected). In these situations, strong consideration for serial assessments to follow the athlete will enhance player safety. It is also clear that, in some cases, an athlete appears dazed or “out of it,” answers questions a bit more slowly than expected, or appears to process information more slowly or displays an unusual affect, and yet completes the sideline assessment without errors. The athletic trainer and team physician should keep the athlete out of play because of the clinical assessment of a suspected concussion. In other words, the clinical assessment and intuition of the sideline clinician remain the criterion standard and should take precedence over how an athlete performs on sideline testing. If signs or symptoms indicate cervical spine injury, intracranial bleeding, or skull fracture, the emergency action plan is initiated and the athlete transported to an emergency facility. Robust public outreach efforts by the Centers for Disease Control and Prevention and the CIS Group (Pocket Concussion Recognition Tool93) to nonmedically trained individuals, including athletes, parents, and coaches, as well as to health care providers have provided education regarding concussion signs and symptoms that emphasizes the importance of recognition and removal from play.94 Lastly, if no athletic trainer or other qualified health care provider is available and the athlete presents with signs or symptoms of concussion, he or she should be removed from play and not allowed to return until evaluated by a health care provider, even if symptoms resolve.
If signs or symptoms indicate cervical spine injury, intracranial bleeding, or skull fracture, the emergency action plan is initiated and the athlete transported to an emergency facility. Robust public outreach efforts by the Centers for Disease Control and Prevention and the CIS Group (Pocket Concussion Recognition Tool93) to nonmedically trained individuals, including athletes, parents, and coaches, as well as to health care providers have provided education regarding concussion signs and symptoms that emphasizes the importance of recognition and removal from play.94 Lastly, if no athletic trainer or other qualified health care provider is available and the athlete presents with signs or symptoms of concussion, he or she should be removed from play and not allowed to return until evaluated by a health care provider, even if symptoms resolve.
Role of Head-Impact Sensors in Detecting Concussive Injury
Given the challenge of providing athletic trainer coverage for all sport activities at every level of competition, a market has developed for additional methods of injury recognition, including products that evaluate the possibility of concussive injury by measuring head-impact forces, despite the lack of correlation between absolute impact magnitude and likelihood of concussive injury. To date, the threshold for concussive injury is unknown, and it is likely to be different for each person.95–100 American football players were concussed by impacts to the head that occurred over a wide range of magnitudes (60.51g to 168.71g linear acceleration), and clinical measures of acute symptom severity, balance, and neuropsychological function all appeared to be largely independent of linear impact magnitude and location.97 Further, clinical outcomes of symptoms, balance, or neuropsychological performance were not related to impact magnitude or location, and the athletes with concussions sustained as a result of lower magnitudes (<70g) tended to present with just as many clinical deficits as those from higher magnitudes (>110g). Thus, despite the literature suggesting that large magnitudes of head impact, particularly with high angular acceleration, resulted in more serious clinical outcomes in cases of moderate or severe traumatic brain injury,84,85 the magnitude and location of impact may not predict clinical outcomes.
To date, the threshold for concussive injury is unknown, and it is likely to be different for each person.95–100 American football players were concussed by impacts to the head that occurred over a wide range of magnitudes (60.51g to 168.71g linear acceleration), and clinical measures of acute symptom severity, balance, and neuropsychological function all appeared to be largely independent of linear impact magnitude and location.97 Further, clinical outcomes of symptoms, balance, or neuropsychological performance were not related to impact magnitude or location, and the athletes with concussions sustained as a result of lower magnitudes (<70g) tended to present with just as many clinical deficits as those from higher magnitudes (>110g). Thus, despite the literature suggesting that large magnitudes of head impact, particularly with high angular acceleration, resulted in more serious clinical outcomes in cases of moderate or severe traumatic brain injury,84,85 the magnitude and location of impact may not predict clinical outcomes.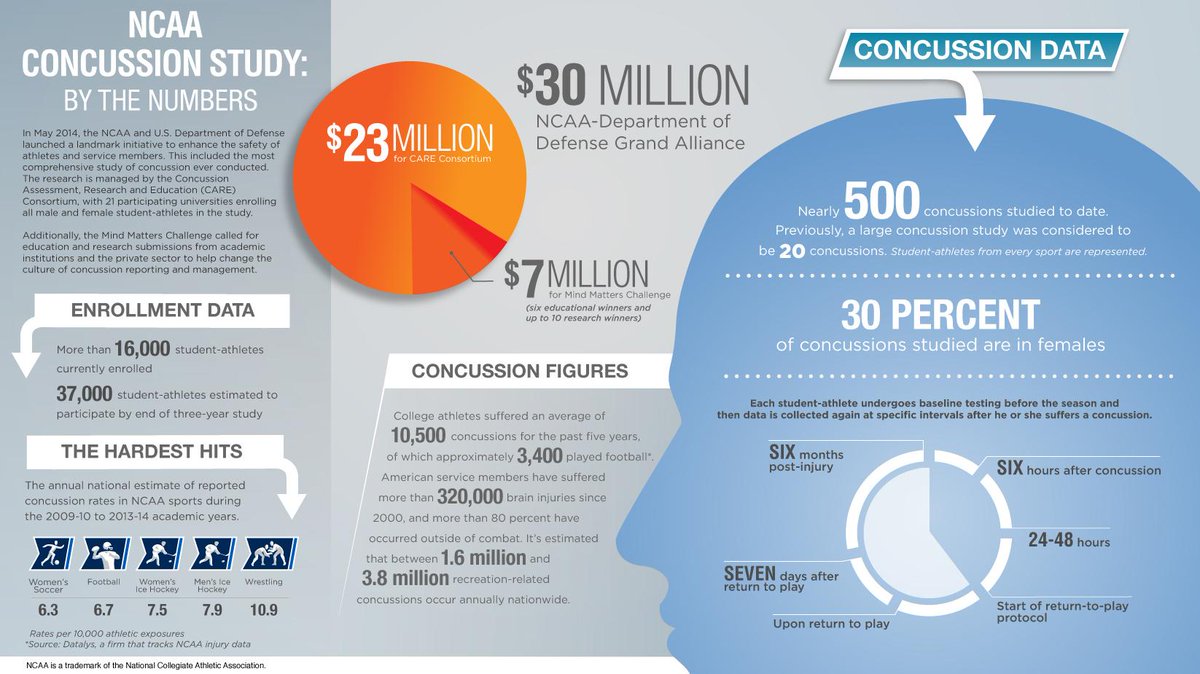
In addition, concussion symptoms are commonly not reported after impacts greater than 90g,99 and fewer than 0.35% of all impacts greater than 80g resulted in a diagnosed concussion.101 Because of the low sensitivity and specificity of head-impact sensors, systems that claim to identify concussions are not recommended at the present time; however, they may have utility for illustrating dangerous behaviors and teaching athletes how to reduce the risk of injury.101 Such devices may also allow for the study of biomechanics with the goal of influencing rule changes to improve safety in contact sports. For example, the aims of such changes would be to prevent open-field and open-ice collisions in which players may be ill prepared for high-level impacts to the head. It is important that athletes, parents, coaches, and other laypeople understand the limitations of head-impact sensor technology and instead rely on educational information93,94 regarding the recognition of concussion.
SUMMARY
The sideline assessment of the athlete after SRC is complex, and the clinical impression remains the criterion standard in making the concussion diagnosis. Asking questions that discern the athlete’s ability to recall the events of the injury, as well as those before and after the injury, and determining if he or she is slow to respond to questions, appears to have trouble processing information, or obviously struggles with simple tasks are important components of the clinical assessment. Standardized sideline concussion-assessment tools are strongly encouraged and should include individual (eg, symptoms, balance, and cognitive functioning) or bundled evaluations (eg, SCAT3) as part of the neurologic examination. The assessment should be done as soon as possible after injury, with the understanding that the optimal timing of the examination is not yet clear. To evaluate a potential concussion, recent research supports the use of sideline visual-tracking tests compared with preinjury baseline tests whenever possible, but more investigation is needed, and these tests are best used as part of a multimodal assessment.
Ultimately, clinicians should feel comfortable and confident when applying clinical suspicion to overrule a “negative” or “normal” result on a standardized sideline assessment tool. Athletes with a suspected or confirmed concussion should be removed from the field of play and not returned to playing or training on the same day. Athletes assessed for concussion should be followed with serial evaluations. If no athletic trainer or other health care professional is present, it is important to err on the side of caution, keeping any athlete suspected of having a concussion out of play until he or she can be evaluated. This process can be aided by providing education to athletes, parents, and coaches regarding the recognition of concussion signs and symptoms with subsequent removal from play. Though more study is needed, the utility of head-impact sensors in detecting potential injury is, at this time, of unclear significance, given the lack of correlation between biomechanical forces and clinical measures.:no_upscale()/cdn.vox-cdn.com/uploads/chorus_image/image/62842806/453175710.jpg.0.jpg)
Lastly, most concussion research has focused on high school and collegiate athletes, primarily males, and American football is overrepresented. Thus, a significant amount of bias is present in the information we know and underscores the need for more work in other sports and including a full spectrum of ages and of both male and female athletes.
Onfield assessment of concussion in the adult athlete
Background:
The onfield assessment of concussion in the adult athlete is challenging, given the elusiveness of injury, the sensitivity and specificity of the sideline assessment tools and the evolving nature of concussive injury. This paper reviews the evidence related to the onfield assessment and considers questions related to same day return to play, what to do when no physician is available onsite, as well as the benefit of remote notification of potential concussive events.
Objective:
To review the evidence regarding the onfield assessment of concussion in the adult athlete. Additional key issues to consider include same day return to play for the adult athlete with concussion, what to do in a community setting when no doctor is present and whether there is any benefit with remote notification of potential concussive events that occur on the playing field.
Data sources:
Systematic literature review of concussion assessment and management. PubMed, MEDLINE, Psych Info and Cochrane Library databases were reviewed using the MeSH key words concussion and mild traumatic brain injury combined with athletic injuries. Each was refined by adding the key words ‘adult’, ‘sideline assessment’, ‘onfield assessment’ and ‘return to play’.
Results:
For the MEDLINE search, using ‘concussion’ and ‘athletic injuries’ as key words, there were 880 results, and refining by ‘adult’ there were 292 results. When ‘traumatic brain injury’ and ‘athletic injuries’ were combined, there were 210 results. When refining by ‘adult’, there were 89 results. Many of these results overlapped. Following an initial review, these articles form the basis of the discussion.
Conclusions:
The onfield evaluation of sport-related concussion is often a challenge, given the elusiveness and variability of presentation, difficulty in making a timely diagnosis, specificity and sensitivity of the sideline assessment tools and the reliance on symptoms. Despite these challenges, the sideline evaluation is based on recognition of injury, assessment of symptoms, cognitive and cranial nerve function and balance. Serial assessments are often necessary and, since signs and symptoms may be delayed, erring on the side of caution (keeping an athlete out of participation when there is any suspicion for injury) is important. A standardised assessment of concussion is useful in the assessment of the athlete with suspected concussion but should not take the place of the clinician’s judgement.
Serial assessments are often necessary and, since signs and symptoms may be delayed, erring on the side of caution (keeping an athlete out of participation when there is any suspicion for injury) is important. A standardised assessment of concussion is useful in the assessment of the athlete with suspected concussion but should not take the place of the clinician’s judgement.
Concussion Protocol 101 Guide – ImPACT Applications
WHAT DOES A SIDELINE EVALUATION ENTAIL?
Sideline evaluations are a critical early measure in checking for a concussion and determining next steps in the concussion care process. After a bump, blow, or jolt to the head, a healthcare provider trained to recognize concussions should follow a well-defined sideline process.
Athletic trainers are frequently the first responders in the case of an athletic head injury. Learn about their important role.
Because a concussion often happens without an athlete losing consciousness, a healthcare provider must use screening for head injury in other ways. Without a full sideline assessment, student athletes may return to play prematurely and be at risk for negative consequences. The brain can swell and cause lasting damage or increased long-term symptoms.
Without a full sideline assessment, student athletes may return to play prematurely and be at risk for negative consequences. The brain can swell and cause lasting damage or increased long-term symptoms.
A sideline evaluation should include a symptom check and memory screening, cognitive functioning, and concentration. Its purpose is to determine if a trip to an emergency department is necessary. If not, they’ll determine if removal from participation with continued monitoring is warranted.
Brief tests like ImPACT Quick Test can help a healthcare provider quickly check cognitive function. Sideline professionals should also be on the lookout for worsening symptoms.
WHAT IS CONCUSSION SCREENING?
A concussion screening is a brief evaluation conducted by a trained healthcare provider. Its purpose is to determine the presence of a concussion after a blow to the head.
A trained healthcare provider will document whether or not there was a hit to the head and the location of impact. They will check for visible injury to the head or body. They’ll record if there was loss of consciousness, amnesia before or after the event, and any early concussion signs.
They will check for visible injury to the head or body. They’ll record if there was loss of consciousness, amnesia before or after the event, and any early concussion signs.
They will ask the patient about any symptoms they feel. They’ll likely conduct a brief cognitive screening to help make the removal from activity decision. They will determine if the patient requires an emergency department visit. The healthcare provider will continue monitoring for any new symptoms that might appear after the injury.
WHAT IS BASELINE COGNITIVE TESTING?
A baseline test measures your brain function in a healthy state. If you have an injury, healthcare providers can use a post-injury test to help determine if you have a concussion. It measures reaction time, memory capacity, speed of mental processing, and executive functioning of the brain. Baseline testing is recommended to be completed annually to ensure an up-to-date record of a patient’s normal functioning.
A trained healthcare provider can compare a post-injury test to a patient’s baseline.This way, they’ll have an objective idea of the extent of the injury. While concussions aren’t preventable, baseline testing is a great way to ensure someone is prepared if a concussion ever happens.
If you don’t have time or resources to group baseline test all your test takers, you have two other time-saving options:
- Send test takers a unique baseline testing link via email from your Customer Center. The tests come out of your normal testing bank.
- Have test takers pay for a baseline test individually and take it at home.
WHAT IS POST-INJURY TESTING?
It measures the same areas as baseline testing. Healthcare providers use post-injury testing to understand a patient’s cognitive functioning after a jolt to the head. A post-injury clinical report is compared to a patient’s baseline to show deficits in cognitive functioning and reaction time.
Post-injury testing can still be used if a test taker doesn’t have a baseline. This is thanks to normative data, which provides average scores within an age range. Post-injury testing is done by trained healthcare providers who use the test and other data to help evaluate a concussion. They’ll use it to develop an appropriate treatment plan to provide the most efficient recovery pattern.
WHAT IS SANDBAGGING AND HOW DOES IT IMPACT CONCUSSION TESTING?
Sandbagging is when a test taker deliberately underperforms on a baseline concussion test.Many athletes are aware that their ability to return to activity is determined by their baseline results. They may perform poorly to lower the threshold of comparison when their healthcare provider is deciding whether or not to clear them. It is not easy to sandbag during baseline testing because of built in validity indicators that flag suspicious results.
Read more about sports concussions and sandbagging as well as the preventative measures you can take.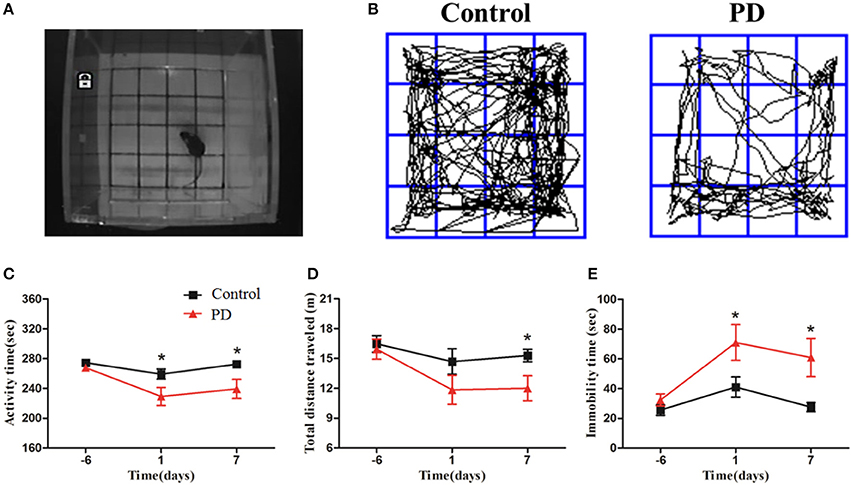
Mayo Clinic Announces New Sideline Protocol: Concussion Check
While a great number of medical resources are devoted to elite-level and professional athletic organizations, youth and recreational sports—at which the vast majority of sports are played—are operating under a vastly different set of safety standards.
Of the 40 million youth athletes in the United States, over half are not supervised by trained medical professionals during practice or games. As a result, children and young adults are oftentimes unprotected when it comes to identifying and treating concussion, putting a large number of children at risk for injury or—in rare cases—death each time they step out on the playing field.
Concussion Check, the Mayo Clinic’s new remove-from-play protocol, provides parents, coaches and teachers with the tools they need to protect young athletes and keep sports safe—even when a medical professional isn’t on hand.
What is Concussion Check?
Concussion Check is a standardized, three-step protocol that can be used by individuals without medical training to identify the signs and symptoms of concussion. The protocol was created to protect youth athletes by empowering parents to make informed decisions about removing young athletes from play when a trained medical professional is not available.
The protocol was created to protect youth athletes by empowering parents to make informed decisions about removing young athletes from play when a trained medical professional is not available.
Concussion Check is like a three-legged stool: if one leg is broken, the stool falls. If a young athlete fails any one of the three steps, they should be removed from play immediately and further evaluated by a medical professional.
Mayo Clinic Concussion Check Steps
Step 1: Recognize and Remove
Parents and other individuals watch for signs and symptoms of concussion during practices and games, keeping an eye out for hits that could be of concern. If they notice anything, they will remove the injured athlete from play.
Step 2: Memory Assessment
A parent will then ask the athlete some basic orientation questions, such as “Is it before or after lunch?” and “What’s your coach’s name?” The protocol’s questions were formulated with youth in mind, and the wrong answer is a strong indicator that something’s off.
Step 3: King-Devick Test in association with Mayo Clinic
Lastly, the parent will administer the King-Devick Test in Association with Mayo Clinic. This portable, two-minute assessment is a sensitive sideline measurement for concussion that evaluates an individual’s eye movements, attention and language. Athletes will need to complete the K-D Test during the pre-season to establish a baseline performance, which will be compared to post-injury test performance.
If the individual fails any of these three steps, they should immediately be removed from play and directed to a healthcare professional—ideally one who specializes in concussion treatment. To learn more about Concussion Check and read articles from Mayo Clinic’s team of concussion experts, visit mayoclinic.org/concussioncheck.
On-field Examination for Concussion Tamara McLeod Athletic Training Neurology Orthopedics Pediatrics Sports 3868
Question
What is included in an on-field examination for a concussion?
Answer
Sport-related concussion recognition includes being able to recognize the injury on the field. This is where the healthcare providers that are out covering sports are a key member of the healthcare team and a key member in recognizing and diagnosing these particular injuries.
This is where the healthcare providers that are out covering sports are a key member of the healthcare team and a key member in recognizing and diagnosing these particular injuries.
With the on-field evaluation, we want to make sure we implement our emergency action plan (EAP). We want to make sure we’re ruling out more serious injuries by recognizing signs and symptoms of intracranial bleeding, such as loss of consciousness, cranial nerve deficits, decreasing mental status and worsening symptoms over time (Dunning et al., 2004). This should be done through a sideline evaluation that serves as the benchmark for serial assessments, with reassessment occurring at five- to ten-minute intervals, until the decision is made to refer the patient or just monitor them through the course of the practice or the game.
Our on-field primary survey should be what we do for all other emergent injuries, including a check of airway, breathing, circulation, and cervical spine. There was a lot of discussion in the Berlin meeting about associated cervicogenic issues. In the immediate care, we do want to make sure we rule out a cervical spine injury. When we get to treatment and rehabilitation, we want to make sure that we are managing those appropriately with different treatment modalities.
In the immediate care, we do want to make sure we rule out a cervical spine injury. When we get to treatment and rehabilitation, we want to make sure that we are managing those appropriately with different treatment modalities.
As part of our on-field evaluation, we want to assess the level of consciousness (i.e., whether the athlete is alert, lethargic, stuporous, semi-comatose or comatose). However, it is important to note that less than 10% of concussions result in loss of consciousness (Guskiewicz et al., 2000, 2003; McCrea et al., 2003). As such, we certainly don’t want to use that as our key symptom or sign that we’re looking for, because the majority of concussions are not going to involve loss of consciousness. Interestingly, loss of consciousness has not been related to severity and/or recovery (McCrory et al., 2004). Initial symptom burden tends to be a more consistent predictor of slower recovery in athletes after concussion.
The Berlin recommendations for the on-field screen include that it be a rapid screen (either “go” or “no-go”). We first want to clear the on-field signs, including any loss of consciousness, ataxia, tonic posturing or post-traumatic seizure, which at minimum results in an immediate diagnosis of concussion, but some of these can be indicative of a more severe injury (Patricios, 2017). The SCAT-5 itself includes a first page that has the immediate or on-field assessment information. You’ll see several different iterations of the SCAT-5 tool in today’s presentation, because it is used in conjunction with various recommendations.
We first want to clear the on-field signs, including any loss of consciousness, ataxia, tonic posturing or post-traumatic seizure, which at minimum results in an immediate diagnosis of concussion, but some of these can be indicative of a more severe injury (Patricios, 2017). The SCAT-5 itself includes a first page that has the immediate or on-field assessment information. You’ll see several different iterations of the SCAT-5 tool in today’s presentation, because it is used in conjunction with various recommendations.
The first piece is the on-field assessment where we’re looking for red flags that would warrant immediate referral (Anderson & Schnebel, 2016; Hyden & Petty, 2016). These may include:
- Deteriorating level of consciousness (LOC)
- Loss of or fluctuating LOC
- Increased confusion
- Inability to recognize people and places
- Increased irritability
- Worsening headache
- Repeated vomiting (some indicate three times, although this number is somewhat arbitrary)
- Extremity numbness
- Signs of skull fracture
- Focal findings on neurologic exams (e.
 g., cranial nerve deficits)
g., cranial nerve deficits) - Seizure
- Glasgow Coma Scale of less than (<) 13
With the Berlin paradigm, after this rapid screen for a suspected sport-related concussion (SRC), you then want to assess and clear those on-field signs. If the suspicion still exists following a significant head impact, or if the patient is reporting symptoms, you would then proceed to the sideline screening using appropriate assessment tools. At this point, a more thorough diagnostic evaluation can be done, ideally in a distraction-free environment.
FAQs about Baseline Testing | HEADS UP
To help answer some common questions about baseline testing among young athletes, CDC has compiled a list of frequently asked questions to help you, your school, or your league prepare for concussions both pre- and post-season.
What is baseline testing?
Baseline testing is a pre-season exam conducted by a trained health care professional. Baseline tests are used to assess an athlete’s balance and brain function (including learning and memory skills, ability to pay attention or concentrate, and how quickly he or she thinks and solve problems), as well as for the presence of any concussion symptoms. Results from baseline tests (or pre-injury tests) can be used and compared to a similar exam conducted by a health care professional during the season if an athlete has a suspected concussion.
Results from baseline tests (or pre-injury tests) can be used and compared to a similar exam conducted by a health care professional during the season if an athlete has a suspected concussion.
Baseline testing generally takes place during the pre-season—ideally prior to the first practice. It is important to note that some baseline and concussion assessment tools are only suggested for use among athletes ages 10 years and older.
How is baseline testing information used if an athlete has a suspected concussion?
Results from baseline testing can be used if an athlete has a suspected concussion. Comparing post-injury test results to baseline test results can assist health care professionals in identifying the effects of the injury and making more informed return to school and play decisions.
Education should always be provided to athletes and parents if an athlete has a suspected concussion. This should include information on safely returning to school and play, tips to aid in recovery (such as rest), danger signs and when to seek immediate care, and how to help reduce an athlete’s risk for a future concussion.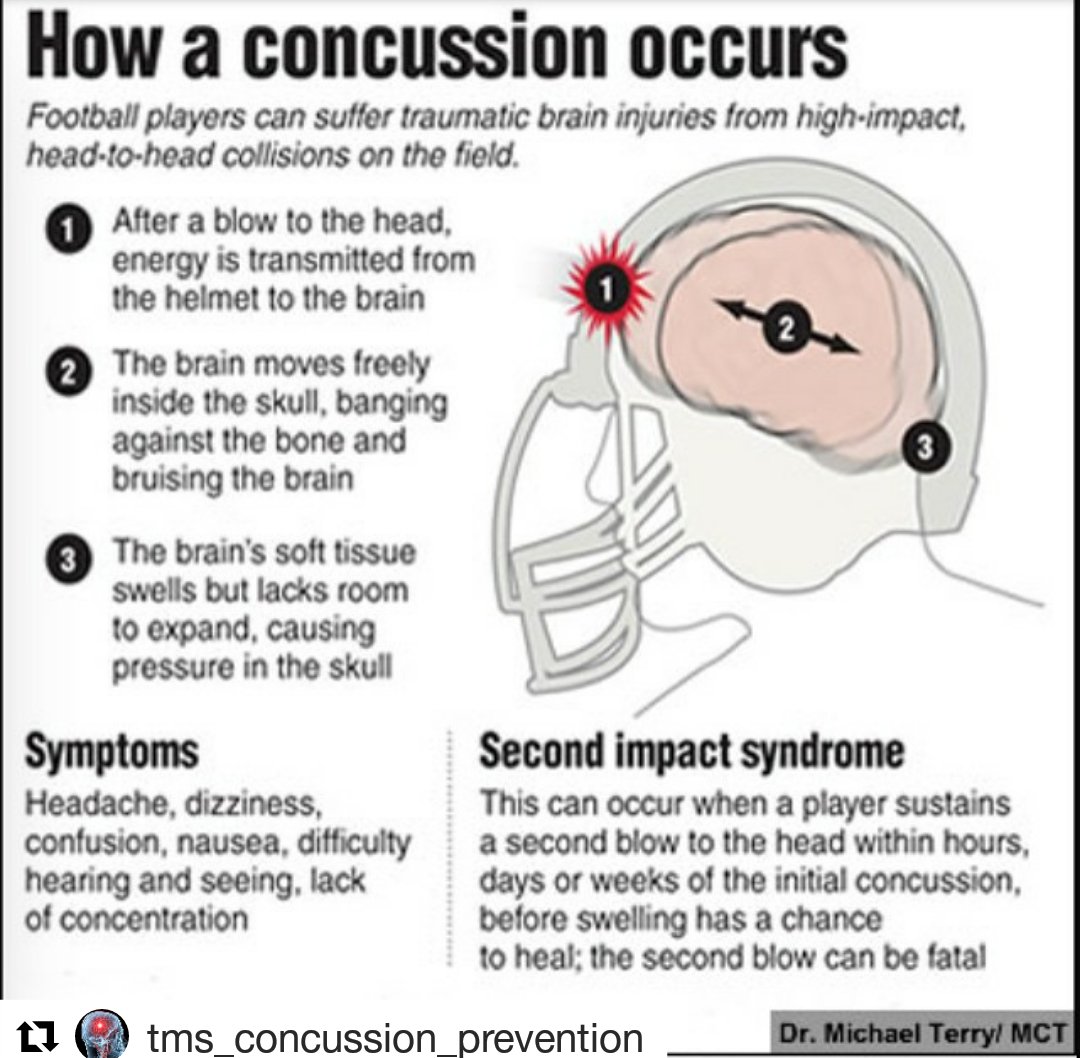
What should be included as part of baseline testing?
Baseline testing should include a check for concussion symptoms, as well as balance and cognitive (such as concentration and memory) assessments. Computerized or paper-pencil neuropsychological tests may be included as a piece of an overall baseline test to assess an athlete’s concentration, memory, and reaction time.
During the baseline pre-season test, health care professionals should also assess for a prior history of concussion (including symptoms experienced and length of recovery from the injury). It is also important to record other medical conditions that could impact recovery after concussion, such as a history of migraines, depression, mood disorders, or anxiety, as well as learning disabilities and Attention Deficit/Hyperactivity Disorder.
Baseline testing also provides an important opportunity to educate athletes and others about concussion and return to school and play protocols.
Who should administer baseline tests?
Baseline tests should only be conducted by a trained health care professional.
Who should interpret baseline tests?
Only a trained health care professional with experience in concussion management should interpret the results of a baseline exam. When possible, ideally a neuropsychologist should interpret the computerized or paper-pencil neuropsychological test components of a baseline exam. Results of neuropsychological tests should not be used as a stand-alone diagnostic tool, but should serve as one component used by health care professionals to make return to school and play decisions.
How often should an athlete undergo baseline testing?
If baseline testing is used, research suggests that most components of baseline testing be repeated annually to establish a valid test result for comparison. Baseline computerized or paper-pencil neuropsychological tests may be repeated every 2 years. However, more frequent neuropsychological testing may be needed if an athlete has sustained a concussion or if the athlete has a medical condition that could affect results of the test.
Learn More about Concussions and Brain Injury
90,000 Concussion – very serious. It’s time to stop admiring those who return to the field after head injuries – An underappreciated opinion – Blogs
Therefore, an additional replacement is introduced in the Premier League and RPL due to concussions.
Sports doctors and neurologists have been pushing for tougher penalties for inflicting head injuries for many years – here is a detailed explanation of why such collisions are dangerous. Football is gradually realizing the problem and looking for a solution. For example, at the club World Cup, an out-of-limit substitution was introduced for players who received a concussion.The same idea is being actively discussed in the RPL and the Premier League – in these leagues, an additional replacement can be introduced as early as February. But why only because of the concussion and how to avoid abuse? Let’s figure it out.
The main problem with concussions is the lack of evidence of symptoms.
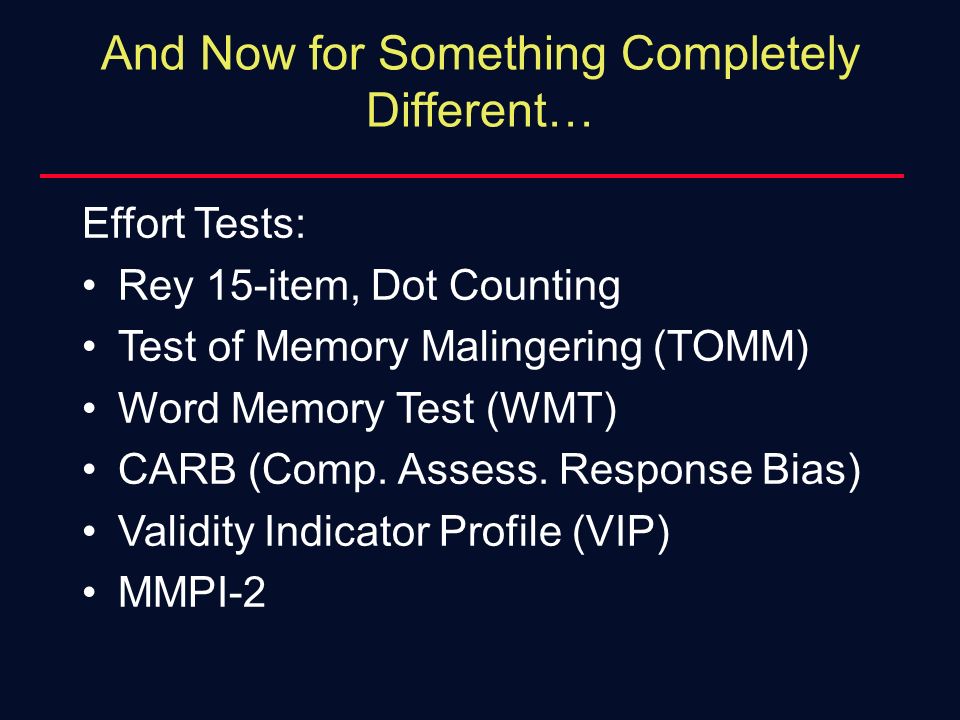 And the consequences can appear after many years
And the consequences can appear after many years
Let’s start with how the doctor determines the need for replacement and generally diagnoses a concussion in the field? The main symptoms in the first hours: confusion, disorientation, inhibited reaction, stunning.For objectivity, FIFA proposes to use SCAT5 (SPORT CONCUSSION ASSESSMENT TOOL – 5TH EDITION) – a special questionnaire according to which the doctor evaluates the above symptoms. Basically, there are questions related to orientation in time and place: what time is it, day of the week, with whom we are playing, who scored the last goal and others. Obviously, a healthy person will answer without hesitation.
Next come the objective symptoms, that is, reliably speaking of a serious injury. They are also called “red flags”.In medicine, this term is used to refer to especially important (and dangerous) signs that should never be overlooked. If there are any, then the footballer should not only be immediately replaced, but also sent to the hospital. There are not so many of them and it is difficult to miss them:
There are not so many of them and it is difficult to miss them:
• pain and / or instability in the cervical spine;
• impaired visual acuity, double vision;
• a burning sensation, tingling sensation, numbness in the hands and / or feet;
• severe and / or worsening headache;
• loss of consciousness;
• convulsions;
• worsening of the condition right during the examination;
• vomiting;
• aggressiveness, nervousness.
But there are important subtleties, they are also spelled out in the protocol: the symptoms of a concussion may not appear immediately, but after 10 minutes or more. A e If a football player is completely healthy from the point of view of SCAT5, then this does not exclude a concussion of the brain . Therefore, if the blow was really strong, a replacement is recommended.
However, as we can see, football players rarely leave the field even after the most difficult clashes, but worst of all, this is encouraged by both other players and spectators. This is a dangerous trend. Researchers from the University of Glasgow examined the medical records and causes of death of 7,676 professional ex-footballers who played from 1900 to 1976, and 23,000 non-athletes. According to a study, former footballers are 3.5 times more likely to suffer from dementia and diseases of the nervous system. And that’s not all: the risk of Parkinson’s disease is 2 times higher, the risk of Lou Gehrig’s is 4 times, and Alzheimer’s is 5 times higher.
This is a dangerous trend. Researchers from the University of Glasgow examined the medical records and causes of death of 7,676 professional ex-footballers who played from 1900 to 1976, and 23,000 non-athletes. According to a study, former footballers are 3.5 times more likely to suffer from dementia and diseases of the nervous system. And that’s not all: the risk of Parkinson’s disease is 2 times higher, the risk of Lou Gehrig’s is 4 times, and Alzheimer’s is 5 times higher.
It is associated with two syndromes: PCS and CTE. Don’t be intimidated by complex terms, they are actually quite simple.
PCS (Post-concussion syndrome) – as the name suggests, a condition after a concussion when its symptoms or part of them persist for months. In rare cases, even for years. The mechanism of occurrence is not precisely defined, since in absolutely identical cases, some people developed PCS, while others did not. It is believed that this condition causes a combination of reasons: structural changes in the tissues of the brain and its vessels, injury to the cervical spine, and even depression after the injury. And repeated or not timely cured concussions increase the chances of developing such a pathology.
And repeated or not timely cured concussions increase the chances of developing such a pathology.
CTE (Chronic Traumatic Encephalopathy) – chronic post-traumatic encephalopathy. Translated into Russian, it is dementia caused by repeated head injuries. It is believed that because of them, irreversible damage to brain cells and connections between them occurs, as a result of which the brain literally begins to dry out, and a person’s mental abilities fade away. At first, these are subtle changes – forgetfulness, difficulties in calculating the amount of purchases in the store.Simply put, the more difficult mental work is, the more difficult it is. Further, the symptoms increase, the vocabulary becomes scarce, the phrases become monosyllabic, and the person gradually loses the ability to perform the simplest actions on his own.
Of course, you need to understand that CTE has been developing for decades and for everyone at a different rate. For some, it simply does not arise, and someone simply does not live up to it or its later stages. Therefore, for a long time this pathology remained poorly understood. Unfortunately, few people think about such distant consequences during matches, the realization comes much later.For example, the words of Vasily Berezutsky:
Therefore, for a long time this pathology remained poorly understood. Unfortunately, few people think about such distant consequences during matches, the realization comes much later.For example, the words of Vasily Berezutsky:
“Identifying a concussion is difficult. Any heavy head bump is already a microshock. It all depends on whether a person can stay on the football field.
From my career I remember only the match against Lokomotiv. The opponent had a fracture, I had a concussion anyway. But I finished playing. I don’t think it had a good effect on my head and on the heads of everyone else. The best thing in these situations is the replacement . But sometimes you want to play.In such situations, the decision is probably made by the player. It all depends on the importance of the match.
I know a lot of footballers who said, “I’m staying.” The doctor, realizing that this is impossible, can remove the person. I often made decisions that I would continue to play. This is not because of courage, but, probably, more because of stupidity. ”
This is not because of courage, but, probably, more because of stupidity. ”
But why is the replacement only due to concussions, because there are a bunch of other serious injuries?
It’s all about the non-obviousness of the symptoms. It is difficult to prove to a player or coach that you need to be replaced, because you cannot read this text to him in a couple of seconds during a match.And it is unlikely that a person after a strong blow to the head is ready to perceive such information and think about what will happen to him in 40-50 years.
Second factor: replacement is risk. Spend everything and be outnumbered in case of injury, or save one just in case? This question is an important part of football, remember how forced substitutions turned important matches and gave sensations.
In the event of a serious injury, the question of whether to change a player or not is simply not worth it. You will either replace him or remove him from the game and remain in the minority. But with the concussion, as we discussed above, everything is far from so simple. Players with a broken head, barely understanding what is happening at all, remain on the field, risking aggravating the injury, and this is romanticized by fans and the media: “Fighter! Warrior! A real man!” And few people are worried about what will happen by the age of 50.
But with the concussion, as we discussed above, everything is far from so simple. Players with a broken head, barely understanding what is happening at all, remain on the field, risking aggravating the injury, and this is romanticized by fans and the media: “Fighter! Warrior! A real man!” And few people are worried about what will happen by the age of 50.
Simply put, the need for replacement in the event of any other severe injury is not even discussed. But for some reason, when it comes to head injuries, no one thinks so.For some reason, people think that it is more dangerous to break a hand than to forget how to use it in 40 years.
Will the teams abuse their substitution rights?
This is much easier to control than it looks. First, despite all the non-obvious clinic for making a diagnosis, in the field, the main factor is a blow to the head. Whether it’s contact with an opponent or a bad fall. After all, hardly anyone, in order to knock out a strategic replacement, will run to ram the bar with his head.
Another point is the uniqueness of the application of the rule itself. At the Club World Cup, a substitute for a concussion player can only be used once per game; in the Premier League and RPL, a more complex scenario is considered. According to Sports.ru, the RFU medical committee offers this option: the right to an additional replacement appears only if all replacements or slots for them are used.
As we can see from the graph, the RPL teams in the past and this season rarely used even the 5 substitutions provided to them, so abuse is unlikely, so the rule will apply in really exceptional cases.
Timely replacement is important because of the tactics of treatment. For the most part it’s just peace
The main task of a sports doctor on the field is the timely diagnosis and exclusion of life-threatening conditions. And, of course, first aid. Then the victim with suspected concussion is taken to the nearest hospital, where a computed tomography (CT) scan of the head is performed. This is necessary to exclude damage to the bones of the skull, cervical vertebrae, intracranial hematomas and cerebral edema.The main danger of traumatic brain injury is that the space in the skull is limited, and a growing hematoma or progressive cerebral edema will cause its structures to shift (dislocation of the brain), which ultimately can lead, for example, to wedging into the foramen magnum.
This is necessary to exclude damage to the bones of the skull, cervical vertebrae, intracranial hematomas and cerebral edema.The main danger of traumatic brain injury is that the space in the skull is limited, and a growing hematoma or progressive cerebral edema will cause its structures to shift (dislocation of the brain), which ultimately can lead, for example, to wedging into the foramen magnum.
In this case, the areas of the brain located in this area are squeezed, namely, the centers of respiration and heart rate. In addition, due to the compression, the outflow of blood and cerebrospinal fluid from the brain tissue is disturbed, due to which the edema intensifies even more, and the brain ceases to receive oxygen and nutrients.
Moreover, edema can form for several days, so doctors recommend rest and observation of the patient for at least 72 hours.
The criteria for returning to the general group are the complete absence of complaints, any symptoms of concussion and a normal picture on CT if it was performed within 3 days from the moment of injury. In mild cases, recovery usually takes no more than 3-5 days and essentially consists of rest: minimal physical activity, avoiding loud sounds (music), especially with headphones.It is undesirable to watch TV and work at a computer. In more severe cases – individually, depending on the accompanying injuries and complaints.
In mild cases, recovery usually takes no more than 3-5 days and essentially consists of rest: minimal physical activity, avoiding loud sounds (music), especially with headphones.It is undesirable to watch TV and work at a computer. In more severe cases – individually, depending on the accompanying injuries and complaints.
It turns out that in most cases, if a player is replaced in a timely manner, given a few days of rest, then he will be ready for the next match. Maximum – will miss one game. But the risk of long-term complications and additional injuries is reduced significantly. The current practice is questionable. It is a little strange that a doctor, when deciding on a replacement, listens to the opinion of a person without medical education, who has just received a blow to the head.
My Telegram channel about sports medicine
Photo: Gettyimages.ru/Catherine Ivill, Stephane Mahe
An additional replacement will be tested in the Russian Football Championship :: Football :: RBC Sport
Russian Premier League clubs may be allowed to make a sixth substitution of a fielder in case of suspected concussion
Read us at
news
news
Photo: globallookpress
The RPL leadership for the first time raised the issue of the sixth replacement of field players in the event of a serious injury (concussion). This was reported on the official website of the Russian Football Championship.
This was reported on the official website of the Russian Football Championship.
The test of the new test rule is planned to be done in the near future, before the resumption of the Russian football championship, which is scheduled for the end of February. In connection with the coronavirus in the RPL, it is officially allowed to carry out five permutations of football players per match, including club goalkeepers. In the summer of 2020, the International Football Association Board (IFAB) extended the five-substitution rule until the end of 2021. Before the pandemic, teams had three substitutions, four in the National Football League (FNL), and five in the Professional Football League (PFL).
On November 18 last year, CSKA defender Igor Diveev spent 42 minutes with the Russian national team against Serbia (0: 5) in the League of Nations with a closed craniocerebral head injury and dislocation of the nasal bones. However, the doctor of the Russian national team at the end of the game said that the footballer did not ask the coaching staff for a replacement.
CSKA bought the rights to 19-year-old defender Diveev from Ufa
Another episode related to a head injury occurred on August 18, 2001 in the Russian Premier League match between Anji and CSKA.At the end of the game, the guests’ goalkeeper Sergey Perkhun was seriously injured as a result of a collision with the Makhachkala team’s forward Budun Budunov. Doctors gave the goalkeeper first aid on the spot, but on the way to the local hospital, Perhun lost consciousness and fell into a coma. Soon the goalkeeper was transported to Moscow to the Burdenko Institute of Neurology, but the capital’s doctors failed to save the goalkeeper’s life. On August 28, 2001, the football player died without regaining consciousness, as a result of cerebral edema.At the time of his death, Perhun was only 23 years old.
On August 28, 2001, the football player died without regaining consciousness, as a result of cerebral edema.At the time of his death, Perhun was only 23 years old.
In the fall of 2006, Czech goalkeeper Petr Cech of London Chelsea suffered a skull fracture in the English Premier League match against Reading after a collision with host midfielder Stephen Hunt. This episode cost the Czech goalkeeper a year of his professional career. According to the results of a medical examination, the football player was diagnosed with a depressed skull fracture. Until the end of his professional career in winter 2019 (playing for Arsenal London), the goalkeeper continued to play in a special protective helmet that protects his head from potential injuries.
The Russian football championship will resume on February 26, 2021 with the 20th round match between Tambov and Rotor. In the central meeting of the tour, Lokomotiv Moscow will host the capital’s CSKA, the derby is scheduled for February 27, beginning at 19:00 Moscow time.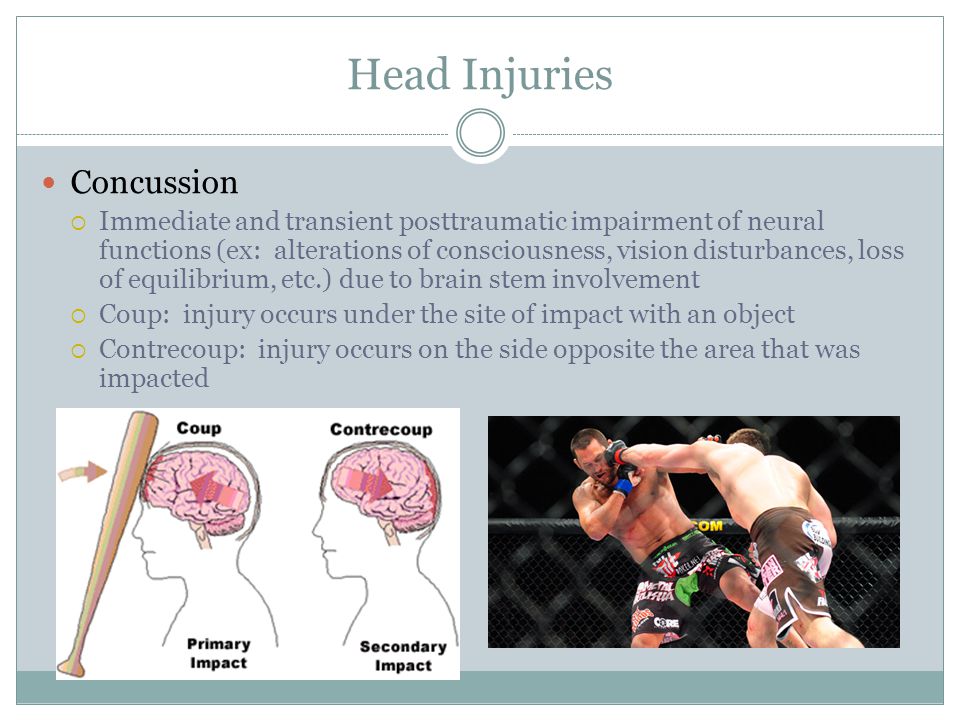
Author
Anatoly Akulov
Handheld Eye-Sync detects concussion
SyncThink has developed a compact Eye-Sync monitor that can determine if an athlete has a concussion (traumatic brain injury) in the field in just 60 seconds.The model fits into a small case and can be transported manually by sports trainers, as well as, if necessary, by rescuers and representatives of other emergency services.
In case of concussion, appropriate care must be taken. At the same time, today this diagnosis in the field is done “by eye”, which leads to the appearance of medical errors and damage to human health. This is especially true for field players, boxers and other athletes who often go to trainings without being accompanied by doctors.
Technologically, SyncThink Eye-Sync consists of a headset-style virtual reality device and a connector for connecting to a tablet computer. If a concussion is suspected, the trainer will use a headset in the absence of a qualified doctor. The athlete follows with his eyes a small circle on the screen, which moves along a predetermined trajectory.
Cameras inside the headset track eye movement. If the direction of gaze is too chaotic and intermittent, this indicates a high probability of receiving a head injury, which requires urgent medical intervention.The analysis results are displayed on the display of the trainer tablet.
Eye-Sync is currently tested at Stanford University and is ready for commercial use. Information on this can be found at syncthink.com.
Source: www.mobipukka.ru
– Attention! Before buying goods or services, carefully read the reviews! – Manufacturers can change them without notice! – Therefore, the characteristics are correct at the time of publication of the material (see the date of the article).
WE ARE IN CONTACT:
Vision Training Methods for Sports Concussion Mitigation and Management
Vision training, when initiated as a team of broad exercises, reduces the frequency of concussion in those players, compared to players who do not receive vision training 7. Vision training produces functional and operational changes that can be quantitatively monitored to measure training success and can be initiated as part of a sports medical intervention to prevent concussions.Functional changes are changes in measurement, for example faster reaction times are documented during vision training. The goal is to have a change in performance such as improved performance while changing the rig from the ball is improved.
The goal is to have a change in performance such as improved performance while changing the rig from the ball is improved.
Details of instructional vision programmatic methods and representative data are provided for use as a frame of reference for clinicians who wish to use teaching methods components in their concussion management programs.These data links can also be used when monitoring a subject DurING injury recovery using one of the onboard light programs.
The components of a vision training program include the following. * The program uses traditional eye-hand reaction training to challenge an individual’s hand-eye coordination in multiple visual fields. Reaction Test The program evaluates and trains visual and motor response times for the left and right hands. Concussion Programs are used as a means to assess and monitor subjects that have had a concussion.Broca’s string is used to develop convergence skills, ocular motor skills, and to minimize suppression. It also aids fantastic xation skills under binocular conditions. Eye Exercises are designed to improve visual performance by training the speed, accuracy and efficiency of the eyes. Accommodation Fins are used to enhance the reflex action of the eye to make the accommodative muscles move faster and with precision. The tachistoscope is used to increase the recognition rate, to show something too quickly consciously recognized, or to check which elements of the image are characteristic.Pinhole glasses or goggles with Strobe Pitch and Catch are used to improve vision processing and focus. Saccadic Eye Movement Training is used to develop rapid eye movement. Near Far Teaching to focus the eye near and far. Stereoscopic is designed to assess both gross binocular and excellent depth perception. Subjects can do all kinds of training. Please note that concussion programs are not training. They are for testing purposes only.
Eye Exercises are designed to improve visual performance by training the speed, accuracy and efficiency of the eyes. Accommodation Fins are used to enhance the reflex action of the eye to make the accommodative muscles move faster and with precision. The tachistoscope is used to increase the recognition rate, to show something too quickly consciously recognized, or to check which elements of the image are characteristic.Pinhole glasses or goggles with Strobe Pitch and Catch are used to improve vision processing and focus. Saccadic Eye Movement Training is used to develop rapid eye movement. Near Far Teaching to focus the eye near and far. Stereoscopic is designed to assess both gross binocular and excellent depth perception. Subjects can do all kinds of training. Please note that concussion programs are not training. They are for testing purposes only.
Athletes consistently improve after vision training in their * A, test response and binocular assessment. In addition, improvements in concussion assessment tasks are seen, which are more and more complex in design.
It is important that subjects have the pre-season and training season to see sustained benefits. Twice a week, 20 minutes at a time, for six weeks, it was found to benefit athletes as well as IX times a week for 2.5 weeks in the offseason.Then in season once a week can be performed as a maintenance program. Training should also be sport or posture and specific when possible, such as trainings that include speed and eye strength of hand coordination for electricians on a football team versus trainings that include speed and accuracy for a wide receiver. Electricians have the task of quickly controlling other hands of electricians in which it requires great strength and fast hands.This can be DynaVision training with resistance bands on the person’s wrists. Receivers need good eye-hand coordination with very good accuracy in order to be able to catch balls in very dynamic conditions, such as when working on the field.
Teaching methods have been adopted and combined with existing methods and have been shown to be effective in two different college sports 3,5,7,17. Previous studies were informal and not while the scientific methods described in this article were verified 3,5,7. Thus, these techniques help the sports healthcare professional by demonstrating what to do and how to do vision training to maximize their success in player performance and safety.
Previous studies were informal and not while the scientific methods described in this article were verified 3,5,7. Thus, these techniques help the sports healthcare professional by demonstrating what to do and how to do vision training to maximize their success in player performance and safety.
Prevention of injury from improved functional peripheral vision may result from an athlete’s increased recognition of what is happening in their peripheral vision and faster response times without removing the main vision from the original target 1,2,9. For example, in the case of a wide receiver in football, which has its central field of view of football in the air, but the oncoming defender approaches with peripheral vision, that the player can make a catch during preparation to avoid or protect himself from the oncoming defender with faster reaction times …Coaches often preach using peripheral vision during competition, but in the case of a light board system and an Oe external training, the inner rings quantify the accuracy of peripheral vision. The ability of peripheral vision to distinguish colors and movements is a component of the fidelity of peripheral vision. For an athlete doing vision training the ability to recognize an opponent against the same team in peripheral vision is better considered improving the fidelity of peripheral vision.
The ability of peripheral vision to distinguish colors and movements is a component of the fidelity of peripheral vision. For an athlete doing vision training the ability to recognize an opponent against the same team in peripheral vision is better considered improving the fidelity of peripheral vision.
In table 1, the outer rings take a longer time to hit, as opposed to the rings in the center of the board, which is the center of the field of view. One explanation could be that the increased distance to travel to reach the outer rings explains the delayed reaction time. While this may be somewhat true, if the distances required to reach the buttons were considered as the reason for the time required, ring three might be expected to have a better time, as it is about shoulder width apart (21.5 inches in diameter) where items are usually in their hands in a neutral position.Hands hitting ring three, therefore, will have the shortest distance to travel. As can be seen from Table 1, , however, gradually more times taken to hit the buttons based on the distance from the central field of view.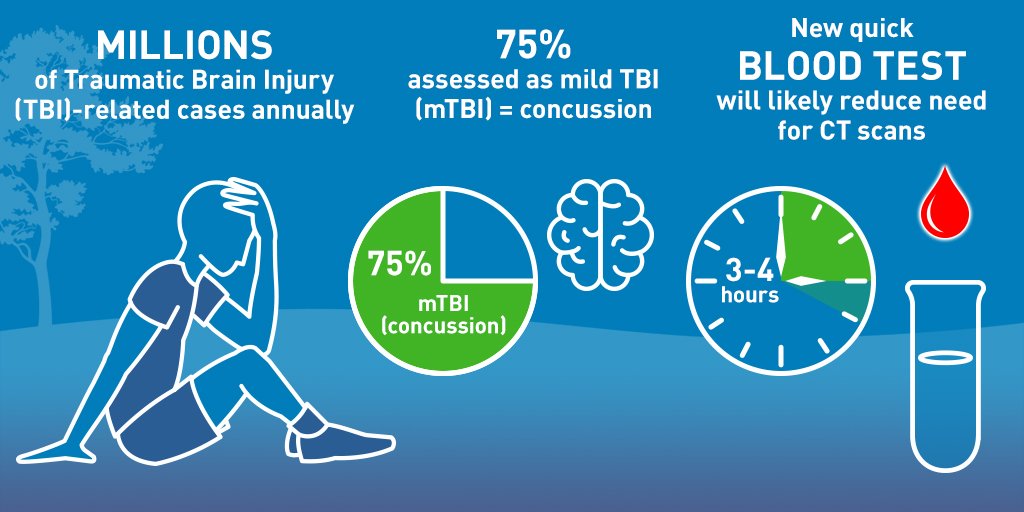 We will support that the reaction time of the eye with the hand is faster in the central visual fields and slower in the peripheral visual fields.
We will support that the reaction time of the eye with the hand is faster in the central visual fields and slower in the peripheral visual fields.
Concussion task interpretation
Concussion 1 double task or multitasking test. This requires the subject to perform continuous visual-motor tasks (press buttons), as well as processing intermittent visual-speech information (calling numbers that appear on the screen).In this age group and based on our experience, it is normal for the test to have 70 hits for points for the first run on DynaVision. This is based on our empirical experience with hundreds of college level athletes. Concussion 2 is a two-pronged task of using the executIve function. It takes memory and using this memory to add numbers. Athletes should be able to accomplish this task with little or no reduction in the mechanical performance of the button stroke. With healthy athletes, this test must have 70 or higher hits, with no significant pauses and no more than one missed number or joining error. Concussion 3 multitasking, memory and frontal lobe / differentiation task. The cognitive need for this task requires many areas of the brain to work together with minimal decrements on the primary motor task. Subjects should call “green” only when or shortly after the appearance of a green light. The task also requires the subject to decide how to name it, as well as remember the numbers when interrupted by the speaking task.
Concussion 3 multitasking, memory and frontal lobe / differentiation task. The cognitive need for this task requires many areas of the brain to work together with minimal decrements on the primary motor task. Subjects should call “green” only when or shortly after the appearance of a green light. The task also requires the subject to decide how to name it, as well as remember the numbers when interrupted by the speaking task.
Comparing scores from 1 Concussion Concussion, 2 and 3 Concussion tests, there was little and no significant improvement in performance as multitasking increased.This is probably a practice effect. Shaking 1 to 3 programs are increasingly challenging, and normal healthy people are shown here to improve their engine efficiency on more challenging tasks; although not significantly. When a concussion is suspected the patient has a significant drop in performance from impairment in the complex brain of multitasking 90,153 10.18 may be indicated. Based on these data, a range of 10% scores in three concussion programs can be considered normal for humans.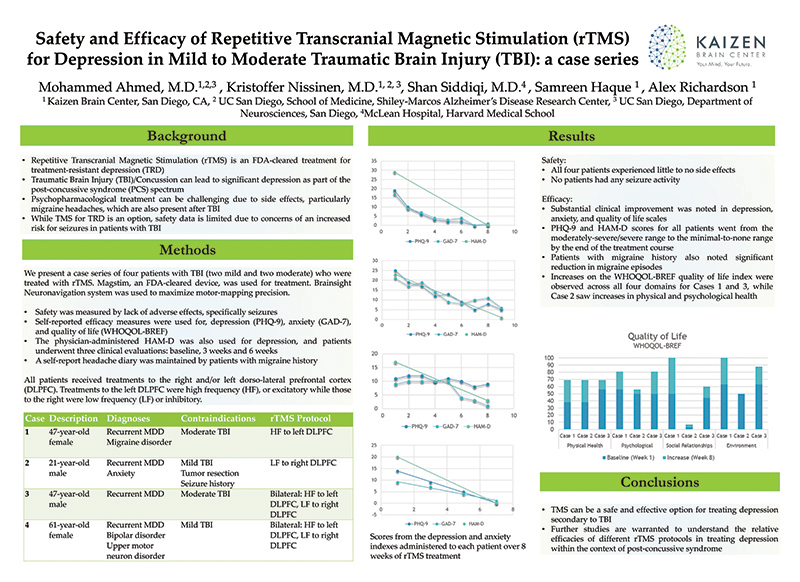 Likewise, if the subject was a Control Test based on recent work 11,13,19,20, the results are repeated, thus more than a 10% decrease should be considered indicative of an abnormal test. Individual practitioners should use their clinical judgment when making a diagnosis 21.
Likewise, if the subject was a Control Test based on recent work 11,13,19,20, the results are repeated, thus more than a 10% decrease should be considered indicative of an abnormal test. Individual practitioners should use their clinical judgment when making a diagnosis 21.
When the * A and response tests along with all three concussion tasks are completed, the subject has multiple cognitive systems assessed: Motor, Vision, Left and Right Symmetry, Memory. executive functions, multitasking, and consistency across five tasks.It will take about eight minutes to complete all five tests. Close observation of the suspected concussion patient may provide additional information regarding the execution of the subject 22. For example; Missing button bias can be observed in some post-concussion subjects suggesting visual field deficits or peripheralization. Peripheralization is typically used by neurological and allied healthcare professionals to describe a common phenomenon where a patient uses one side more than the other.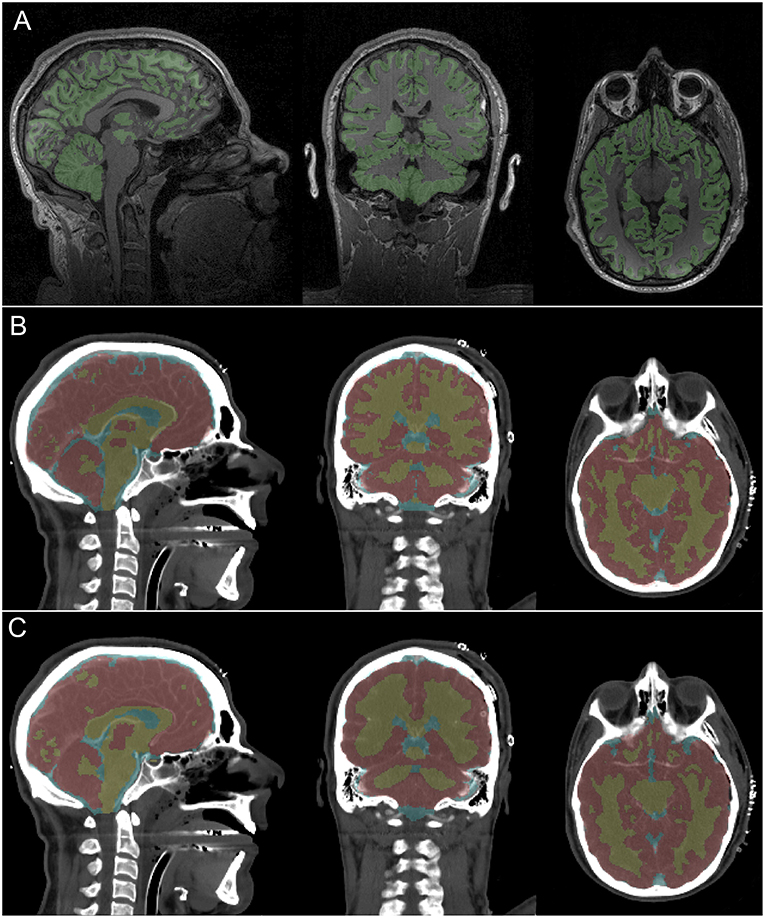 It includes hemiparesis, neglect and transformation disorders. The sum of these observations can be used by the diagnostic physician to make an assessment of the cognitive status of the subjects.
It includes hemiparesis, neglect and transformation disorders. The sum of these observations can be used by the diagnostic physician to make an assessment of the cognitive status of the subjects.
Interpretation of binocular measurements
Perceive the distance of an object or its depth of field, the brain uses the Angles of the Vergent eyes “and size information to determine the distances. The brain uses the angles of the eyes” to estimate the distance. This information, for the baseball player, is important in determining the speed and trajectory of the ball; whether it be a field, throw or hit.Stereo Fly aims to appreciate the depth of perception of the mastery of convergence. Vision training improves the perception of the depth of this measure and expansion, can help by increasing their ability to assess the characteristics of the ball in flight. Baseball players use and need depth perception from distance ( fielders, etc.), and up close (hitters and infielders) to maintain field awareness and optimal performance.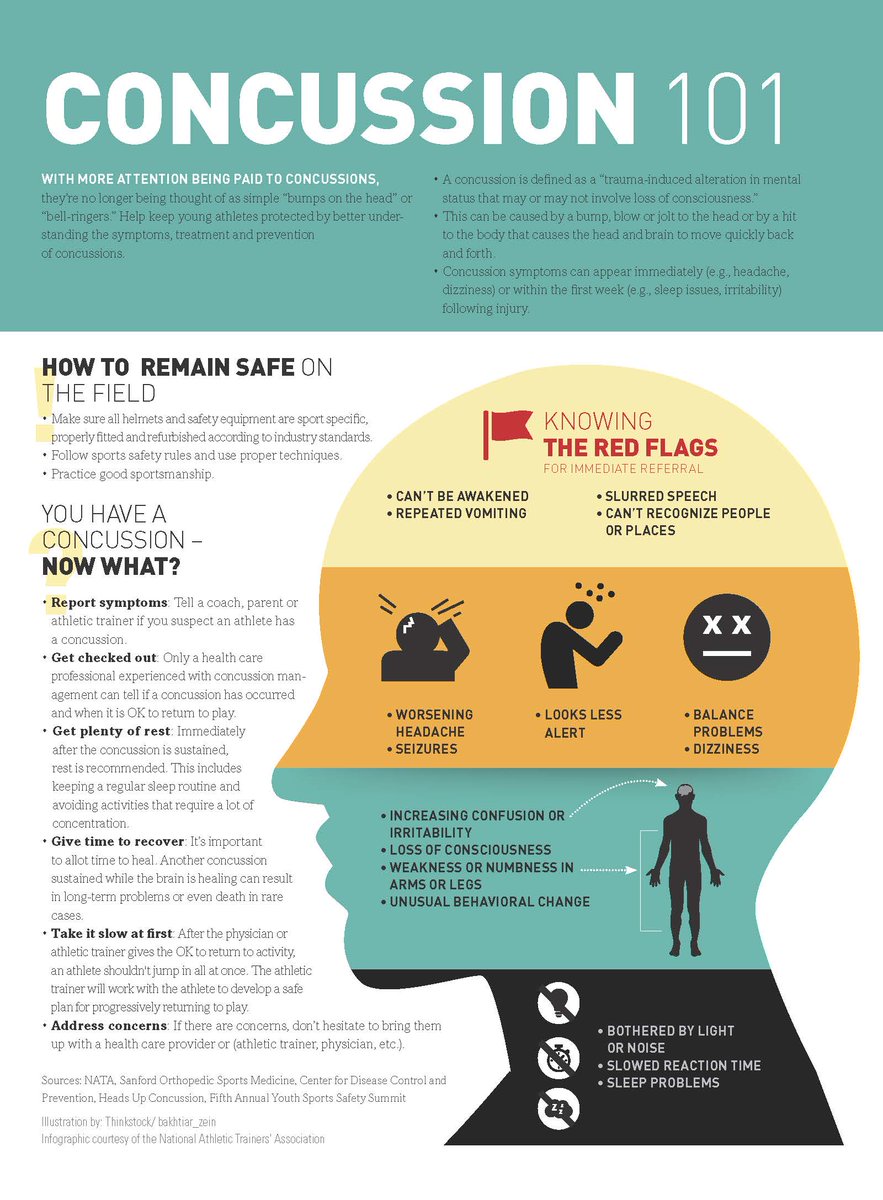 Improved depth perception for the test may mean that it is less likely to be misleading for an upward change in the 23-25 field.
Improved depth perception for the test may mean that it is less likely to be misleading for an upward change in the 23-25 field.
Assuming that learning has a vision of causation in relation to observed binocular changes, it begs the question why this might happen. It is possible that vision training, which includes motor and ophthalmic neuro-visual conditioning, results in an improvement in the coarse and fine motor control of the extra eyepiece and inside the ocular muscles of the eyes. This probably includes improved proprioception. The eyes can more accurately “focus” on a point, stay there with a good “eye of discipline” and give the brain better information about convergence.Hence the brain improves depth perception. To a certain extent in the players, this can help raise awareness of where that point is in physical space. It is likely that the Stereo Fly results were improved because the ability to detect angles for triangulation was better. This can occur with improved proprioception of the muscles of the eyeball, and / or improved accuracy as in the position of the eyes. The timing of improvement is consistent with the effect of muscle training. As mentioned in the results, the players are consistently come in season with a binocular of 23.7 mm and six weeks of training increases this binocular and improve to 36.9 mm.Players return from the offseason, and after not doing vision training for six months plus with binocular numbers similar to their original. This suggests that there is an effect of getting off the train in the absence of a vision preparation.
The timing of improvement is consistent with the effect of muscle training. As mentioned in the results, the players are consistently come in season with a binocular of 23.7 mm and six weeks of training increases this binocular and improve to 36.9 mm.Players return from the offseason, and after not doing vision training for six months plus with binocular numbers similar to their original. This suggests that there is an effect of getting off the train in the absence of a vision preparation.
Neurovisual processing combined with ocular motor proprioception It is believed to improve the perception of stereo depth, that is, the ability to use convergence angles to perceive depth 8.26. This improvement is lost during the off-season, which is consistent with the drop-off effect.At this time, we cannot determine if prolonged continuous vision training for many years will provide more beneficial, as we see, disembarkations when vision training is discontinued after the season. In any case, vision training has obvious positive results. Continued or regular training of vision can restore and / or maintain them, furthermore.
In any case, vision training has obvious positive results. Continued or regular training of vision can restore and / or maintain them, furthermore.
Troubleshooting. Vision and / or eye exercises can often cause eye fatigue or headaches.This is probably due to the type of DOMS and should be considered normal but resolved before the start of the season. This is also an important reason why you should start before the start of the season and be in the maintenance phase of the season. Reducing or modifying your workout can reduce eye fatigue that should occur. If headache or discomfort persists, eye care and or treating physician should be consulted.
Limitations
The limitation of the study is that it takes time to do the training and preparation should begin before the start of the season.If possible, it is better to have raw data on subjects, but with large teams that are often difficult. Some tasks have disadvantages with pre-existing ocular motor problems. For example double vision due to “cross eyed” cast can be exorbitant with Brock’s string. Therefore, good eye health and tolerance ranges should be checked by a qualified ophthalmologist or ophthalmologist before starting a vision training regimen.
Therefore, good eye health and tolerance ranges should be checked by a qualified ophthalmologist or ophthalmologist before starting a vision training regimen.
This report provides a unique perspective on improving depth perception of tall caliber athletes following vision training.A previous paper indicated improved performance with vision training 3, and current results confirm the training vision for improved performance. Emerging evidence also suggests that depth perception and vision learning can continue to improve in terms of performance enhancement as well as injury prevention 7.
As we have seen improvements in reaction time and improved peripheral vision we attribute these in part to improvements in brain processing.We believe that the improvement in visual acuity cannot explain changes such as processing the brain need to have eyes coordination of the hands S urinated changes. As for the peripheral visual fields, the cones and rods of the retina may be functional, but the brain does not process these signals to the fullest extent. Vision training, which results in improved peripheral vision, is likely to occur along with constitutive processing of brain changes. Future research to evaluate changes in the brain with visual training to better address this.
Vision training, which results in improved peripheral vision, is likely to occur along with constitutive processing of brain changes. Future research to evaluate changes in the brain with visual training to better address this.
Future work is to better optimize the methods used to improve certain tasks, and that indicators for use in monitoring the success of vision teaching methods are warranted.
Subscription Required. Please recommend JoVE to your librarian.
Opposition received a heavy blow – Society – Kommersant Novosibirsk
An attack on Nadezhda Kosenkova and Alexei Panshin, organizers of the opposition rallies “For Fair Elections”, took place in Kemerovo.Doctors diagnosed the first with a concussion, and the second with a broken nose. The victims believe that the cause of the incident is their social activities.
The attack on Aleksey Panshin and Nadezhda Kosenkova, chairman of the executive committee of the regional branch of the Union of Right Forces, and Nadezhda Kosenkova took place at 23. 15 last Friday on the ground floor of house No. 15 on Oktyabrsky Prospekt in Kemerovo. “We returned home, waited for the elevator. At that moment, without any warning, two people attacked us, apparently already waiting at the entrance.They inflicted several blows, knocked down, and began to kick. They managed to see one: a middle-aged, dark-haired man. The second was behind him, and his appearance was not remembered, ”said Mr. Panshin.
15 last Friday on the ground floor of house No. 15 on Oktyabrsky Prospekt in Kemerovo. “We returned home, waited for the elevator. At that moment, without any warning, two people attacked us, apparently already waiting at the entrance.They inflicted several blows, knocked down, and began to kick. They managed to see one: a middle-aged, dark-haired man. The second was behind him, and his appearance was not remembered, ”said Mr. Panshin.
According to the oppositionist, “the attackers did not try to rob.” “All personal belongings remained with us, we raised a cry, after which they quickly retreated,” he explained. Alexey Panshin considers the attack planned and purposeful. “They beat me exclusively in the face, not a single hit in the body – they obviously wanted to ruin the face on the eve of our planned picket on Saturday in defense of the Krasnoyarsk opposition leader Oleg Leontyev,” the activist said.
Alexey Panshin and Nadezhda Kosenkova are known in Kemerovo as organizers of the protests that took place in the city at the end of last year and the first half of this year. The rallies “For Fair Elections” on December 10 and 28 brought together about 500 participants, marches and rallies on March 5 and May 6 – 70-80 each.
The rallies “For Fair Elections” on December 10 and 28 brought together about 500 participants, marches and rallies on March 5 and May 6 – 70-80 each.
Immediately after the attack, the opposition tried to call a police squad, but the officer on duty invited them to come to the “Central” department themselves. “Only four hours later, and only after our numerous calls and calls from our acquaintances, the district officer on duty from this department arrived and received my statement about the attack and explanations,” explained Alexey Panshin.When asked why there was no police for so long, the district police officer, according to the victim, replied that “there were too many corpses that night”. In the summaries of the main department of the Ministry of Internal Affairs for the Kemerovo region and the regional investigation department of the TFR, there are no reports of serious crimes of a violent nature in the regional center on weekends.
By the time the district police officer arrived, the victims had already gone to an ambulance. Doctors discovered that Nadezhda Kosenkova had a concussion and hospitalized her in the neurosurgical department of one of the city hospitals.In addition to abrasions and bruises, Alexei Panshin was found to have a closed fracture of the nasal bones without displacement.
Doctors discovered that Nadezhda Kosenkova had a concussion and hospitalized her in the neurosurgical department of one of the city hospitals.In addition to abrasions and bruises, Alexei Panshin was found to have a closed fracture of the nasal bones without displacement.
On Saturday, a regular district militia officer conducted a survey of Nadezhda Kosenkova. At what stage is the investigation of the incident, Alexey Panshin could not say yesterday.
The regional headquarters of the Ministry of Internal Affairs yesterday refused to officially comment on the attack on Alexei Panshin and Nadezhda Kosenkova. According to Kommersant’s information, a pre-investigation check is being carried out on this case. Mr. Panshin has already passed the forensic medical examination, Mrs. Kosenkova is not yet.Depending on the results of the examination, the issue of initiating a criminal case will be resolved.
Igor Lavrenkov, Kemerovo
90,000 IFAB clarified hand play and approved testing of additional concussion substitutions
World football experts have brought some clarity to a controversial point among fans.
theifab.com
05 March 2021, 15:56
On the agenda of the 135th annual meeting of the International Football Association (IFAB) Council, which was held in the format of a videoconference, the key issue was the consideration of issues related to clarifying the interpretation of episodes with a handball by field players, as well as the need to introduce additional substitutions for a case if a football player receives a concussion during the fight.
Particular attention was paid to the Laws of the Game, and specifically to Rule No. 12 “Violations and Misdemeanors”, within the framework of which the general interpretations of the hand game by footballers were fixed.
The members of the meeting agreed that not every handball on the part of a field footballer should be interpreted as a violation of the rules. As for the episodes with “unnatural increase in body volume”, the experts confirmed the exclusiveness of the personal referee’s interpretation for such situations, which should be based on the position of the limb of the body prohibited for play in relation to the ball’s flight path in each individual situation.
As a result, the following situations were considered a violation of the rules:
– a player deliberately touches the ball with his hand, for example, moving his hand / arm entirely in his direction;
– touches the ball with his hand, and at the same time his body grows unnaturally in size.
At the same time, it is considered that the player has unnaturally increased his body in size, if the position of his hand does not correspond to and is not justified by the trajectory of body movement in a particular situation.
By placing his hand in such a position, the player independently creates the risk of the ball hitting it, therefore, can be punished by the referee, depending on the situation on the field.
However, from now on, if the ball is directly in the goal from an accidental contact of the hand of a team-mate of an attacking player, the referee is obliged to score a goal in favor of the attacking team, ignoring the fact that the ball hits a part of the body prohibited for play.
A similar interpretation of the situation will now be relevant in the event that an accidental hit of the ball in the hand of a team-mate has led to the creation of a goal-scoring situation for the attacking team.
Also, the council approved the clarifications to Rule No. 11 “Determination of the game boundaries of body parts”, according to which the arm ends at the base of the armpit, which is also used when fixing an offside position by the side referees and the VAR panel.
Council members also welcomed the results of the year-long testing of additional concussion-related footballers’ concussion replacements, extending the mandate for these studies until August 2022, while alerting all associations to the need to prepare for the practice in the future.
Regarding the temporary amendments to Rule 3 “On Substitutions”, thanks to which the organizers of competitions have the right to increase the number of substitutions for teams to five per game, the council members agreed that until the COVID-19 pandemic subsided, there is no reason to talk on the abolition of this practice.
However, the end dates: December 31, 2021 for club football and July 31, 2022 for international, were not renewed at this meeting.
For a more detailed review and discussion of the changes made to the Rules of the Game, the functionaries allocated one month more time to the associations, setting the date of entry into force of the new edition of the rules for July 1, 2021, instead of the usual June 1, while retaining the right to make adjustments.
90,000 A teenager with aortic dissection was rescued in St. Petersburg State Medical University
The child had an accident on the eve of the New Year holidays.On December 31, doctors of the Pediatric University, together with colleagues from the Mariinsky Hospital and the City Multidisciplinary Hospital No. 2, performed a rare operation.
road accidents occurred on December 27 in the Lomonosov district of the Leningrad region. The taxi, in the back seat of which 14-year-old Daniil Mikhailov and his father were peacefully sleeping, drove into the oncoming lane and collided with a passenger minibus.
– A second before the accident, I woke up and saw that the driver had closed his eyes.I wanted to wake him up, but didn’t manage to , – said the boy. |
From the impact, he flew into the front of the cabin and hit the torpedo with his chest. This, probably, was the cause of the most severe trauma – tearing of the aortic wall. Doctors later also diagnosed the child with a ruptured subcapsular hematoma of the spleen, contusion of the lung and liver, and concussion. However, Daniel was able to get out of the car on his own.
– I got out in front – the windshield was gone.Found dad, patted him on the shoulder – he mumbled something in response. I thought – alive, already good. |
The victim was taken to the Children’s City Multidisciplinary Clinical Center for High Medical Technologies named after Rauchfus. There, using computed tomography, doctors revealed a dissection of the thoracic aorta with the formation of a pseudoaneurysm – in other words, a pulsating hematoma.Even a small jump in blood pressure could lead to her rupture, massive internal bleeding and death.
For further treatment, it was decided to transfer the patient to the Pediatric University.
| | – The child was lucky that there was no complete rupture of the aorta at the time of the accident or on the first day after it , – explained the head of the cardiac surgery department of the Mariinsky Hospital, associate professor of the Department of Cardiovascular Surgery at St. |
Doctors could either monitor the patient’s condition, in the hope that the tear would heal itself over time, or perform endoprosthetics of the thoracic aorta and exclude the aneurysm from the bloodstream.
– All specialists came to the conclusion that it is necessary to apply active surgical tactics to eliminate this problem.This point of view was adhered to by our cardiac surgeons and vascular surgeons, and the doctors with whom we consulted , – said the head of the department of X-ray surgical methods of diagnostics and treatment of St. Petersburg State Pedagogical University Mikhail Komissarov . |
The surgery was performed in two stages. A stent graft, a metal frame covered with a special hermetic polymer, had to be implanted into the aorta. But, according to the doctors’ calculations, this design was supposed to block the subclavian artery, which would lead to a disruption of the blood supply to the brain.
A stent graft, a metal frame covered with a special hermetic polymer, had to be implanted into the aorta. But, according to the doctors’ calculations, this design was supposed to block the subclavian artery, which would lead to a disruption of the blood supply to the brain.
Therefore, at the first stage, SPbGPMU doctors, together with cardiovascular surgeons at the Mariinsky Hospital, formed a shunt to the subclavian artery from the neighboring carotid artery, thereby redistributing the blood flow. The operation was performed through a small incision above the child’s collarbone.
In case of complications, the doctors were ready at any time to begin a larger-scale intervention using artificial blood circulation. The main risk was associated with rupture of the aneurysm during surgery.There were other dangers as well.
| | – If the carotid artery was also closed at the stage of stent graft deployment, we would have performed an operation to replace it through a sternotomy (sternum incision). |
A number of difficulties were associated with the installation of a stent graft.
– These operations are often performed on adult patients. But in children, such interventions are extremely rare. A stent graft is a large device that is placed through large delivery systems. A stent of a suitable size was only recently released on the market, and it was a great success that the manufacturer was able to promptly provide it to us , – said Mikhail Komissarov. |
The second stage of the operation was carried out by the doctors of the Pediatric University together with the specialists of the City Multidisciplinary Hospital No. 2. Invaluable help to the SPbSPMU doctors was provided by the head of the department of X-ray endovascular methods of diagnostics and treatment of GMPB No. “ Evgeniy Shloydo .
2. Invaluable help to the SPbSPMU doctors was provided by the head of the department of X-ray endovascular methods of diagnostics and treatment of GMPB No. “ Evgeniy Shloydo .
Both phases of the operation took place on the last day of 2020. Now Daniel has already been transferred to a regular ward, he is preparing for discharge.
– Many friends and acquaintances call us who are worried about Dan. It seems to me that they do not fully understand the gravity of the situation in which my son was. At first, I myself did not fully understand how difficult the operation was, which was done to him, what a huge risk it was. Fortunately, the doctors did not refuse us, and I am very grateful to all of them , – says the boy’s mother Olga Mikhailova . |
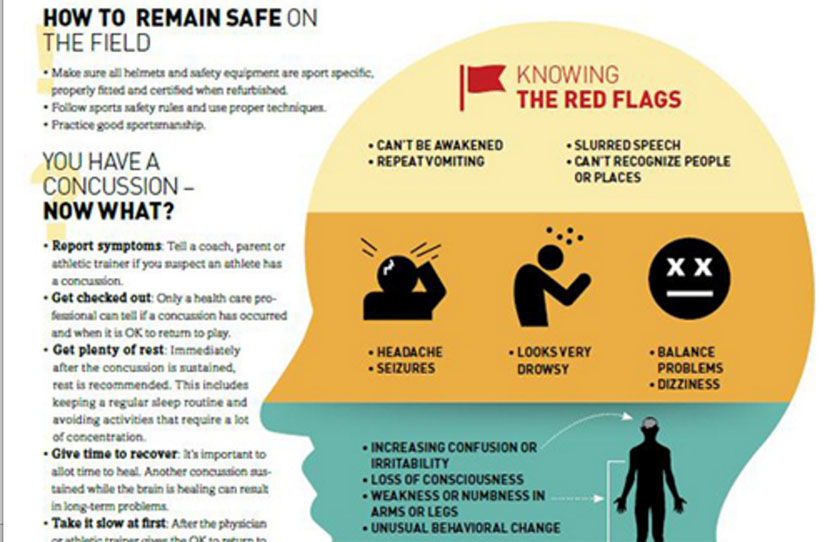 g., cranial nerve deficits)
g., cranial nerve deficits) Then I sat and waited for an ambulance, which was called by one of the passengers on the bus. I did not lose consciousness , – Daniel shared.
Then I sat and waited for an ambulance, which was called by one of the passengers on the bus. I did not lose consciousness , – Daniel shared. Petersburg State Pedagogical University Magomedemin Askerov .
Petersburg State Pedagogical University Magomedemin Askerov . But, fortunately, we managed to implement the plan that was initially outlined by cardiovascular and endovascular surgeons , – Magomedemin Askerov said.
But, fortunately, we managed to implement the plan that was initially outlined by cardiovascular and endovascular surgeons , – Magomedemin Askerov said.