How do concussion laws vary across US states. What are the key components of concussion legislation for schools. How do return-to-play and return-to-learn policies differ by state. What are the education requirements for concussion awareness in schools.
Overview of Concussion Legislation in the United States
Concussion management in youth sports has become a critical concern across the United States. As of 2024, all 50 states have implemented some form of legislation regarding sport-related concussions. This widespread adoption of concussion laws marks a significant step forward in protecting young athletes from the potentially severe consequences of traumatic brain injuries.
The genesis of this nationwide legislative movement can be traced back to May 2009, when Washington State passed the groundbreaking “Zackery Lystedt Law.” This pioneering legislation was the first to mandate a “removal and clearance for Return to Play” protocol for youth athletes suspected of sustaining a concussion. The Lystedt Law served as a catalyst, inspiring similar legislation across the country.

Key Components of Concussion Legislation
While concussion laws vary from state to state, they typically address several core areas:
- Removal from play protocols
- Return-to-play requirements
- Medical clearance standards
- Concussion education and awareness
- Scope of schools affected
- Return-to-learn policies
Understanding these components is crucial for physical educators, coaches, school administrators, and parents to ensure compliance with state regulations and to provide optimal care for student-athletes.
Removal from Play and Return-to-Play Protocols
One of the most critical aspects of concussion management is the immediate removal of a potentially concussed athlete from play. As of June 2017, 48 states required that students suspected of sustaining a concussion be removed from play for the remainder of the day or for at least 24 hours. This precautionary measure is essential to prevent further injury and allow for proper assessment.
Variations in Return-to-Play Timelines
While most states adhere to a minimum 24-hour removal period, some have implemented more stringent guidelines:

- Arizona and South Carolina: Allow same-day return if cleared by a healthcare professional
- California: Mandates a minimum seven-day return-to-play period
- New Mexico: Requires a ten-day minimum before return-to-play
These variations highlight the importance of staying informed about specific state regulations. Do longer mandated return-to-play periods lead to better outcomes for concussed athletes? While more research is needed, erring on the side of caution with extended recovery periods aligns with current best practices in concussion management.
Graduated Return-to-Play Strategy
The 2016 Berlin Guidelines, which represent the international consensus on concussion management, recommend a graduated return-to-play strategy. This approach typically involves a five-day progression of increasingly demanding activities before full return to play. How does this graduated strategy benefit recovering athletes? It allows for a controlled and monitored return to physical activity, reducing the risk of re-injury and ensuring that the athlete is fully prepared for the demands of their sport.
Medical Clearance Requirements for Return-to-Play
All states require some form of medical clearance before a student-athlete can return to play following a concussion. However, the specifics of who can provide this clearance vary significantly from state to state.
Categories of Medical Clearance Providers
States generally fall into one of three categories regarding who can provide medical clearance:
- Licensed physicians only (MDs or DOs)
- Select providers only (may include physicians, nurse practitioners, physician assistants, or neuropsychologists)
- Any provider trained in concussion management
Why is there such variation in medical clearance requirements? The differences often reflect a balance between ensuring high-quality care and addressing the practical realities of healthcare access, especially in rural or underserved areas.
Written vs. Verbal Clearance
Another important distinction in state laws is whether medical clearance must be provided in writing. While some states explicitly require written clearance, many do not specify the format. How does this impact the return-to-play process? Written clearance provides a clear record and may offer additional legal protection for schools and healthcare providers, but it may also introduce delays in the return-to-play process.

Concussion Education and Awareness Requirements
As of June 2017, all states mandated some form of concussion awareness or education. However, the specific requirements vary widely in terms of who must receive education, how often it must be provided, and what content must be covered.
Target Groups for Concussion Education
Depending on the state, concussion education may be required for various stakeholders:
- Students
- Parents
- Coaches
- Healthcare professionals
- Physical educators
- Referees
Why is comprehensive education across all these groups important? Concussion recognition and management is a shared responsibility. By educating all stakeholders, states aim to create a culture of safety and awareness that can lead to better outcomes for student-athletes.
Frequency and Content of Education
The frequency of required education ranges from annual updates to one-time sessions. Content typically covers concussion recognition, immediate response protocols, and the potential long-term effects of concussions. How can schools ensure that concussion education remains effective over time? Regular refresher courses and updates on the latest research can help maintain awareness and improve compliance with best practices.

Scope of Schools Affected by Concussion Legislation
The applicability of concussion laws varies significantly across states, both in terms of the types of schools affected and the grade levels covered.
Public vs. Private Schools
As of June 2017, approximately 80% of state concussion laws applied only to public schools, while about 20% included private and charter schools. Why does this disparity exist? Public schools are more directly under state control, making it easier to implement and enforce legislation. However, the exclusion of private schools from these laws may create gaps in protection for a significant number of student-athletes.
Grade Levels Covered
The grade levels affected by concussion legislation also vary:
- 25% of states: Public high schools only
- 25% of states: Public middle and high schools
- 50% of states: All grades (K-12)
What are the implications of these differences in coverage? While older students may be at higher risk due to participation in contact sports, younger students are also vulnerable to concussions. Comprehensive coverage across all grade levels ensures that all students receive appropriate protection and care.

Return-to-Learn Policies in Concussion Legislation
While return-to-play protocols have been a primary focus of concussion legislation, there is growing recognition of the importance of “return-to-learn” policies. These policies address the cognitive challenges students may face when returning to academic activities following a concussion.
State Adoption of Return-to-Learn Policies
As of June 2017, 12 states had incorporated return-to-learn language into their concussion laws, either in the original legislation or through subsequent amendments. Why is there a growing emphasis on return-to-learn policies? Research has shown that cognitive rest and a gradual return to academic activities are crucial for optimal recovery from concussions.
Components of Return-to-Learn Policies
Effective return-to-learn policies typically include:
- Individualized academic accommodations
- Gradual increase in cognitive workload
- Coordination between medical providers and school personnel
- Monitoring of symptoms during the return-to-learn process
How can schools effectively implement return-to-learn policies? Close collaboration between educators, school nurses, counselors, and medical professionals is essential to create a supportive environment for recovering students.

Implementation and Evaluation of Concussion Laws
The passage of concussion legislation is only the first step in protecting student-athletes. Effective implementation and ongoing evaluation are crucial to ensure that these laws achieve their intended goals.
Case Study: Washington and Massachusetts
The National Center for Injury Prevention and Control (NCIPC) conducted a case study evaluation of Return to Play implementation efforts in Washington and Massachusetts. These states were chosen for their early adoption of concussion laws and the differences in their implementation approaches.
Key Factors in Successful Implementation
The case study evaluation revealed several factors that contribute to successful implementation of concussion laws:
- Clear roles and responsibilities for stakeholders
- Robust education and training programs
- Effective communication channels between schools, healthcare providers, and families
- Regular monitoring and enforcement mechanisms
- Flexibility to adapt to new research and best practices
What challenges do states face in implementing concussion laws? Common obstacles include limited resources, inconsistent application of protocols, and difficulties in reaching all relevant stakeholders with education and training.
Future Directions in Concussion Legislation and Management
As our understanding of concussions continues to evolve, so too must the legislation and policies designed to protect student-athletes. Several key areas are likely to shape the future of concussion management in schools:
Emerging Research and Technology
Advancements in neuroimaging, biomarker research, and wearable technology are opening new avenues for concussion diagnosis and monitoring. How might these developments impact concussion legislation? Future laws may incorporate requirements for using validated assessment tools or may set standards for the use of new technologies in concussion management.
Expanding Focus on Non-Sports Concussions
While current legislation primarily focuses on sports-related concussions, there is growing recognition of the need to address concussions from other causes, such as playground accidents or non-sports activities. How can schools adapt their policies to cover all types of concussions? Comprehensive protocols that apply to all students, regardless of the cause of injury, may become the new standard.

Long-Term Monitoring and Support
As awareness grows about the potential long-term effects of concussions, future legislation may include provisions for extended monitoring and support of students with a history of concussions. What might this long-term care look like? It could involve regular check-ups, ongoing academic accommodations, or mental health support services.
In conclusion, the landscape of concussion legislation in U.S. schools is complex and ever-evolving. While significant progress has been made in protecting student-athletes, there remains considerable variation in state laws and room for improvement in implementation. As research advances and our understanding of concussions deepens, we can expect further refinements in legislation and management practices. The ultimate goal remains constant: to ensure the safety and well-being of all students, both on and off the playing field.
Concussion Legislation by State/SHAPE America
Today, all 50 states have some form of legislation regarding sport-related concussion.1 Because such policies vary widely, physical education teachers and other school personnel should take the time to understand their state and local concussion policies in addition to their school policy.2 Typically, this information can be found through each state’s official government website.
The following images provide a quick overview of several components of state concussion policy. This information is current as of June 2017.
As of June 2017, 48 states require that students suspected of sustaining a concussion be removed from play for the remainder of the day, or 24 hours. Arizona and South Carolina allow such athletes to return to play the same day if cleared by a healthcare professional.
The consensus from the Berlin Guidelines is for a graduated return-to-play strategy, typically of five days.3 Two states mandated longer periods of time for returning to play (California, seven days; New Mexico, 10 days).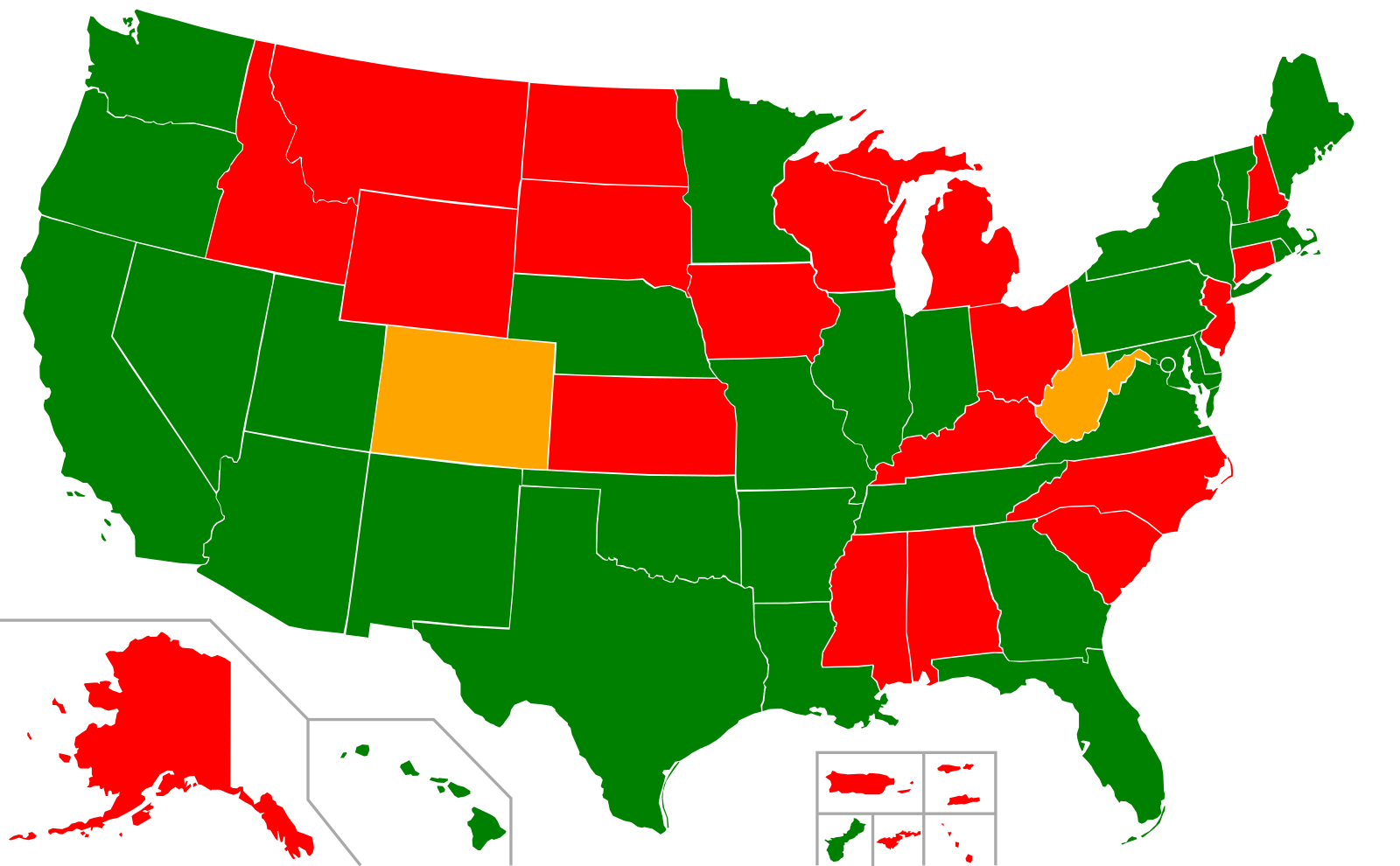
Clearance can be given only by licensed physicans (MDs or DOs).
Clearance can be given by select providers only.
Clearance can be given by any provider trained in concussion management.
As of June 2017, all states require medical clearance before a student may return to play. Physical educators should learn what kind of healthcare professionals are legally allowed to provide medical clearance in their state. Note: Some states specify that such clearance is to be written, while many states do not.
Education Requirements
Require some type of concussion awareness or education.
As of June 2017, all states require some type of concussion awareness or education, although many of the requirements are ambiguous as to who should receive such education and how often. Concussion-education requirements for students, parents, coaches, healthcare professionals, physical educators and referees vary from state to state. It is important for physical educators to learn and follow their state and school policies regarding concussion education.
Types of Schools Affected by State Concussion Legislation
State concussion legislation affects both public and private schools.
State concussion legislation affects public schools only.
State concussion legislation affects grades K-12.
State concussion legislation affects middle school and high school only.
State concussion legislation affects high school only.
As of June 2017, about 25% of state concussion laws applied to only public high schools, another 25% applied to public middle and high schools, and 50% applied to all grades (K-12). Only about 20% of state concussion laws applied to private and charter schools.
Return to Learn
Concussion laws include language regarding return-to-learn policy, either in original or amended legislation.
Concussion laws do not include language regarding return-to-learn policy, either in original or amended legislation.
As of June 2017, 12 states had concussion laws that included language regarding return-to-learn policy.
References:
1Potteiger, K., Potteiger, A., Pitney, B. & Wright, P. M. (2018). An examination of concussion legislation in the United States. Internet Journal of Allied Health Sciences and Practice, 16(2), Article 6.
2Roetert, E. P. & Richardson, C. (2014). What every educator should know about concussions. Principal Leadership, March, 18-20.
3McCrory, P., Meeuwisse, W., Dvořák, J., et al. (2017). Consensus statement on concussion in sport- the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine, 51: 838-847. Retrieved from http://bjsm.bmj.com/content/51/11/838.
Sports Concussion Policies and Laws | HEADS UP
In May 2009, the State of Washington passed the “Zackery Lystedt Law” to address concussion management in youth athletics.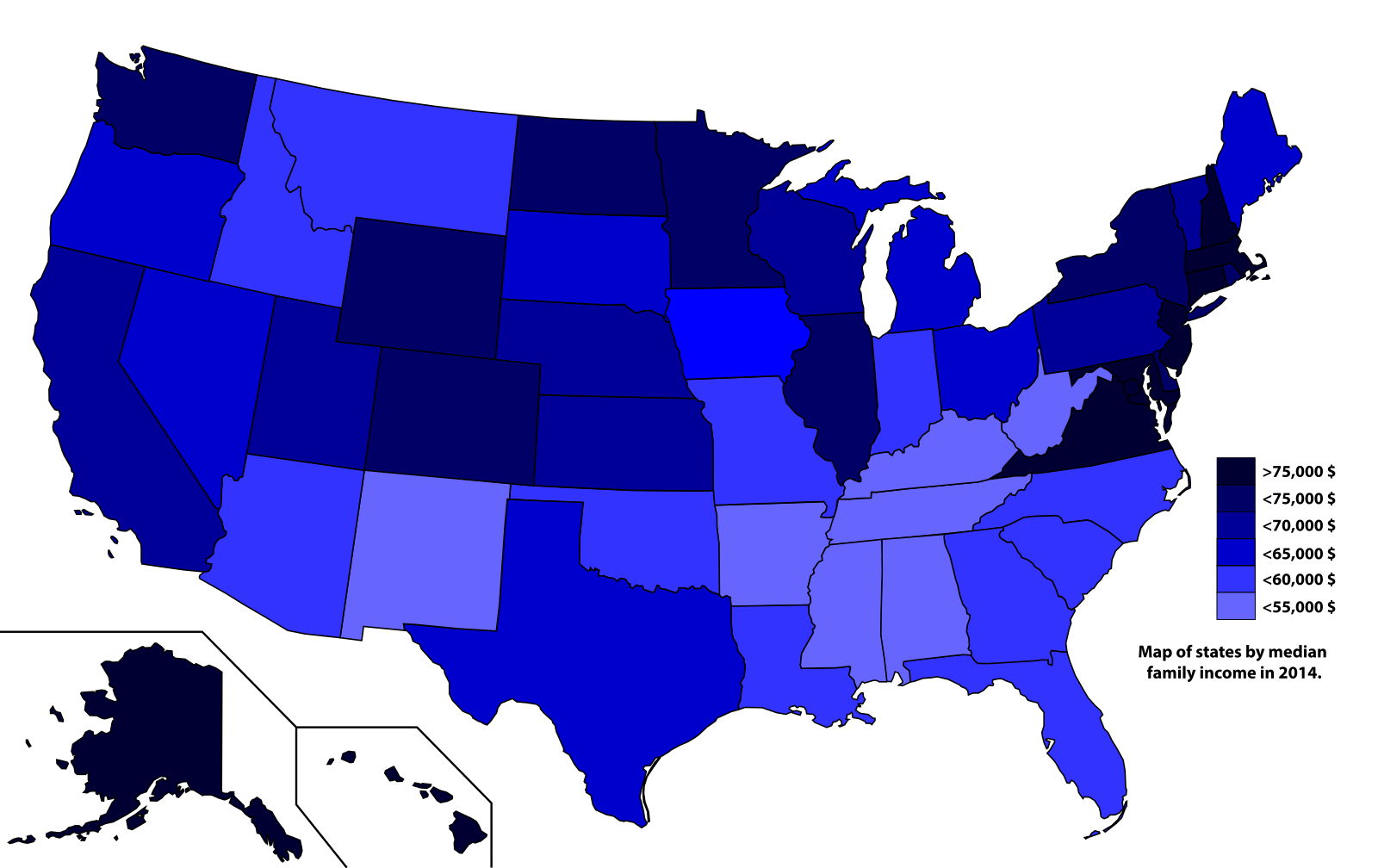 The Washington law was the first state law to require a “removal and clearance for Return to Play” among youth athletes. Now all 50 states have a Return to Play law.
The Washington law was the first state law to require a “removal and clearance for Return to Play” among youth athletes. Now all 50 states have a Return to Play law.
In order to assess the implementation of Return to Play laws, the National Center for Injury Prevention and Control (NCIPC) conducted a case study evaluation on the Return to Play implementation efforts in two states: Washington and Massachusetts. These two states were selected because they were both early adopters of Return to Play and because their laws varied on several important dimensions, including the role of the health department and other stakeholder groups. The evaluation was designed to assess implementation efforts, including related challenges and successes in implementation.
Return to Play laws include a variety of different components that can be complicated to implement, such as removal from play, collection of concussion histories, required training for different stakeholders, etc. Additionally, Return to Play laws do not always provide specific guidance on how each of the components of the laws should be carried out. Some laws identify a specific entity, such as a state agency, to develop regulations and other laws are less specific. As a result, implementers are sometimes required to make decisions after the law has passed that can have an impact on successful implementation. Thoroughly considering the logistics of implementation and engaging in a robust planning process can help increase the consistency and quality of implementation.
Some laws identify a specific entity, such as a state agency, to develop regulations and other laws are less specific. As a result, implementers are sometimes required to make decisions after the law has passed that can have an impact on successful implementation. Thoroughly considering the logistics of implementation and engaging in a robust planning process can help increase the consistency and quality of implementation.
Based on the experiences of the stakeholders interviewed in Massachusetts and Washington, there are a number of key considerations for the implementation of Return to Play. The guide presents considerations, as well as lessons learned from state stakeholders and potential barriers to implementation, in the following areas:
- Stakeholder Roles and Responsibilities
- Implementation Requirements
- Knowledge and Awareness
- Medical Clearance
- Supporting and Monitoring Implementation
- Planning Ahead to Evaluate the Impact of Return to Play
Traumatic Brain Injury Legislation
Table of Contents
Contact
Traumatic Brain Injury (TBI) is caused by a bump, blow, or jolt to the head that disrupts brain functioning. The leading causes of TBI are falls, being struck by or against objects and motor vehicle crashes. TBIs range from mild (a brief disruption in consciousness) to severe (prolonged unconsciousness or amnesia). While a majority of the TBIs that occur each year are mild—commonly referred to as concussions—many are severe and occasionally lead to permanent disability or death. In 2013, there were approximately 2.8 million TBI-related emergency department (ED) visits, hospitalizations and deaths in the United States.
The leading causes of TBI are falls, being struck by or against objects and motor vehicle crashes. TBIs range from mild (a brief disruption in consciousness) to severe (prolonged unconsciousness or amnesia). While a majority of the TBIs that occur each year are mild—commonly referred to as concussions—many are severe and occasionally lead to permanent disability or death. In 2013, there were approximately 2.8 million TBI-related emergency department (ED) visits, hospitalizations and deaths in the United States.
In addition to the emotional burden of TBIs, the economic burden of TBIs in the United States is estimated to be approximately $76.5 billion. Programs and services that support TBI patients are funded through various federal and state sources. For example, Medicaid Home- and Community-Based Services (HCBS) waivers are active in 47 states and the District of Columbia and fund cost-effective services to those at risk of being institutionalized due to a medical condition. At least 22 states utilize a HCBS waiver to extend benefits and services to certain patients with TBI.
Many states aim to prevent TBIs as well as effectively diagnose and rehabilitate TBI patients. Between 2009 and 2015, 50 states and the District of Columbia passed laws to address traumatic brain injury. The majority of states enacted legislation targeting youth sports-related concussions. According to the Youth Risk Behavior Survey, sports-related concussions affected about 2.5 million high school students in 2017. Other introduced legislation addresses traumatic brain injury in veterans, appropriates funds to traumatic brain injury prevention or treatment programs, and requires insurers, hospitals and health maintenance organizations to provide insurance coverage for survivors of traumatic brain injury.
Return to the injury and violence prevention overview page to learn about other topics and additional resources.
Below is a list of enacted legislation between 2009 and 2014 to address traumatic brain injury. To view state actions from 2015 onward related to TBI and other injury and violence prevention topics, please visit NCSL’s Injury and Violence Prevention Legislation Database.
The box allows you to conduct a full text search or use the dropdown menu option to select a state.
Additional Resources
NCSL Resources
Other Resources
*External links are included for informational purposes only and do not imply an endorsement of the content.
It is time to rewrite state youth sports concussion laws
Key points
Return-to-learn procedures can facilitate recovery for children and adolescents reintegrating into school postconcussion.
Although all states and the District of Columbia have youth sports concussion legislation, few of these laws address return-to-learn.
All state youth concussion laws should address return-to-learn, with provisions for postconcussion school reintegration for all students, not just student athletes.
Traumatic brain injury (TBI) results from a bump, blow or jolt to the head that affects brain function. 1 In 2014, there were 837 000 TBI-related emergency department visits, hospitalisations and deaths among children ≤17 years in the USA.1 Of these, 23 000 children were hospitalised and 2529 died because of TBI alone or in conjunction with other injuries.1
1 In 2014, there were 837 000 TBI-related emergency department visits, hospitalisations and deaths among children ≤17 years in the USA.1 Of these, 23 000 children were hospitalised and 2529 died because of TBI alone or in conjunction with other injuries.1
The importance of appropriate management of youth concussion in sports has received significant attention from medical professionals, public health institutions, schools, state legislators, sports organisations, parents and researchers. Between 2009 and 2014, all 50 states and the District of Columbia passed legislation to improve the recognition and management of youth concussed in sports.2 These laws can include mandates such as requiring periodic concussion training for school athletic personnel, educating students and their parents about concussion, return-to-play (RTP) procedures and medical clearance for RTP.
Most TBIs among children are mild and are commonly called concussions. Symptoms of concussion for most youth typically resolve within 28 days of injury,3 but symptoms can last longer. One study found that 1 month postconcussion, nearly 25% of young patients (11–22 years) with concussion reported headache, >20% reported fatigue and nearly 20% reported slower cognitive processing.4 While symptomatic, concussion can be a serious health problem that can affect a young person’s physical and mental status, with implications for performance of daily activities, including academics.3–14 Postconcussion outcomes in children and adolescents include a range of somatic (eg, headache, fatigue), cognitive (eg, attention deficits, forgetfulness, slowed processing) and affective (eg, irritability, disinhibition) symptoms.5 6 11 Learning new materials or remembering previously learnt material can pose challenges to students returning to school postconcussion.9 School environment (bright lights, computer screens, between-class crowded hallways and noisy cafeterias) can trigger or aggravate postconcussion symptoms.5 These symptoms can negatively impact academic performance. In a study that followed 349 children and adolescents (5–18 years) with concussion, actively symptomatic students reported significantly more school-related problems than recovered peers.
One study found that 1 month postconcussion, nearly 25% of young patients (11–22 years) with concussion reported headache, >20% reported fatigue and nearly 20% reported slower cognitive processing.4 While symptomatic, concussion can be a serious health problem that can affect a young person’s physical and mental status, with implications for performance of daily activities, including academics.3–14 Postconcussion outcomes in children and adolescents include a range of somatic (eg, headache, fatigue), cognitive (eg, attention deficits, forgetfulness, slowed processing) and affective (eg, irritability, disinhibition) symptoms.5 6 11 Learning new materials or remembering previously learnt material can pose challenges to students returning to school postconcussion.9 School environment (bright lights, computer screens, between-class crowded hallways and noisy cafeterias) can trigger or aggravate postconcussion symptoms.5 These symptoms can negatively impact academic performance. In a study that followed 349 children and adolescents (5–18 years) with concussion, actively symptomatic students reported significantly more school-related problems than recovered peers. Greater severity of postconcussion symptoms was associated with significantly more school-related problems and significantly worse academic performance, regardless of time since injury.8
Greater severity of postconcussion symptoms was associated with significantly more school-related problems and significantly worse academic performance, regardless of time since injury.8
Return-to-learn (RTL) procedures are intended to mitigate concussion symptoms and accelerate recovery as concussed students reintegrate into school. These protocols can take the form of ‘academic adjustments’, ‘academic accommodations’, or ‘academic modifications’.9 ‘Academic adjustments’ refer to non-formalised environmental adjustments that do not involve classroom work (eg, reduced exposure to light and sound stimuli).9 ‘Academic accommodations’ include extra time for assignments and changes in class and exam schedules.9 ‘Academic modifications’ involve more permanent changes to an education plan, which are formalised in an Individualised Education Plan, pursuant to the Federal Individuals with Disabilities Education Act, or a 504 Plan, pursuant to the Federal Rehabilitation Act and the Americans with Disabilities Act. 9
9
Despite the potential impact of concussion on learning and school performance, a 2016 review of state youth concussion laws found that only eight states included provisions for RTL.2 Several other states have since amended their youth concussion laws to address this gap.14 Most states, however, do not mandate RTL as part of youth concussion legislation. In the absence of mandates, some schools have, by policy or initiative of school personnel, provided RTL protocols for their concussed students.
While acknowledging the lack of definitive efficacy research on components of RTL plans, various medical, public health and research organisations have endorsed RTL strategies for ameliorating individual students’ symptoms throughout the recovery period. These organisations include the American Academy of Pediatrics,7 9 the 5th International Conference on Concussion in Sport (Berlin 2016),10 the American Medical Society for Sports Medicine11 and the Centers for Disease Prevention and Control. 12 Nonetheless without legislation, schools vary in terms of the consistency, scope and quality of RTL procedures. A 2015 study of RTL procedures in public schools in Washington state (which does not provide for RTL in its youth sports concussion legislation) found that only 12% of schools reported a formal RTL policy; 67% had informal policies and 30% of teachers reported receiving no formal concussion training, even though approximately half reported having had a child with concussion in their class at some point.15
12 Nonetheless without legislation, schools vary in terms of the consistency, scope and quality of RTL procedures. A 2015 study of RTL procedures in public schools in Washington state (which does not provide for RTL in its youth sports concussion legislation) found that only 12% of schools reported a formal RTL policy; 67% had informal policies and 30% of teachers reported receiving no formal concussion training, even though approximately half reported having had a child with concussion in their class at some point.15
Of the eight states identified in the 2016 study as having youth concussion laws that address RTL, only three applied RTL procedures to all students with concussion, without regards to concussion mechanism or precipitating activity.2 Some states that have since amended their youth concussion laws to include RTL have mandated it only for student atheletes.14 Yet, it is evident that many youth concussions occur during activities other than sports, such as non-sports falls, bicycle and other vehicular crashes, or fighting. Several studies have examined the proportion of medically treated youth concussions that are sports-related (SR) versus non-SR (NSR). One study that used the National Hospital Ambulatory Medical Care Survey, which sampled 600 randomly selected US hospital Emergency Departments (EDs) and ambulatory care clinics, estimated that between 2002 and 2006, 70% of youth (0–19 years) presenting with concussions at hospital EDs and ambulatory care clinics had an NSR concussion.16 A second study that examined medical records of a sample of patients (0–17 years) treated for concussion between 2012 and 2014 at a large, urban, paediatric hospital and associated suburban practices found that 30% of concussions were NSR.17 A third study that examined medical records of Medicaid-insured patient (0–18 years) treated for concussion at a paediatric accountable care organisation between 2008 and 2017 also found that 70% of the concussions were NSR.18 A fourth study of 13 291 children (5–19 years) presenting for TBI at a level 1 trauma centre between 2002 and 2011 found that 71.
Several studies have examined the proportion of medically treated youth concussions that are sports-related (SR) versus non-SR (NSR). One study that used the National Hospital Ambulatory Medical Care Survey, which sampled 600 randomly selected US hospital Emergency Departments (EDs) and ambulatory care clinics, estimated that between 2002 and 2006, 70% of youth (0–19 years) presenting with concussions at hospital EDs and ambulatory care clinics had an NSR concussion.16 A second study that examined medical records of a sample of patients (0–17 years) treated for concussion between 2012 and 2014 at a large, urban, paediatric hospital and associated suburban practices found that 30% of concussions were NSR.17 A third study that examined medical records of Medicaid-insured patient (0–18 years) treated for concussion at a paediatric accountable care organisation between 2008 and 2017 also found that 70% of the concussions were NSR.18 A fourth study of 13 291 children (5–19 years) presenting for TBI at a level 1 trauma centre between 2002 and 2011 found that 71. 7% had NSR injuries.19
7% had NSR injuries.19
Differences in estimates of the relative proportions of SR and NSR concussions among children and adolescents may be due to differences in how investigators classified concussions (eg, sports and recreation related vs organised SR) and whether caregivers recorded injury activity as well as mechanism (eg, a fall could occur during an SR or NSR activity).20 Regardless of the exact proportions of SR to NSR concussions, all concussed students should have the opportunity to benefit from RTL procedures. As Yeates notes: ‘Even if only a small proportion of children with mild TBI suffer negative outcomes, then mild TBI is a serious public health problem’.5 As state concussion laws evolve, revisions should include RTL procedures that apply to all students, however their concussion occurred.
Revising state youth concussion laws to mandate RTL provisions for all students may specifically benefit low-income students and students of colour because there is evidence that these students are less apt than their more affluent or white peers to have SR concussions. 17 19 In a retrospective review of youth concussion mechanisms, Haarbauer-Krupa et al found that children with private insurance were 1.4 (95% CI 1.25 to 1.62) times as likely to have an SR concussion than children who were Medicaid beneficiaries or who were self-pay.17 Non-Hispanic Black children were less likely (RR 0.80; 95% CI 0.71 to 0.91) to have SR concussion than non-Hispanic White children.17 A similar study of youth concussion mechanisms by Hanson et al found that Medicaid and self-pay children were significantly more likely than children with private insurance to have an NSR concussion (86% vs 66%; p<0.000) and that African American children were significantly more likely than Caucasian children to have NSR concussions (81% vs 68%; p<0.000).19
17 19 In a retrospective review of youth concussion mechanisms, Haarbauer-Krupa et al found that children with private insurance were 1.4 (95% CI 1.25 to 1.62) times as likely to have an SR concussion than children who were Medicaid beneficiaries or who were self-pay.17 Non-Hispanic Black children were less likely (RR 0.80; 95% CI 0.71 to 0.91) to have SR concussion than non-Hispanic White children.17 A similar study of youth concussion mechanisms by Hanson et al found that Medicaid and self-pay children were significantly more likely than children with private insurance to have an NSR concussion (86% vs 66%; p<0.000) and that African American children were significantly more likely than Caucasian children to have NSR concussions (81% vs 68%; p<0.000).19
In a 2018 commentary, several prominent scholars of youth concussion have argued that expanding concussion laws to incorporate RTL mandates is not necessary.21 These authors note that Colorado and Pennsylvania, which do not have RTL legislation, have implemented statewide RTL programmes through collaborations between state Departments of Education and Health. 21 In their review of state youth concussion laws, Thompson et al noted that Oregon, Pennsylvania and Colorado have strong RTL programmes without legislation.2 Nonetheless, these latter authors conclude that legislative action on RTL and improved integration of laws and research are needed. We agree. The passage of RTP legislation by all 50 states and the District of Columbia demonstrates that the political will to address youth concussion exists. Revising these laws to include RTL will ensure that procedures are implemented; it will enhance consistency with best practices and it will provide for accountability in implementation of mandates. Notwithstanding the success of a few states in addressing RTL without legislation, these states are the exceptions. Without legislated mandates under-resourced schools are less apt to implement RTL programmes due to lack of funding and personnel, thus compounding the existing disparities in concussion management due to racial and income differences in SR versus NSR concussions.
21 In their review of state youth concussion laws, Thompson et al noted that Oregon, Pennsylvania and Colorado have strong RTL programmes without legislation.2 Nonetheless, these latter authors conclude that legislative action on RTL and improved integration of laws and research are needed. We agree. The passage of RTP legislation by all 50 states and the District of Columbia demonstrates that the political will to address youth concussion exists. Revising these laws to include RTL will ensure that procedures are implemented; it will enhance consistency with best practices and it will provide for accountability in implementation of mandates. Notwithstanding the success of a few states in addressing RTL without legislation, these states are the exceptions. Without legislated mandates under-resourced schools are less apt to implement RTL programmes due to lack of funding and personnel, thus compounding the existing disparities in concussion management due to racial and income differences in SR versus NSR concussions. It is time to revise state laws to: (1) include provisions for RTL and (2) apply these provisions to all students, athletes and non-athletes, regardless of how, when or where their concussion occurred.
It is time to revise state laws to: (1) include provisions for RTL and (2) apply these provisions to all students, athletes and non-athletes, regardless of how, when or where their concussion occurred.
CONCUSSION LEGISLATION
Evaluation and management of concussion in student athletes is an important area of practice for many neuropsychologists, and in recent years, concern about the safety of student athletes has entered into our national dialogue. The Zackery Lystedt Law passed in 2009 in Washington State in response to a young man who was severely disabled after he sustaining a brain injury during a football game and returning to play after halftime, resulting in experiencing significant and disabling complications. It is viewed as a “model law” for other states to follow in creating legislation to protect student athletes from negative outcomes of returning to play when still symptomatic.
The law includes Zackery Lystedt Brain Project’s Three Principles:
- Education for coaches, athletes, and parents/guardians
- Removal from play for athletes suspected of sustaining a concussion or head injury
- No return to play until the athlete is evaluated by a licensed health care provider (LHCP) trained in the evaluation and management of concussion and receives written clearance.

Most states have laws that vary in the degree to which they cover the three principles and in the degree to which they allow neuropsychologists to make independent return to play decisions. The NAN LAAC has been involved in advocating for the independent practice of neuropsychologists by writing letters of support or suggestions for changes, offering meetings with key legislators, sending action alerts to members, and coordinating efforts with other professional organizations. Examples of letters and a spreadsheet with state laws are available to NAN members.
Click here to login to your member account to view the following:
- Letter 1 to Senator Vitale
- Letter 2 to Senator Vitale
- Letter to Senator Durbin
- Letter to Assemblyman Diegnan
- Letter to Education Policy Associate Broughnan
- State Laws Spreadsheet
Resources:
Concussions in Youth Athletes – Little League
The Youth Sports Concussion Safety Act is found at 410 ILCS 145/1, et seq. under the Illinois Public Health Law at the section dealing with Health Prevention and Protection.
under the Illinois Public Health Law at the section dealing with Health Prevention and Protection.
Under the Act “Sponsored youth sports activity” means any athletic activity, including practice or competition, for players under the direction of a coach, athletic director, or band leader of a youth sports league, including, but not limited to, baseball, basketball, cheerleading, cross country track, fencing, field hockey, football, golf, gymnastics, ice hockey, lacrosse, marching band, rugby, soccer, skating, softball, swimming and diving, tennis, track (indoor and outdoor), ultimate Frisbee, volleyball, water polo, wrestling, and any other sport offered by a youth sports league.
This Act applies to any sponsored youth sports activity sponsored or sanctioned by a youth sports league beginning or continuing after January 1, 2016 and is not applicable to interscholastic athletic activity, which is defined in the Illinois School Code (105 ILCS5/22-80). 410 ILCS 145/10.
The law defines Player and Youth sports league, respectively, as follows:
“Player” means an adolescent or child participating in any sponsored youth sports activity of a youth sports league. 410 ILCS 145/5.
410 ILCS 145/5.
“Youth sports league” means any incorporated or unincorporated, for-profit or not-for-profit entity that organizes and provides sponsored youth sports activities, including, but not limited to, any athletic association, organization, or federation in this State that is owned, operated, sanctioned, or sponsored by a unit of local government or that is owned, operated, sanctioned, or sponsored by a private person or entity, as well as any amateur athletic organization or qualified amateur sports organization in this State under the U.S. Internal Revenue Code (26 U.S.C. Sec. 501(c)(3) or Sec. 501(j)). 410 ILCS 145/5.
Section 410 ILCS 145/15 provided in relevant part that:
Each youth sports league with players who participate in any youth-sponsored sports activity sponsored or sanctioned by the youth sports league is encouraged to make available, electronically or in writing, to coaches, game officials, and players, as well as the parents/ guardians, and other persons with legal authority to make medical decisions, educational materials that describe the nature and risk of concussions and head injuries, including the advisability of removal of players that exhibit signs, symptoms, or behaviors consistent with a concussion, such as a loss of consciousness, a headache, dizziness, confusion, or balance problems, from participating in a youth-sponsored sports activity sponsored or sanctioned by the youth sports league.
Any park district is authorized and encouraged to make available to residents and users of park district facilities, including a youth athletic program, education materials with regard to the nature and risks of concussions and is subject to and shall comply with the requirements of the Youth Sports Concussion Safety Act, if the park district is directly responsible for organizing and providing a sponsored youth sports activity as a youth sports league by registering the players and selecting the coaches, as those terms are defined in the Youth Sports Concussion Safety Act [410 ILCS 145/1 et seq.]. 70 ILCS 1205/8-24.
The Illinois Law regarding concussions as related to interscholastic athletic activity can be found at 105 ILCS 5/22-80 of the Illinois School Code and 105 ILCS 25/1.15 and 105 ILCS 25/1.20 of the Interscholastic Athletic Organization Act.
410 ILCS Section 145/1 et seq. can be viewed online at:
http://ilga.gov/legislation/ilcs/ilcs3.asp?ActID=3652&ChapterID=35
70 ILCS Section 1205/8-24 can be viewed online at:
http://ilga.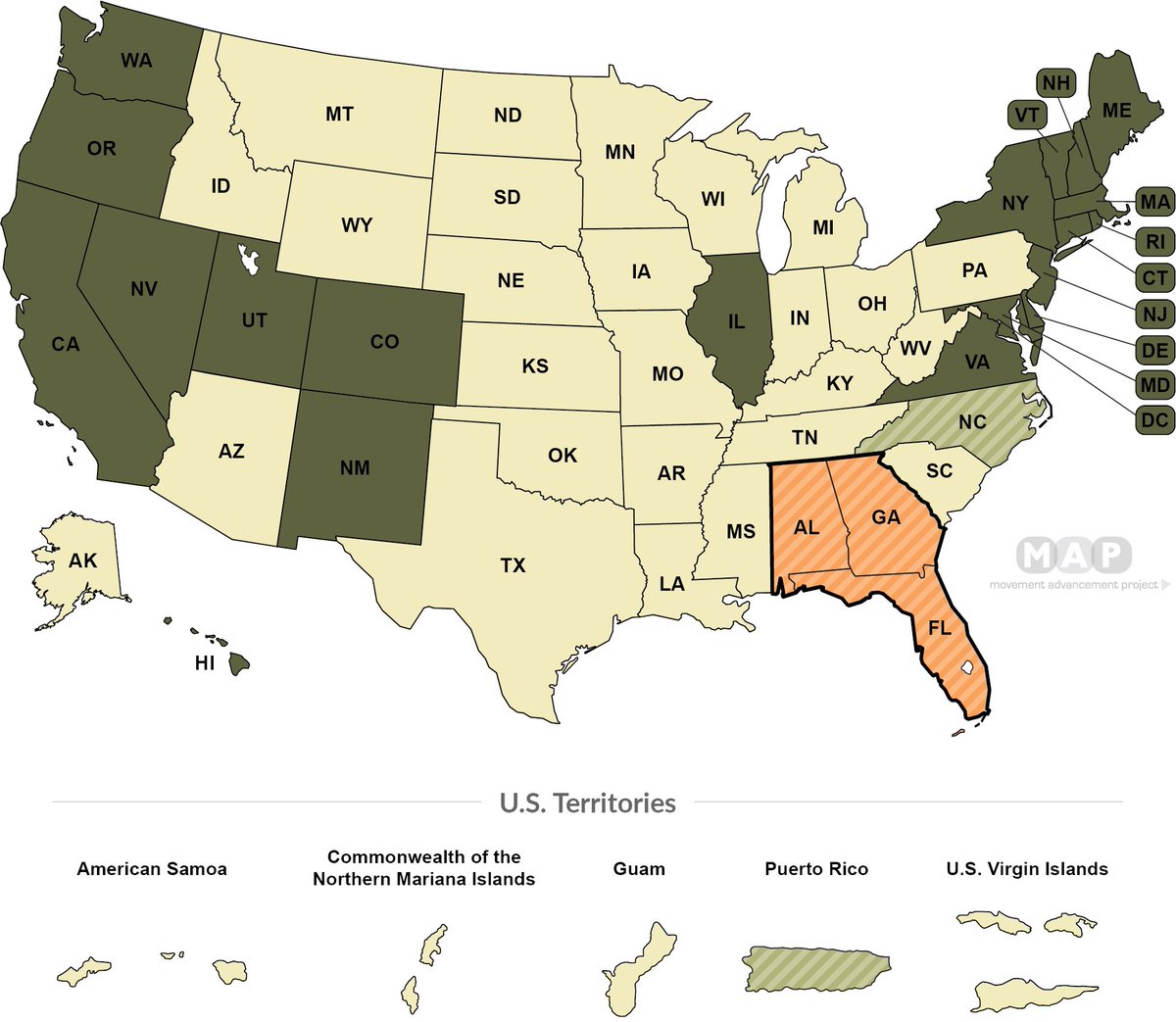 gov/legislation/ilcs/ilcs4.asp?DocName=007012050HArt%2E+8&ActID=892&ChapterID=15&SeqStart=10200000&SeqEnd=14200000 (ctrl F search concussion).
gov/legislation/ilcs/ilcs4.asp?DocName=007012050HArt%2E+8&ActID=892&ChapterID=15&SeqStart=10200000&SeqEnd=14200000 (ctrl F search concussion).
105 ILCS Section 5/22-80 of the Illinois School Code and 105 ILCS Section 25/1.15 and 105 ILCS Section 25/1.20 of the Interscholastic Athletic Organization Act can be viewed online at:
http://ilga.gov/legislation/ilcs/documents/010500050K22-80.htm
http://ilga.gov/legislation/ilcs/ilcs3.asp?ActID=1009&ChapterID=17
http://www.ilga.gov/legislation/ilcs/documents/010500250K1.20.htm
Section 20 ILCS 2310/2310-307 of the Department of Public Health Powers and Duties Law of Civil Administrative Code of Illinois can be viewed online at:
http://www.ilga.gov/legislation/ilcs/fulltext.asp?DocName=002023100K2310-307
The following website offers additional information regarding Illinois concussion laws:
https://www.ihsa.org/Resources/Sports-Medicine/Concussion-Management
TN Sports Concussion Law
In April 2013, Tennessee became the 44th state to pass a sport concussion law designed to reduce youth sports concussion and increase awareness of traumatic brain injury.
The legislation, Public Chapter 148 and Public Chapter 948 has three key components:
· To inform and educate coaches, youth athletes and their parents and require them to sign a concussion information form before competing.
· To require removal of a youth athlete who appears to have suffered a concussion from play or practice at the time of the suspected concussion.
· To require a youth athlete to be cleared by a licensed health care provider* before returning to play or practice.
· *Health care provider means a Tennessee licensed medical doctor, osteopathic physician, clinical neuropsychologist with concussion training, or physical assistant with concussion training who is a member of a health care team supervised by a Tennessee licensed medical doctor or osteopathic physician.
Below you will find links for the required forms, trainings and guidelines that will equip coaches, parents and athletes to recognize and respond to sports related concussions:
Sample Policy
Parent Athlete Signature Form
Coach Signature Form
Return to Learn/Return to Play: Concussion Management Guidelines PDF
Training Resources
The following trainings have been approved by the Department of Health as concussion recognition and head injury safety education online course. Completion of one of the trainings on an annual basis fulfills the requirement of training for all coaches and athletic directors as required by the Tennessee Youth Sports Concussion Law.
Completion of one of the trainings on an annual basis fulfills the requirement of training for all coaches and athletic directors as required by the Tennessee Youth Sports Concussion Law.
HEADS UP to Youth Sports: Online Training
https://www.cdc.gov/headsup/youthsports/training/index.html
National Federation of State High School Associations
https://nfhslearn.com/?courseid=38000
National Alliance for Youth Sports
https://www.nays.org/additional-training/preview/concussion-training.cfm
Tennessee Athletic Trainer’s Society
https://sportsafety.com/Tennessee/
USA Football
https://sportsafety.com/Tennessee/
Additional Sports Safety Recognition
The Safe Stars Initiative recognizes youth sports leagues throughout Tennessee for providing the highest level of safety for their young athletes. Safe Stars consists of 3 levels: gold, silver, and bronze, and involves implementation of policies around topics such as concussion education, weather safety and injury prevention. For more information about Safe Stars, please visit https://www.tn.gov/health/health-program-areas/fhw/vipp/safe-stars-initiative.
For more information about Safe Stars, please visit https://www.tn.gov/health/health-program-areas/fhw/vipp/safe-stars-initiative.
90,000 Medical myths: is it dangerous to let someone get a concussion to sleep?
- Claudia Hammond
- BBC Future
Photo author, Getty Images
It is said that a person with a concussion should never fall asleep – there is a risk that sleep will pass into a coma. Observer BBC tried to figure out how true this statement is.
Concussion has recently become a major concern with debate over whether athletes with head injuries should be allowed to return to professional sports.
Many argue that the short and long term consequences of traumatic brain injury should be taken more seriously.
At the same time, the majority share the dubious concept that a person who has been hit on the head should never be allowed to fall asleep, otherwise he will sink into a coma.
However, such recommendations can no longer be heard from modern doctors, since there is no evidence to support the validity of this thesis.
A concussion is an injury that occurs as the result of a severe blow to the head or a sudden and violent shock, such as in a car accident.
People who tend to take head injuries extremely seriously are quite right: these episodes can be very unfortunate, and one of the difficulties is that it is very difficult to diagnose the severity of the injury.
Photo Credit, Getty Images
Photo Caption,
Rugby is a sport with an increased risk of head injuries
In the United States of America alone, between 1.6 and 3 million head injuries are reported annually.
At the moment, doctors are forced to rely on characteristic symptoms to determine the severity of such an injury, which include vomiting, blurred consciousness, loss of balance, blurred vision or headaches, and tingling in the extremities.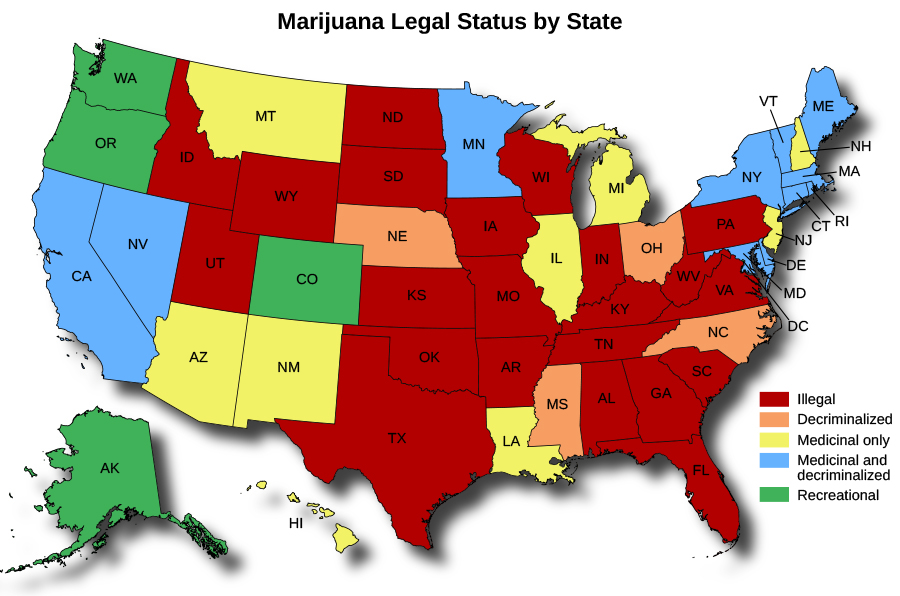
It is hoped that in the future, doctors will be able to detect concussion with a simple blood test that measures the level of certain substances in the bloodstream.
A group of researchers from the Regional Medical Center of St.Orlando, Florida, recently discovered two types of proteins that the brain secretes when damaged by a blow to the head.
However, it will take several more years to complete the research, and until then, doctors will have to rely on symptoms to determine the diagnosis.
The fear that a person with a head injury may fall asleep and not wake up is due to the fact that many do not fully understand the mechanism of the so-called lucid consciousness gap.
This is a rare occurrence and denotes a period of wakefulness between primary and secondary loss of consciousness.
At first, a person wakes up after an injury in a seemingly normal state, but at this time a hemorrhage, or hematoma, occurs in his brain, which puts pressure on the brain tissue.
And if, as a result of this hematoma, the victim again loses the creation, then here we can already talk about a threat to life.
However, even in the case of cerebral hemorrhage, the likelihood of an interval of clear consciousness remains extremely small.
Photo author, Getty Images
Photo caption,
During the first night after a traumatic brain injury in a child, his condition should be checked every few hours
However, the threat of a cerebral hemorrhage is the reason why it is so important to pay attention the symptoms listed above if you are dealing with someone who has just received a blow to the head.
This is what a wide variety of organizations recommend, from the World Rugby Association to the UK National Health Service.
But if a person does not experience clouding of consciousness, vomiting, double vision, impaired motor functions or acute pain in the head or neck, then there is no need to force him to stay awake.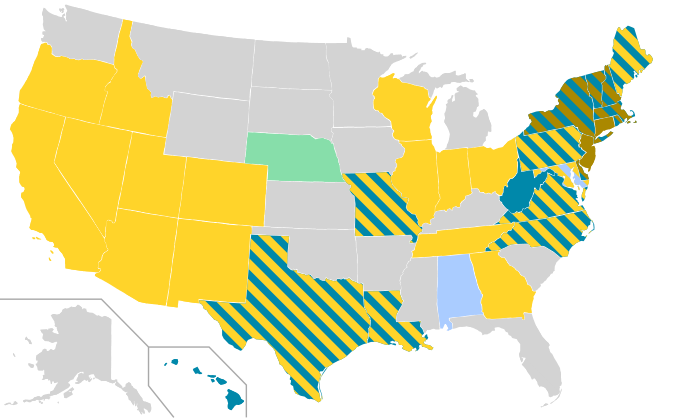
In reality, the victim, on the other hand, needs rest – both physically and mentally.
That is why athletes need to not only stop their training for a while, but also avoid intense mental efforts.
Children with concussion should reduce their schoolwork until they recover.
The brain is in need of recovery by reducing stress, and sleep is an ideal solution to this problem.
So for traumatic brain injury victims, sleep is a blessing, not a source of risk.
This is how the recommendations of modern specialists sound. However, it should be admitted that until recently, practically no tests were carried out to verify these or those recommendations, and this causes serious concern among a number of researchers.
On the positive side, several new tests have been registered and are being carried out to date. This means that there is a chance that in the near future there will be new information about the best treatment for concussion and the rules of caring for patients with head injury.
The word “concussion” is partly misleading and sounds so harmless that some doctors strongly recommend dropping it in favor of the term “head injury”.
However, a number of organizations do recommend waking a child every hour or two for the first night after a concussion if a child suffers from a traumatic brain injury to make sure he is feeling normal and able to maintain a coherent conversation. After that, you can allow the child to fall asleep again.
Thus, sleep is recommended for patients as one of the recovery measures, but this task itself is often difficult to accomplish.
Studies show that many patients develop sleep disorders after a concussion, including insomnia, fatigue, drowsiness, and in some cases even narcolepsy (a disorder that manifests itself in a frequent and uncontrollable desire to sleep) and apnea (stopping breathing) during sleep …
Legal information. This article is for general information only and should not be construed as a substitute for the advice of a physician or other healthcare professional. The BBC is not responsible for any diagnosis made by the reader based on the materials of the site. The BBC is not responsible for the content of other sites, links to which are present on this page , and also does not recommend commercial products or services mentioned on these sites.If you are concerned about your health condition, see your doctor.
The BBC is not responsible for any diagnosis made by the reader based on the materials of the site. The BBC is not responsible for the content of other sites, links to which are present on this page , and also does not recommend commercial products or services mentioned on these sites.If you are concerned about your health condition, see your doctor.
Zenit defender suffered a concussion in a street fight
In St. Petersburg, as a result of a fight that ended an ordinary road conflict, a player of the local football club Zenit Denis Terentyev was seriously injured. Due to a broken nose and a concussion, the athlete will no longer be able to enter the field this season. The police investigate the circumstances of the incident and establish the identity of the abuser of the football player.
Representatives of the football club told Kommersant that the incident took place on the evening of November 29 at house 20, building 3 on Laboratorny Prospekt. According to Denis Terentyev, at about 5 pm, the 25-year-old Zenit defender, returning from an autograph session in Pulkovo in his private car, was going to enter the courtyard of his house. But the passage was blocked by another car. The inexperienced girl driving the Mercedes did not figure out how to get away from the oncoming traffic. The footballer showed a possible movement option with a turn signal signal, but was not understood.He did not want to give way to the lady, but preferred to wait for the reaction of the owner of the oncoming foreign car. At this moment, he was allegedly approached by a passer-by who recommended that the athlete simply back up. In turn, Mr. Terentyev said that he would figure out the situation on his own and suggested that the interlocutor not interfere. Apparently, the pedestrian did not like the rebuke, and through an open window he stabbed a football club defender in the face. Subsequently, Denis Terentyev on his Instagram said that he tried to get out of the car in order to repulse the aggressor, but from that moment he did not remember anything.
According to Denis Terentyev, at about 5 pm, the 25-year-old Zenit defender, returning from an autograph session in Pulkovo in his private car, was going to enter the courtyard of his house. But the passage was blocked by another car. The inexperienced girl driving the Mercedes did not figure out how to get away from the oncoming traffic. The footballer showed a possible movement option with a turn signal signal, but was not understood.He did not want to give way to the lady, but preferred to wait for the reaction of the owner of the oncoming foreign car. At this moment, he was allegedly approached by a passer-by who recommended that the athlete simply back up. In turn, Mr. Terentyev said that he would figure out the situation on his own and suggested that the interlocutor not interfere. Apparently, the pedestrian did not like the rebuke, and through an open window he stabbed a football club defender in the face. Subsequently, Denis Terentyev on his Instagram said that he tried to get out of the car in order to repulse the aggressor, but from that moment he did not remember anything. He woke up in his car only a few minutes later.
He woke up in his car only a few minutes later.
Later, the post on Instagram was deleted by its owner at the request of the management of the football club – as overly emotional. The press secretary of Zenit Anton Makarenko told Kommersant that the injured footballer was hospitalized in the nearest hospital by an ambulance. Doctors diagnosed him with a broken nose and a concussion. Doctors will be able to finally assess the severity of traumatic brain injury in two to three days.But in any case, the athlete’s rehabilitation will take at least a month and he will have to miss the remaining games of this season. By the end of the year, Zenit will play two matches in the Russian championship and one match in the Europa League.
The injured defender reported to the police. Now law enforcement officers are checking these facts and finding out the circumstances of the incident. The issue of initiating a criminal case is being resolved.
Vladislav Litovchenko, St. Petersburg
90,000 Concussion – causes, symptoms, diagnosis and treatment
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-medication. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. For a diagnosis and correct prescription of treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. For a diagnosis and correct prescription of treatment, you should contact your doctor.
Concussion: causes, symptoms, diagnosis and treatment.
Definition
Concussion is a functionally reversible form of closed traumatic brain injury without organic damage to the brain, resulting from a bruise, impact, and, in rare cases, as a result of sudden movement of the head.
Causes of a brain concussion
A concussion can be the result of a traffic accident, falls, domestic, sports and industrial injuries, as well as injuries sustained as a result of street fights and collisions during mass events, exposure to a blast wave. Even a seemingly minor head injury can lead to a concussion. Thus, the fact of the presence of an injury may already indicate a possible concussion.
The mechanism of concussion is not exactly known. Most likely, as a result of trauma, certain problems arise with the functioning of the nerve cells of the brain (neurons). It is assumed that there is a functional disconnection between the brain stem and hemispheres. It is believed that due to a concussion, there is a temporary disruption of interneuronal connections. A slight displacement of the layers of brain tissue may appear, their nutrition may deteriorate and the connection between some brain centers may be disordered, which contributes to the development of functional disorders.In this case, macroscopic and histological changes in brain tissue are not detected.
Most likely, as a result of trauma, certain problems arise with the functioning of the nerve cells of the brain (neurons). It is assumed that there is a functional disconnection between the brain stem and hemispheres. It is believed that due to a concussion, there is a temporary disruption of interneuronal connections. A slight displacement of the layers of brain tissue may appear, their nutrition may deteriorate and the connection between some brain centers may be disordered, which contributes to the development of functional disorders.In this case, macroscopic and histological changes in brain tissue are not detected.
Concussion ranks first among all brain injuries. Most patients recover within 1–2 weeks.
If over time the patient’s condition continues to deteriorate, and more severe forms of traumatic brain injury are excluded, then it is necessary to look for other causes of the existing symptoms – psychological problems, mental illness, side effects of drugs or other concomitant diseases.
Classification of the disease
According to the International Classification of Diseases (ICD-10), concussion has a code S06.0. This nosology is one of the clinical forms of traumatic brain injury.
Depending on the severity of the patient’s condition and clinical symptoms, three degrees of concussion are distinguished.
Concussion, mild . The victim has no impairment of consciousness, but disorientation, headache, dizziness, and nausea may occur during the first 20 minutes after the injury.Then the general state of health returns to normal. A short-term increase in body temperature (37.1-38 ° C) is possible.
Moderate concussion . Although the victim does not lose consciousness, pathological symptoms such as headache, nausea, dizziness, and disorientation may occur. They all last more than twenty minutes. There may be short-term memory loss (amnesia), most often retrograde amnesia with the loss of a few minutes of memories prior to the trauma.
Severe concussion . It is necessarily accompanied by loss of consciousness for a short period of time, usually from several minutes to several hours. The victim does not remember what happened – retrograde amnesia develops. Pathological symptoms disturb a person for 1-2 weeks after injury (headache, dizziness, nausea, fatigue, disorientation, impaired appetite and sleep).
Concussion symptoms
Behavioral, emotional symptoms :
- drowsiness;
- increased fatigue or general weakness;
- irritability;
- depression;
- anxiety;
- excess sleep hours;
- Difficulty falling asleep.

Cognitive symptoms :
- retardation and impaired coordination of movements;
- short-term confusion of consciousness;
- delayed incoherent speech;
- difficulty concentrating;
- Difficulty memorizing.
Diagnosis of concussion
Diagnosis of concussion is established on the basis of anamnesis, examination and exclusion of a more severe traumatic brain injury.
The doctor examines the entire body of the patient for abrasions, bruises, joint deformities, changes in the shape of the chest and abdomen, bleeding.
In the first hours after a concussion, the victim’s pupils are dilated or narrowed – a traumatic brain injury of any severity leads to disruption of the nerve pathways responsible for the functioning of the eyes.The reaction of the pupils to light is normal. The victim complains of pain when moving the eyes to the sides, there is a small horizontal nystagmus (involuntary trembling movements of the eyeballs), if you take your eyes to the most extreme positions. There may be slight asymmetry of tendon reflexes, unsteadiness in the Romberg position (legs together, straight arms extended forward to a horizontal level, eyes closed). The level of consciousness is assessed on the Glasgow coma scale and is 14-15 points.
There may be slight asymmetry of tendon reflexes, unsteadiness in the Romberg position (legs together, straight arms extended forward to a horizontal level, eyes closed). The level of consciousness is assessed on the Glasgow coma scale and is 14-15 points.
The list of laboratory tests includes:
- general blood test;
There should be no specific changes in blood, urine, and cerebrospinal fluid during concussion.
Instrumental diagnostics includes:
- X-ray of the skull – with a concussion, there are no fractures of the skull bones;
Magnetic resonance imaging of the spine may be needed to rule out spinal problems.
Differential diagnosis is carried out with brain contusion, asthenic state of the patient, psychoemotional lability, alcohol intoxication, vegetative-vascular dystonia, post-convulsive syndrome.
Which doctors should I contact
If you have a concussion, you should see a trauma doctor. He examines the patient, collects anamnesis, checks reflexes, prescribes an X-ray of the skull, and if a more complex brain damage is suspected, he sends a consultation to
He examines the patient, collects anamnesis, checks reflexes, prescribes an X-ray of the skull, and if a more complex brain damage is suspected, he sends a consultation to
neurologist or neurosurgeon.
Indications for specialist consultation:
- consultation
otorhinolaryngologist in order to exclude pathologies of the ear, throat, nose; - consultation with an ophthalmologist in order to exclude or confirm violations on the part of the visual apparatus;
- consultation
a therapist with the aim of correcting the treatment of concomitant pathology; - consultation
surgeon, maxillofacial surgeon and other narrow specialists according to indications.
Treatment of concussion
If a concussion is suspected, first aid should be given to the victim, ensuring him complete rest. It is necessary to lay a person in a quiet darkened room, it is better to slightly raise his head. It is very helpful to apply cold compresses to the head. Patients with concussion should stay in bed for at least several days.
Patients with concussion should stay in bed for at least several days.
If you have a concussion, you should not read, listen to loud music, or watch TV.Drinking a lot is not recommended. Alcohol is strictly contraindicated!
For 12 weeks after the injury, the patient should be under the supervision of a doctor in order to assess his condition and a full return to daily activity. To date, there are no effective drugs that accelerate the recovery period.
From drugs used non-narcotic analgesics, tranquilizers, hypnotics, sedatives. This is usually enough.
In some cases, drugs are used to relieve cerebral edema, suppress the gag reflex, as well as antihistamines.If any autonomic symptoms are excessively expressed, then, for example, b-blockers may be required (with severe tachycardia and hypertension). They conduct courses of nootropic and metabolic therapy.
Hospitalization is indicated within three days after injury. The indication for emergency hospitalization is the fact of injury or the presence of severe cerebral and autonomic symptoms.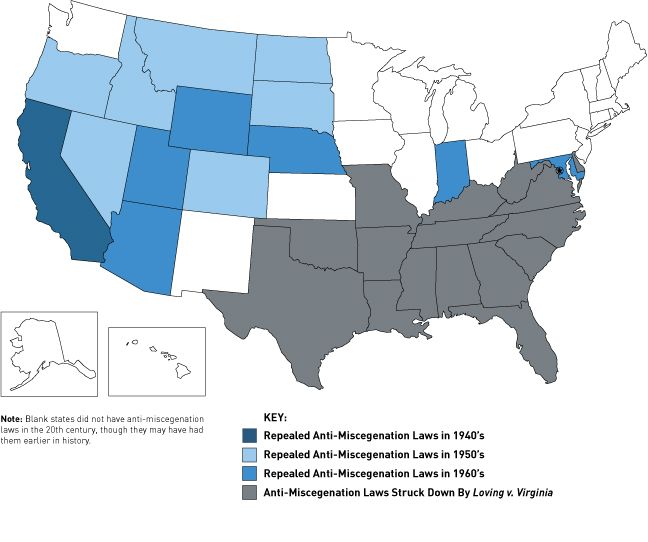
Complications
It must be remembered that a person who has suffered even a mild concussion may develop post-traumatic neurosis or other more serious complications, such as epilepsy.Approximately 3% of patients experience complications in the form of persistent asthenic syndrome, insomnia, migraines, intracranial hypertension and other conditions. Therefore, some time after recovery, you should definitely visit a neurologist and perform an electroencephalography.
The consequences of a concussion of the brain can appear after a few years, significantly complicating the usual life.
The hardest thing is for those who, for one reason or another, did not seek medical help in time for the timely diagnosis of the problems that have arisen.
Prevention of concussion
Prevention of concussion consists in following the following rules:
- Wear a helmet when cycling, skateboarding, rollerblading, as well as playing hockey, rugby and other traumatic sports games;
- Protect your head when practicing martial arts;
- do not forget about the seat belt in the car;
- during icy conditions, use special pads on shoes that reduce slipping;
- follow the rules of personal safety, avoid traumatic situations.

Sources:
- Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 24.
- Mild traumatic brain injury: clinical guidelines / Potapov A.A., Likhterman L.B., Kravchuk A.D. and others – M .: Association of neurosurgeons of Russia, 2016 .– 23 p.
- Golovacheva V.A., Evzikov G.Yu. Management of a concussion patient. iDoctor 2014; 10 (29): 60-63.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-medication.In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. For a diagnosis and correct prescription of treatment, you should contact your doctor.
Information verified by an expert
Lishova Ekaterina Alexandrovna
Higher medical education, work experience – 19 years
Concussion
At first glance, the human brain may have little to threaten: after all, it is reliably protected by the bones of the skull. Well-established processes for maintaining the brain in the environment it needs, protect it from lack of nutrients and serve as an excellent shock absorber in case of falls and shocks. However, head injuries are very dangerous for the brain and often result in serious health problems.
Well-established processes for maintaining the brain in the environment it needs, protect it from lack of nutrients and serve as an excellent shock absorber in case of falls and shocks. However, head injuries are very dangerous for the brain and often result in serious health problems.
Any injuries can be divided into open and closed forms. Open injuries result in damage to the soft tissues of the head and bones of the skull. It is easy to guess that such injuries are especially dangerous for human health.Closed injuries are subdivided into several types: concussion, contusion, or compression of the brain. The most common type of injury is concussion. It is noteworthy that children under the age of one year practically do not receive a concussion. The reason for this is the ungrown fontanelle, which protects the baby from such complications during falls.
The causes of concussion are blows and bruises of a different nature, or sudden movements. Most often, people are concussed as a result of car accidents and accidents that occur in fights, or injured while playing sports or household chores.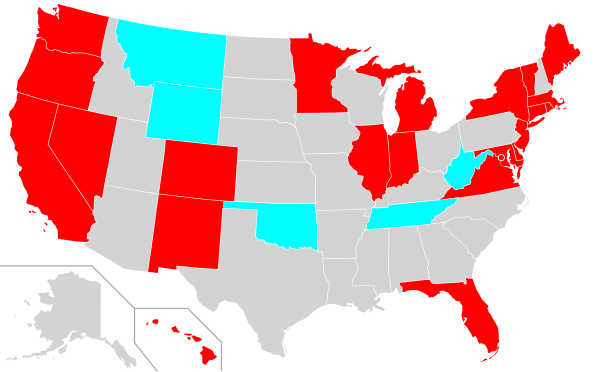
It is still difficult for modern medicine to accurately describe the processes occurring during a concussion. A computer scan will not show any signs of deviation, although in fact violations are occurring. As the doctors explain, most likely, with a concussion, the work of nerve cells is disrupted. In this regard, cellular nutrition is disrupted, and the connection between individual brain centers disappears. Severe concussion can compromise the integrity of blood vessels, and there is a high risk of serious damage to certain areas of the brain.Internal bleeding, which can disrupt the viability of brain cells, is a serious danger. In addition, there is an equally frightening complication – cerebral edema. The most severe injuries are accompanied by violations of the integrity of the brainstem, which strikes the regulation of respiration and blood pressure.
After such an injury, a person usually loses consciousness. The duration of the clouding of consciousness lasts for a short time: usually a few minutes. However, this symptom only occurs with serious injuries.We can say that the stronger the concussion, the longer the person will be unconscious. In the most severe cases, the patient may fall into a coma.
Another characteristic of the severity of damage is memory loss: the more serious the violation, the longer the period of time lived has sunk into oblivion. After the victim has regained consciousness, new symptoms may appear: nausea and vomiting, pallor, dizziness, tinnitus, rapid breathing. Upon examination, the doctor will probably notice one more feature: the pupils of the eyes after a concussion are always narrowed or dilated.One way or another, head trauma leads to disruption of neurochemical processes. If the pupils of the eyes do not respond well to light, the negative consequences of the injury are negligible. If the pupils do not react at all, or one pupil is narrowed and the other is dilated, there is a serious injury, up to the disruption of one of the cerebral hemispheres.
At the slightest suspicion of a brain injury, it is necessary to provide the victim with first aid and call a team of doctors.Provide the patient with peace, lay him on a flat surface, slightly raising his head. Cooling compresses may be applied prior to the arrival of the ambulance. In severe cases, closely monitor the patient, in case of cardiac arrest, start artificial respiration and indirect massage. Do not ignore the manifestation of symptoms. The situation can worsen in a matter of minutes, and the patient himself cannot always adequately assess his state of health.
Concussion is a traumatologist’s specialization.After being interviewed and examined, the doctor will likely order an X-ray or CT scan to rule out more serious damage to the skull and brain. As a treatment, adherence to strict bed rest is prescribed. During this time, it is not recommended to burden the brain with reading books or watching television programs. When applying the prescribed treatment and observing all the rules, the patient recovers in a week, less often in two.


