How do personalized hydration strategies impact athletic performance and safety. What are the key physiological, behavioral, and logistical factors that influence an athlete’s fluid needs. How can clinicians assess hydration status in athletes and provide practical hydration solutions.
The Importance of Proper Hydration for Athletes
Maintaining optimal hydration is crucial for athletes to perform at their best and stay safe during sports activities. Euhydration, the state of preserving body water within its ideal homeostatic range, is essential for sustaining life and athletic performance. Water makes up 50-70% of total body mass and is distributed between intracellular (65%) and extracellular (35%) spaces.
Proper hydration plays a vital role in numerous physiological functions that impact athletic performance, including:
- Regulating body temperature
- Transporting nutrients and oxygen to cells
- Removing waste products
- Lubricating joints
- Maintaining blood volume and cardiovascular function
Dehydration can significantly impair an athlete’s performance and increase the risk of heat-related illnesses. Even mild dehydration of just 2% body mass loss can negatively affect cognitive function, coordination, and endurance capacity.

Factors Influencing Fluid Needs in Athletes
An athlete’s fluid requirements during sports activities are influenced by various factors:
Environmental Conditions
Temperature, humidity, altitude, and air flow all impact sweat rates and fluid loss. Hot and humid environments increase fluid needs, while cold environments may reduce thirst sensation despite ongoing fluid losses.
Sport-Specific Demands
The intensity, duration, and nature of the sport affect hydration needs. Endurance events typically require more fluid intake than short-duration, high-intensity activities.
Individual Characteristics
Factors such as body size, sweat rate, heat acclimatization, and fitness level influence an athlete’s fluid requirements. Larger athletes and those with higher sweat rates generally need more fluids to maintain hydration.
Logistical Constraints
Access to fluids during training or competition can vary greatly between sports. Some activities allow frequent hydration opportunities, while others may restrict fluid intake to specific times.

Assessing Hydration Status in Athletes
Accurately assessing an athlete’s hydration status is crucial for developing effective hydration strategies. Several methods can be used to evaluate hydration levels:
Urine Color and Volume
Monitoring urine color and volume provides a simple, non-invasive indicator of hydration status. Pale yellow urine generally indicates proper hydration, while dark, concentrated urine suggests dehydration.
Body Weight Changes
Tracking changes in body weight before and after exercise can help estimate fluid losses. A loss of more than 2% of body weight indicates significant dehydration.
Thirst Sensation
While thirst can be a useful indicator of hydration needs, it’s important to note that thirst sensation may lag behind actual fluid requirements, especially during intense exercise or in hot conditions.
Bioelectrical Impedance
This method uses electrical currents to estimate body water content and can provide more precise measurements of hydration status.

Developing Personalized Hydration Strategies
Creating effective hydration plans for athletes requires a personalized approach that considers individual needs and sport-specific factors:
Pre-Exercise Hydration
Ensuring proper hydration before exercise is crucial. Athletes should aim to begin activities in a euhydrated state by consuming adequate fluids in the hours leading up to exercise.
During-Exercise Fluid Intake
Fluid intake during exercise should aim to replace sweat losses and prevent excessive dehydration. The amount and frequency of fluid consumption will vary based on individual sweat rates, exercise intensity, and environmental conditions.
Post-Exercise Rehydration
Replenishing fluid losses after exercise is essential for recovery. Athletes should aim to consume 150% of their fluid losses within 2-4 hours post-exercise to account for ongoing urine losses.
Practical Hydration Solutions for Different Sports
Implementing effective hydration strategies often requires creative solutions tailored to the specific demands and constraints of each sport:

Endurance Sports
For activities like marathon running or long-distance cycling, consider:
- Utilizing hydration belts or backpacks for easy access to fluids
- Planning refueling stations along the route
- Incorporating electrolyte-rich beverages to replace losses from prolonged sweating
Team Sports
In sports like soccer or basketball, strategies may include:
- Maximizing hydration during timeouts and halftime breaks
- Using personalized water bottles for quick identification
- Educating athletes on the importance of proactive hydration
Indoor Sports
For activities in climate-controlled environments, consider:
- Placing easily accessible water stations around the training area
- Encouraging regular hydration breaks during practice sessions
- Monitoring indoor temperature and humidity levels to adjust fluid needs
Overcoming Hydration Challenges in Extreme Environments
Athletes competing in extreme environments face unique hydration challenges that require specialized strategies:
Hot and Humid Conditions
In hot and humid environments, sweat rates increase dramatically, elevating the risk of dehydration and heat-related illnesses. To combat these challenges:
- Implement pre-cooling techniques to reduce core body temperature before exercise
- Use cold fluids and ice slurries to enhance cooling during activity
- Increase fluid intake to match elevated sweat rates
- Monitor urine color and body weight changes more frequently
Cold Environments
While fluid losses may be less apparent in cold conditions, dehydration can still occur due to increased respiratory water loss and reduced thirst sensation. Strategies for cold environments include:
- Encouraging regular fluid intake despite reduced thirst cues
- Using insulated hydration systems to prevent fluids from freezing
- Consuming warm fluids to aid in maintaining core body temperature
High Altitude
At high altitudes, increased respiratory water loss and diuresis can lead to accelerated dehydration. To address these issues:
- Increase fluid intake to compensate for elevated losses
- Monitor urine output and color more closely
- Consider using electrolyte-rich beverages to maintain proper fluid balance
The Role of Electrolytes in Athletic Hydration
Electrolytes play a crucial role in maintaining proper hydration and supporting athletic performance. These electrically charged minerals, including sodium, potassium, calcium, and magnesium, are essential for various physiological functions:

Fluid Balance
Electrolytes, particularly sodium, help regulate fluid balance between intracellular and extracellular spaces. This is crucial for maintaining blood volume and supporting cardiovascular function during exercise.
Muscle and Nerve Function
Electrolytes are vital for proper muscle contraction and nerve signaling. Imbalances can lead to muscle cramps, fatigue, and impaired performance.
Hydration Status
The presence of electrolytes in fluids can enhance fluid retention and absorption, improving overall hydration status.
For many athletes, especially those engaging in prolonged or intense exercise in hot conditions, incorporating electrolyte-rich beverages or supplements into their hydration strategy can be beneficial. However, the specific electrolyte needs can vary based on individual factors and the nature of the activity.
Hydration Strategies for Different Types of Athletes
While the fundamental principles of hydration remain consistent, the specific strategies may vary depending on the type of athlete and their sport:

Endurance Athletes
Marathoners, triathletes, and long-distance cyclists face unique hydration challenges due to the prolonged nature of their events. Key considerations include:
- Developing a comprehensive hydration plan that accounts for the entire duration of the event
- Balancing fluid intake with electrolyte replacement to prevent hyponatremia
- Practicing hydration strategies during training to optimize individual approaches
Team Sport Athletes
Athletes in sports like soccer, basketball, or rugby need to maintain hydration despite intermittent high-intensity efforts and limited access to fluids during play. Strategies may include:
- Maximizing hydration opportunities during breaks in play
- Using rapid hydration techniques to quickly replenish fluids during short rest periods
- Individualizing hydration plans based on positional demands and personal sweat rates
Strength and Power Athletes
Weightlifters, sprinters, and other power athletes may have different hydration needs due to the short-duration, high-intensity nature of their events. Considerations include:

- Focusing on maintaining hydration status between training sessions and competitions
- Balancing fluid intake to support performance without causing discomfort or excess body weight
- Addressing hydration needs specific to weight class competitions
The Impact of Hydration on Cognitive Function and Decision-Making in Sports
Proper hydration is not only crucial for physical performance but also plays a significant role in cognitive function and decision-making abilities, which are essential in many sports. Research has shown that even mild dehydration can negatively impact various aspects of cognitive performance:
Attention and Focus
Dehydration can lead to decreased attention span and difficulty maintaining focus, which can be particularly detrimental in sports requiring high levels of concentration and quick reactions.
Decision-Making Speed
Studies have demonstrated that dehydration can slow down decision-making processes, potentially impacting an athlete’s ability to make split-second choices during competition.

Mood and Perception
Inadequate hydration has been linked to increased perception of task difficulty and negative mood states, which can affect an athlete’s motivation and performance.
To support optimal cognitive function during sports activities, athletes should:
- Prioritize hydration before, during, and after cognitive-demanding tasks or competitions
- Monitor hydration status regularly, especially in situations where cognitive performance is crucial
- Educate themselves on the signs of cognitive impairment related to dehydration
Innovative Hydration Technologies and Their Application in Sports
Advancements in technology have led to the development of innovative tools and methods to support athlete hydration. These technologies can provide more accurate assessments of hydration status and help optimize fluid intake strategies:
Wearable Hydration Monitors
These devices use various methods, such as bioelectrical impedance or sweat analysis, to provide real-time feedback on hydration status. Athletes and coaches can use this information to make immediate adjustments to fluid intake during training or competition.

Smart Water Bottles
Equipped with sensors and connected to smartphone apps, these bottles can track fluid intake, set hydration goals, and provide reminders to drink. This technology can be particularly useful for athletes who struggle to maintain consistent hydration habits.
Sweat Analysis Patches
These wearable patches can analyze the electrolyte content of an athlete’s sweat, providing valuable information for creating personalized hydration and electrolyte replacement strategies.
Hydration Testing Devices
Portable devices that can quickly analyze urine or saliva samples to assess hydration status are becoming more accessible, allowing for more frequent and convenient monitoring.
While these technologies offer exciting possibilities for optimizing hydration strategies, it’s important to remember that they should be used in conjunction with, not as a replacement for, traditional hydration assessment methods and individualized approaches developed with healthcare professionals.

Educating Athletes on Hydration Best Practices
Empowering athletes with knowledge about proper hydration is crucial for implementing effective strategies and promoting long-term healthy habits. Key areas of education should include:
Understanding Hydration Physiology
Provide athletes with a basic understanding of how the body regulates fluid balance and the impact of dehydration on performance and health.
Recognizing Dehydration Signs
Teach athletes to identify early signs of dehydration, such as thirst, dark urine, and decreased performance, so they can take proactive measures.
Personalized Hydration Strategies
Help athletes develop individualized hydration plans based on their specific needs, sweat rates, and sport requirements.
Proper Use of Sports Drinks
Educate athletes on when and how to use sports drinks effectively, including understanding the differences between various types of beverages and their appropriate applications.
Hydration in Different Environments
Provide guidance on adjusting hydration strategies for various environmental conditions, including hot, cold, and high-altitude settings.

Effective education programs can utilize a variety of methods, including:
- Interactive workshops and seminars
- Hands-on demonstrations of hydration assessment techniques
- Integration of hydration education into regular training sessions
- Use of technology, such as apps or online resources, to reinforce learning
By fostering a deeper understanding of hydration principles and practices, athletes can become more proactive and effective in managing their fluid needs, ultimately leading to improved performance and reduced risk of hydration-related issues.
Practical Hydration Solutions for Sports
Nutrients. 2019 Jul; 11(7): 1550.
,1,*,2,1,3,4,5,6,7,8,9,1,10,4,11,12,13,14,1,15 and 16
Luke N. Belval
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Yuri Hosokawa
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
Douglas J. Casa
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
William M. Adams
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
Lawrence E. Armstrong
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Lindsay B.
 Baker
Baker
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
Louise Burke
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
Samuel Cheuvront
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
George Chiampas
8U.S. Soccer, Chicago, IL 60616, USA
José González-Alonso
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
Robert A. Huggins
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Stavros A. Kavouras
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
Elaine C. Lee
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Brendon P. McDermott
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
Kevin Miller
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
Zachary Schlader
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
Stacy Sims
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
Rebecca L.
 Stearns
Stearns
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Chris Troyanos
15International Institute of Race Medicine, Plymouth, MA 02360, USA
Jonathan Wingo
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
8U. S. Soccer, Chicago, IL 60616, USA
S. Soccer, Chicago, IL 60616, USA
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
15International Institute of Race Medicine, Plymouth, MA 02360, USA
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
Received 2019 May 15; Accepted 2019 Jul 3.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
Abstract
Personalized hydration strategies play a key role in optimizing the performance and safety of athletes during sporting activities. Clinicians should be aware of the many physiological, behavioral, logistical and psychological issues that determine both the athlete’s fluid needs during sport and his/her opportunity to address them; these are often specific to the environment, the event and the individual athlete. In this paper we address the major considerations for assessing hydration status in athletes and practical solutions to overcome obstacles of a given sport. Based on these solutions, practitioners can better advise athletes to develop practices that optimize hydration for their sports.
Keywords: fluid replacement, athletics, exercise
1.
 Introduction
Introduction
Maintaining euhydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water contributes 50–70% of total body mass and is compartmentalized within both intracellular (65%) and extracellular (35%) spaces [1]. Euhydration is typically maintained over the course of day-to-day life via behavioral and biological controls [2]. However, exercise can cause an acute disruption to fluid balance, challenging the athlete’s goal of optimal performance and safety during exercise, especially in hot environmental conditions. The process of incurring a fluid deficit is known as dehydration, while the outcome is defined as hypohydration. The loss of body water during exercise exacerbates physiological and perceptual strain [3,4,5,6,7,8,9,10] and it is well established that these changes can impair endurance performance, particularly in hot environments and may increase the risk of exertional heat illness [11,12,13,14,15,16,17].
While the sensation of thirst, a centrally mediated response to body water deficits, is useful in dictating the need for fluid intake during daily life, thirst is relatively insensitive in acutely tracking hydration status during exercise [18,19]. Maintaining an optimal state of hydration during exercise becomes more complicated depending on the sport, type of activity and availability of fluid. Optimal hydration is dependent on many factors but can generally be defined during exercise as avoiding losses greater than 2–3% of body mass while also avoiding overhydration [15]. Furthermore, during exercise, it is not uncommon for individuals to involuntarily dehydrate, in which they consume less fluid than their fluid needs. Excessive fluid intake can also be problematic, with hyponatremia developing in severe cases of overhydration [15]. Inappropriate management of fluid intake resulting in hypohydration, or hyperhydration, can be detrimental for performance and in some circumstances, increases health risk.
Current consensus recommends that good hydration practices include: (1) beginning exercise in a state of euhydration, (2) preventing excessive hypohydration during exercise, and (3) replacing remaining losses following exercise prior to the next exercise bout [15,20,21]. These practices attenuate the adverse effects of acute dehydration on physical activity and health [15]. However, it is acknowledged that fluid needs are individualistic and rely on factors such as personal sweat rate, exercise mode, exercise intensity, environmental conditions and exercise duration () [14,15,22,23,24,25]. Furthermore, characteristics and rules unique to each sport environment in which it is played, event uniform and equipment, and the availability of fluid during both training and competition may greatly influence the ability to optimize hydration during activity. The Korey Stringer Institute and Gatorade convened a meeting to address these issues as they relate to athletes. The purpose of these proceedings is to discuss practical strategies to assess and tailor hydration for sports. This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
Factors that contribute to the risk of hypohydration or hyperhydration during exercise.
2. Hydration Assessment
Hydration assessment can be utilized to indicate one’s current hydration state, but if taken serially, it can also be used to track changes in hydration and indicate fluid needs (i.e., during a bout of physical activity). While various methods of hydration assessment exist, there is no single method that can serve as a criterion measure to assess hydration status in all settings (i.e., day-to-day life and exercise, etc.). Plasma osmolality, changes in plasma volume, and the volume, osmolality and specific gravity of urine are the most commonly published metrics to assess changes in hydration status in clinical settings [26]. The use of these measures in field applications is often impractical, due to the methods or equipment needed to acquire the measure (e. g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
In field applications, the careful assessment of changes in body mass over a bout of physical activity provides a reasonably accurate assessment of body water deficits incurred during the session, since sweat loss and fluid intake during the session underpin the major changes in body mass and body water content. This is true for most sporting activities conducted over a duration of <2–3 h; however, during very prolonged and strenuous exercise (e.g., ultra-endurance races), other factors that cause mass changes, metabolic water production and the liberation of stored water become numerically important and undermine the utility of this assessment [15,27,28]. A comparison of body mass pre- and post-exercise will help guide the athlete in understanding whether their hydration strategy during activity was effective in achieving acceptable fluid balance as well as knowing the volume of fluids that are needed following exercise to return to baseline hydration levels prior to the next exercise session. The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
A useful paradigm for tracking daily changes in hydration status in sporting situations is to consider a combination of assessments to track daily changes. The monitoring of daily changes in body mass, coupled with urine color and thirst sensation status provides adequate sensitivity for most athletic situations [30]. Cheuvront and Kenefick established useful criteria for these variables as body mass changes greater than 1.1%, a conscious desire for water (thirst), and dark-colored urine (>5 a.u. on an 8-a.u. scale [31]) indicating varying degrees of fluid inadequacy [32]. Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Practical Solutions:
(1)
Carefully monitor acute changes in body mass over an exercise bout to determine sweat rate, adequacy of fluid replacement and fluid needs for recovery for that session. Consider how well this can be used to evaluate general hydration strategies in similar situations.
(2)
Use changes in body mass, urine color and thirst upon awakening to track daily changes in hydration status.
3. Exercise Structure
Body fluid loss during sport or exercise largely results from sweating. Net fluid balance is modulated to a certain extent by drinking. Rate of sweating is primarily a function of metabolic heat production [33], but can be modified by environment, clothing, acclimatization and hydration status [7,34]. As the primary mechanism of heat dissipation in many environments, the evaporation of sweat is vital for regulating body temperature, even during exercise in temperate weather. However, this heat dissipation is accompanied by typical fluid losses of ~0.5–1.9 L/h [35].
As the primary mechanism of heat dissipation in many environments, the evaporation of sweat is vital for regulating body temperature, even during exercise in temperate weather. However, this heat dissipation is accompanied by typical fluid losses of ~0.5–1.9 L/h [35].
Exercise intensity is the main factor that determines metabolic heat production, meaning that the rate of fluid losses from sweat for a given exercise session can be partially explained by the intensity of the exercise [36]. Total fluid losses are a result of the sweat rate of a given exercise intensity and the total duration of that activity [27]. In most circumstances there is an inverse relationship between the exercise intensity of a session and the duration of that session. However, given the wide variability in individual sweat rates, the unique interplay between intensity, duration and sweat rate must be considered in unison. For example, a runner with a 2 L/h sweat rate who completes a marathon in 2 h will accumulate the same fluid losses as a runner with a 1 L/h sweat rate that completes the race in 4 h. In and , we define exercise intensity of a range of sporting activities into three distinct categories (High, Moderate, Low), based on typical practice and competition structures on the principles described above but comprehensive plans should consider individual athletes.
In and , we define exercise intensity of a range of sporting activities into three distinct categories (High, Moderate, Low), based on typical practice and competition structures on the principles described above but comprehensive plans should consider individual athletes.
Table 1
Team Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Basketball | High | High | Low | Low | Mod | Mod | Low | Low |
| Ice Hockey | High | High | Low | Low | Mod | High | Mod | Mod |
| Football | High | High | Mod | Mod | Mod | High | Mod | Mod |
| Baseball | High | High | Mod | Mod | Low | Low | Low | Low |
| Softball | High | High | Mod | Mod | Low | Low | Low | Low |
| Volleyball | High | High | Low | Low | Low | Low | Low | Low |
| Soccer | Mod | Low | Mod | Mod | Mod | High | Mod | High |
| Lacrosse | High | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Rugby | High | Low | Mod | Mod | Mod | High | Mod | High |
Table 2
Individual Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Tennis | High | Mod | Mod | Mod | High | High | Mod | Mod |
| Wrestling | High | High | Mod | Mod | High | High | High | Low |
| Gymnastics | High | High | Low | Low | Mod | Low | Low | Low |
| Running (<1 h) | Low | High | Mod | Mod | High | High | Low | Low |
| Running (1–2 h) | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Running (>2 h) | Low | High | Mod | Mod | Low | Mod | Mod | Mod |
| Cycling (<1 h) | High | High | Mod | Mod | High | High | Low | Low |
| Cycling (>2 h) | Mod | Mod | Mod | Mod | Mod | Mod | Low | High |
| Swimming | High | High | Low | Low | High | High | Low | Low |
| Triathlon (<2 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (2–5 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (5–9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Triathlon (>9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
For sports like cycling and running, the influence of exercise intensity and duration on fluid needs is very easy to determine given the consistent nature of exercise. demonstrates the relationship between duration and target fluid replacement for steady-state exercise. However, as shown in , some of the most common sports involve supramaximal exercise in short bursts with longer breaks. In this case, individuals should regard an overall average of exercise intensity rather than the maximal effort during the exercise bout when determining optimal fluid balance.
demonstrates the relationship between duration and target fluid replacement for steady-state exercise. However, as shown in , some of the most common sports involve supramaximal exercise in short bursts with longer breaks. In this case, individuals should regard an overall average of exercise intensity rather than the maximal effort during the exercise bout when determining optimal fluid balance.
Target fluid replacement estimates to prevent >2 ± 1 % body mass (BM) loss as water (i.e., dehydration). The 70 kg athlete in the example would need to drink a volume of fluid equal to 2.6 ± 0.7 L to prevent >2 ± 1% dehydration when losing 4 L of body water, such as during a marathon (42.1 km). During shorter distances such as 5 or 10 km when fluid losses are unlikely to reach or exceed 2% dehydration, the same athlete would not need to ingest fluids during competition as fluid losses accumulate to <2% dehydration.
It should also be noted that exercise intensity influences gastric emptying rate [37]. Individuals striving to closely match sweat losses with fluid consumption can be challenged by maximal gastric emptying rates. However, when vigorous exercise is conducted (>70% VO2max), gastric emptying decreases predictably, most likely based on decreased splanchnic perfusion [37].
Individuals striving to closely match sweat losses with fluid consumption can be challenged by maximal gastric emptying rates. However, when vigorous exercise is conducted (>70% VO2max), gastric emptying decreases predictably, most likely based on decreased splanchnic perfusion [37].
Practical Solutions:
(1)
Increased fluid intake is necessary with prolonged or intense exercise due to increased sweat production.
(2)
During vigorous exercise (>70% VO2max) understand that gastric emptying may limit fluid absorption. Athletes can train their gut to improve gastrointestinal comfort or adopt strategies to increase fluid intake before and after exercise.
4. Environment
At a fixed exercise intensity, the ambient environment further modulates sweat rate. The magnitude of evaporative, radiant, convective and conductive heat exchange between the body and the environment is a function of the gradients between the environment and the skin which provides the main physiological interface for heat exchange. A number of factors contribute to sweat rate including ambient and radiant temperature, humidity, clothing, and air velocity [34], all of which differ depending on the sport or activity ( and ). Therefore, individuals exercising in hot-humid environments with direct sunlight and minimal airflow will produce near maximal sweat rates and be at the greatest risk of hypohydration. Wet-bulb globe thermometry (WBGT) accounts for these environmental factors and can help inform fluid replacement decisions [38].
A number of factors contribute to sweat rate including ambient and radiant temperature, humidity, clothing, and air velocity [34], all of which differ depending on the sport or activity ( and ). Therefore, individuals exercising in hot-humid environments with direct sunlight and minimal airflow will produce near maximal sweat rates and be at the greatest risk of hypohydration. Wet-bulb globe thermometry (WBGT) accounts for these environmental factors and can help inform fluid replacement decisions [38].
All clothing provides insulation and presents a barrier to heat loss, resulting in increased sweat rates to provide similar cooling to an unclothed situation [34]. Thus, sports/activities with specific clothing requirements, such as American football [39,40], are at greater risk of body fluid loss compared to similar activities in which clothing is minimal. Synthetic wicking materials can increase sweat fluid losses compared to cotton garments [41], potentially decreasing the thermal load but increasing the risk of dehydration. When the effects of hot, humid environmental conditions are combined with clothing and equipment, individuals can achieve near maximal sweat rates which can create a significant fluid deficit rapidly [40].
When the effects of hot, humid environmental conditions are combined with clothing and equipment, individuals can achieve near maximal sweat rates which can create a significant fluid deficit rapidly [40].
Other Environmental Considerations:
Exercising in the cold, or at high altitudes merits special considerations when determining the fluid needs of athletes. Athletes must also be vigilant and mindful of their fluid needs during exercise in the cold. Exercise in the cold can still produce copious sweating, especially when heavy clothing is worn, while also diminishing thirst sensitivity and reducing ad libitum fluid consumption, thus potentially leading to impaired fluid replacement and hypohydration [42]. If possible, athletes should know their individual fluid replacement needs, based upon sweat rate measurement, during exercise in hot and cold environments to ensure they can develop a plan for competing while optimally hydrated.
Athletes unaccustomed to exercising in higher altitudes may require additional fluids. Very high altitude (4900–7600 m) exposure tends to increase water and electrolyte losses, decrease plasma volume and total body water content [43]. In both cold air and high altitudes, respiratory water losses may increase and require additional fluid consumption due to low air water vapor pressures [44]. Therefore, athletes should acclimate to altitude over several days and maintain euhydration prior to competition to ensure optimal athletic performance.
Very high altitude (4900–7600 m) exposure tends to increase water and electrolyte losses, decrease plasma volume and total body water content [43]. In both cold air and high altitudes, respiratory water losses may increase and require additional fluid consumption due to low air water vapor pressures [44]. Therefore, athletes should acclimate to altitude over several days and maintain euhydration prior to competition to ensure optimal athletic performance.
and summarizes typical environmental conditions found among a range of sports into three distinct categories, and how these conditions contribute to the considerations around an individualized fluid plan. Of course, there are large regional differences in environmental conditions experienced for sports at the same time of year [45]. Local measurements utilizing WBGT allow for the greatest characterization of the environmental demands placed on athletes during exercise in the heat [46].
Practical Solutions:
(1)
Measure local environmental conditions to determine the risk of high sweat rates resulting in large fluid losses.

(2)
Increase fluid-replacement during exercise in hot and humid environments to account for increased sweat losses.
(3)
Account for clothing or equipment requirements when evaluating fluid needs.
(4)
Modify fluid intake when exercising in cold or altitude according to an estimation of fluid losses noting that thirst may be less reliable as a guide to dehydration under these conditions.
5. Fluid Availability
Fluid availability refers to the factors that dictate an athlete’s ability to replace fluid losses during activity. In many instances, the characteristics of the sport have a strong influence on the ability to drink during competition and in many scenarios prevent an athlete from “drinking to thirst” [21]. Meanwhile, training activities are often easily modified to allow for some degree of fluid replacement. In many instances, water-breaks during training can be determined on the basis of work-to-rest ratios set by environmental conditions with free access to fluid throughout the break [47]. Characteristics such as flavor and temperature affect the palatability of fluids and may increase voluntary intake when they are matched to the cultural preferences of the athletes and the prevailing conditions (e.g., cool drinks in a warm environment) [48,49].
Characteristics such as flavor and temperature affect the palatability of fluids and may increase voluntary intake when they are matched to the cultural preferences of the athletes and the prevailing conditions (e.g., cool drinks in a warm environment) [48,49].
In endurance sports which provide competitors with feed zones/water stations (e.g., running events), the number of water stations on a course and the frequency with which a competitor reaches them can influence drinking behavior. The International Association of Athletics Federations recommends that stations are placed approximately every 5 km, however, many races include more frequent stations which may influence athletes’ drinking strategies and behaviors [50]. Slower athletes with lower sweat rates who compete in such events, particularly over prolonged distances or duration, are often able to drink in volumes that exceed their true fluid losses and are at particular risk of developing hyponatremia [51]. Athletes taking part in these events should be educated on the importance of fluid balance and the prevention of hyperhydration. It should also be noted that in many events lasting up to 45 min, the risk of dehydration is low due to the limited duration across which sweat losses can accumulate. For faster and/or more competitive athletes, extra elements related to drinking while performing continuous exercise must be taken into consideration. This includes considerations around gastrointestinal comfort when fluid consumed during higher-intensity and “gut joggling” activities (e.g., high-speed running vs. the more “gliding” movements of cross-country skiing or cycling). Furthermore, the time lost in slowing down or moving out of an aerodynamic position to obtain or consume a drink must be factored into the overall race performance. This creates different factors in the cost:benefit analysis of an individual’s fluid intake plan.
It should also be noted that in many events lasting up to 45 min, the risk of dehydration is low due to the limited duration across which sweat losses can accumulate. For faster and/or more competitive athletes, extra elements related to drinking while performing continuous exercise must be taken into consideration. This includes considerations around gastrointestinal comfort when fluid consumed during higher-intensity and “gut joggling” activities (e.g., high-speed running vs. the more “gliding” movements of cross-country skiing or cycling). Furthermore, the time lost in slowing down or moving out of an aerodynamic position to obtain or consume a drink must be factored into the overall race performance. This creates different factors in the cost:benefit analysis of an individual’s fluid intake plan.
The official rules and competition characteristics of “stop-start” sports such as team and racket sports create other influences, and often unique scenarios, around fluid availability. In some examples (e.g., soccer, rugby), governing rules limit the availability of fluids for athletes during competition. Soccer, for example, includes two 45-min halves (with a continuous running clock) in which fluid availability is extremely limited to players. At the other end of the spectrum are sports such as baseball, basketball and tennis with frequent rest breaks within playing time (e.g., time outs, change of ends or player rotations) during which fluids can be consumed. An athlete’s drinking strategy for a competition represents a unique instance for their particular sport based on their ability to rehydrate within the rules [52]. We support recent governing body rule changes and referee decisions to add breaks to competitions (Major League Soccer, FIFA soccer matches, US Open Tennis) to facilitate safe participation by the athletes. These changes likely augment athletic performance and safety simultaneously. Individuals should understand their sport and its fluid needs/fluid availability characteristics to prepare and practice optimal fluid plans for competition.
In some examples (e.g., soccer, rugby), governing rules limit the availability of fluids for athletes during competition. Soccer, for example, includes two 45-min halves (with a continuous running clock) in which fluid availability is extremely limited to players. At the other end of the spectrum are sports such as baseball, basketball and tennis with frequent rest breaks within playing time (e.g., time outs, change of ends or player rotations) during which fluids can be consumed. An athlete’s drinking strategy for a competition represents a unique instance for their particular sport based on their ability to rehydrate within the rules [52]. We support recent governing body rule changes and referee decisions to add breaks to competitions (Major League Soccer, FIFA soccer matches, US Open Tennis) to facilitate safe participation by the athletes. These changes likely augment athletic performance and safety simultaneously. Individuals should understand their sport and its fluid needs/fluid availability characteristics to prepare and practice optimal fluid plans for competition. Where rule changes, or alterations are allowed, individuals and teams should attempt to ask for these alterations (e.g., extended rest periods, additional breaks) in advance to formulate an appropriate drinking strategy. In all sports, athletes should aim to practice and fine-tune their personal drinking strategy for race/competition conditions. This will help individuals to confirm its feasibility, understand their personal responses and develop any necessary behavioral practices within the expected rules of competition.
Where rule changes, or alterations are allowed, individuals and teams should attempt to ask for these alterations (e.g., extended rest periods, additional breaks) in advance to formulate an appropriate drinking strategy. In all sports, athletes should aim to practice and fine-tune their personal drinking strategy for race/competition conditions. This will help individuals to confirm its feasibility, understand their personal responses and develop any necessary behavioral practices within the expected rules of competition.
In and , we define fluid availability into three distinct categories, based on particular sport variations. Sports were categorized as having high fluid availability if there are multiple opportunities for fluid consumption, rather than only during breaks. Low fluid availability was used to describe those activities involving governing rules, time constraints, or an inability to carry personal fluids during competition. Accessibility to fluid consumption during competition represents a major variable to be used in preparation of an optimal fluid replacement strategy.
Practical Solutions:
(1)
During training, ensure that there is ample access to fluids that are palatable to athletes.
(2)
Investigate or understand the opportunities for fluid intake during that are specific to a sport or event, and any other practical issues that determine fluid intake.
(3)
Consider the risks of hyperhydration as well as hypohydration for any sporting event or individual athlete, and prepare appropriate practice and education strategies.
(4)
Develop personalized fluid intake plans that incorporate fluid availability characteristics of the sport or event. Where there is a likelihood of hypohydration, be proactive and creative in making use of existing opportunities for fluid intake within sport rules and characteristics and be prepared to request for changes when there is a likelihood of a serious mismatch between fluid losses and the opportunity to address these.
(5)
Practice intended competition drinking plans ahead of time to determine their suitability and allow time for readjustment.

6. Intrinsic Factors
A number of intrinsic factors modulate the individual variances that are observed in fluid losses. One of the greatest considerations for an individual’s sweat rate is his or her body size. Larger individuals typically have higher sweat losses, with football linemen exhibiting some of the highest recorded sweat rates [14]. Therefore, required absolute drink volumes will be higher for these athletes. An individual’s thirst drive also dictates how much they desire to drink during exercise, but this may not match their actual fluid needs. Indeed, multiple authors report that athletes voluntarily dehydrate during exercise due to discrepancies in fluid losses and drinking behavior [53,54]. Case studies of individuals who have developed hyponatremia due to excessive drinking during exercise also note that they reported thirst as an underlying contributor to their fluid intake [55].
Heat acclimatization contributes to variations in an individual’s sweating rate responses. Individuals who are heat acclimatized exhibit greater sweat rates which can pose a greater risk of hypohydration [56]. Although the increased sweat provides extra heat dissipation, it also requires extra fluid intake.
Individuals who are heat acclimatized exhibit greater sweat rates which can pose a greater risk of hypohydration [56]. Although the increased sweat provides extra heat dissipation, it also requires extra fluid intake.
Women may be at greater risk for exercise-induced hyponatremia. This risk has been attributed to their lower body weight and size, excess water ingestion, and longer racing times relative to men [57]. The greater incidence of hyponatremia in women is unlikely due to their greater levels of estradiol in plasma and tissue. Although female sex-hormones can also influence neural and hormonal control of thirst, fluid intake, sodium appetite and sodium regulation [58,59], there is no evidence that anything beyond stature and drinking behavior significantly impact their risk.
Practical Solutions:
7. Sport-Specific Factors
Weight Division, Acrobatic and Appearance-Based Sports
The culture and normal behaviors surrounding specific sports can greatly affect the hydration practices of its athletes. The three most prominent examples of the cultural effects of sports on hydration practices are weight division sports, acrobatic sports and appearance-based sports. In weight division sports (e.g., combat sports, horse racing, lightweight rowing, etc.), the practice of deliberately dehydrating to manipulate body mass to meet lighter competition weight classifications is common [60]. In many cases, athletes not only sacrifice their performance through these practices but also endanger their health and well-being. In a similar fashion, sports where body-image and appearance are emphasized (e.g., cheerleading, body building and gymnastics), dangerous practices, such as extreme fluid restriction may be used by athletes to cheat “unofficial” weight checks that are self-instigated or expected within their training environment. Finally, “acrobatic” feats such as gymnastics, jumping and climbing are aided by a high power to weight ratio, but should not rely on severe hypohydration to achieve this.
The three most prominent examples of the cultural effects of sports on hydration practices are weight division sports, acrobatic sports and appearance-based sports. In weight division sports (e.g., combat sports, horse racing, lightweight rowing, etc.), the practice of deliberately dehydrating to manipulate body mass to meet lighter competition weight classifications is common [60]. In many cases, athletes not only sacrifice their performance through these practices but also endanger their health and well-being. In a similar fashion, sports where body-image and appearance are emphasized (e.g., cheerleading, body building and gymnastics), dangerous practices, such as extreme fluid restriction may be used by athletes to cheat “unofficial” weight checks that are self-instigated or expected within their training environment. Finally, “acrobatic” feats such as gymnastics, jumping and climbing are aided by a high power to weight ratio, but should not rely on severe hypohydration to achieve this.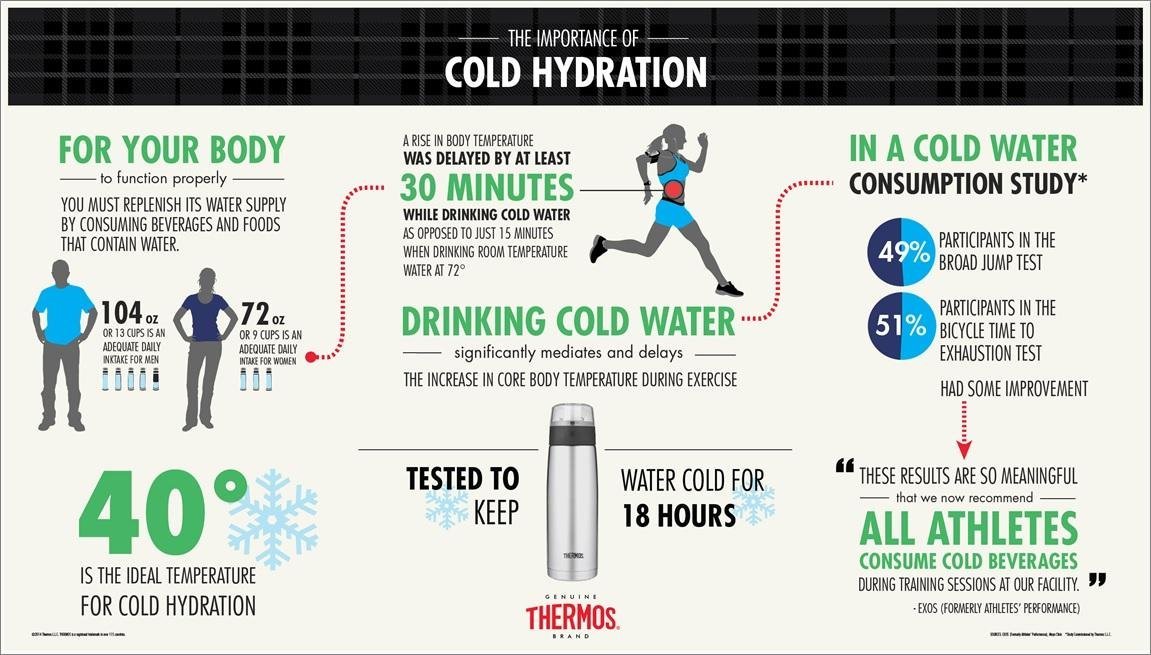 Excessive use of dehydration to manage body mass goals should be corrected to avoid long-term health complications [61].
Excessive use of dehydration to manage body mass goals should be corrected to avoid long-term health complications [61].
Practical Solutions:
8. Conclusions
Based on the factors in the above sections, along with published literature on typical fluid balance observations in various sports [62,63], we assigned risks of hypohydration to the sports in and . These determinations can be used as a general guideline for sports that pose large risks for fluid imbalances that may limit sport performance. The factors for individual situations or geographical locations may vary and should be considered based on the principles mentioned above to tailor the necessary fluid replacement accommodations. An example of using this paradigm to develop a hydration plan can be found in .
Table 3
Establishing a Hydration Plan.
| Guiding Question | Steps to Correct | Implementation Example |
|---|---|---|
| Are athletes in a state of optimal hydration? | ||
| Is the exercise prolonged or intense? | ||
| Is the exercise being performed in environmental conditions that lead to greater fluid losses? | ||
| Is fluid available throughout the entire duration of exercise? |
| |
| Are there individuals with intrinsic risk factors? |
| |
| Are there sport-specific factors that need to be considered? |
In this paper we present a paradigm that can be used by clinicians and practitioners to develop hydration strategies for sports based on fluid availability, environment and exercise intensity. These tools are provided to inform hydration education and practices in a dynamic and individualized manner so that athletes can adapt to different circumstances and optimize performance.
These tools are provided to inform hydration education and practices in a dynamic and individualized manner so that athletes can adapt to different circumstances and optimize performance.
Author Contributions
All authors attended the meeting and contributed to drafting and revision of the manuscript. All authors approved the final version of the paper.
Funding
The meeting preceding this manuscript was funded by PepsiCo (Gatorade).
Conflicts of Interest
Douglas Casa is the Chief Executive Officer of the Korey Stringer Institute, a 503.c not for profit which subsists on the donations from our corporate partners who include Gatorade, CamelBak, NFL, NATA, Mission, Eagle Pharmaceuticals and Kestrel. He has also been a recipient of grant funds from the following entities to study hydration related products: GE Healthcare, Halo Wearables, Nix Inc., CamelBak. William Adams has consulted with the following entities regarding hydration and exercise performance or the development of hydration assessment devices: BSX Athletics; Samsung Oak Holdings, Inc; Nobo, Inc; Clif Bar &Company; The Gatorade Company, Inc. Lawrence Armstrong is a hydration consultant to Danone Nutricia Research, France and the Drinking Water Research Foundation, Alexandria VA, USA. Lindsay Baker is employed by the Gatorade Sports Science Institute, a division of PepsiCo, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc. Louise Burke was a member of the Gatorade Sports Science Institute’s Expert Panel from 2014–2015 for which her workplace received an honorarium. Jose Gonzalez-Alonso was a member of the Gatorade Sports Science Institute’s Expert Panel in 2017 for which his workplace received an honorarium. Stavros Kavouras has served as scientific consultant for Quest Diagnostics, Standard Process and Danone Research and has active grants with Danone Research. The funders had no role in the in the writing of the manuscript.
Lawrence Armstrong is a hydration consultant to Danone Nutricia Research, France and the Drinking Water Research Foundation, Alexandria VA, USA. Lindsay Baker is employed by the Gatorade Sports Science Institute, a division of PepsiCo, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc. Louise Burke was a member of the Gatorade Sports Science Institute’s Expert Panel from 2014–2015 for which her workplace received an honorarium. Jose Gonzalez-Alonso was a member of the Gatorade Sports Science Institute’s Expert Panel in 2017 for which his workplace received an honorarium. Stavros Kavouras has served as scientific consultant for Quest Diagnostics, Standard Process and Danone Research and has active grants with Danone Research. The funders had no role in the in the writing of the manuscript.
References
1. Sawka M., Pandolf K.B. Effects of body water loss on physiological function and exercise performance. In: Gisolfi C., Lamb D.R., editors. Perspectives in Exercise Science and Sports Medicine. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 1–38. [Google Scholar]2. Sawka M.N., Wenger C.B., Pandolf K.B. Thermoregulatory Responses to Acute Exercise-Heat Stress and Heat Acclimation. In: Terjung R., editor. Comprehensive Physiology. John Wiley & Sons; Hoboken, NJ, USA: 2011. pp. 97–151. [Google Scholar]3. Montain S.J., Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [PubMed] [CrossRef] [Google Scholar]4. Montain S.J., Sawka M.N., Latzka W.A., Valeri C.R. Thermal and cardiovascular strain from hypohydration: Influence of exercise intensity. Int. J. Sports Med. 1998;19:87–91. doi: 10.1055/s-2007-971887. [PubMed] [CrossRef] [Google Scholar]5. Sawka M.N., Young A.J., Francesconi R.P., Muza S.R., Pandolf K.B. Thermoregulatory and blood responses during exercise at graded hypohydration levels.
In: Gisolfi C., Lamb D.R., editors. Perspectives in Exercise Science and Sports Medicine. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 1–38. [Google Scholar]2. Sawka M.N., Wenger C.B., Pandolf K.B. Thermoregulatory Responses to Acute Exercise-Heat Stress and Heat Acclimation. In: Terjung R., editor. Comprehensive Physiology. John Wiley & Sons; Hoboken, NJ, USA: 2011. pp. 97–151. [Google Scholar]3. Montain S.J., Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [PubMed] [CrossRef] [Google Scholar]4. Montain S.J., Sawka M.N., Latzka W.A., Valeri C.R. Thermal and cardiovascular strain from hypohydration: Influence of exercise intensity. Int. J. Sports Med. 1998;19:87–91. doi: 10.1055/s-2007-971887. [PubMed] [CrossRef] [Google Scholar]5. Sawka M.N., Young A.J., Francesconi R.P., Muza S.R., Pandolf K.B. Thermoregulatory and blood responses during exercise at graded hypohydration levels. J. Appl. Physiol. 1985;59:1394–1401. doi: 10.1152/jappl.1985.59.5.1394. [PubMed] [CrossRef] [Google Scholar]6. Adams W.M., Ferraro E.M., Huggins R.A., Casa D.J. Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 2014;28:2380–2389. doi: 10.1519/JSC.0000000000000501. [PubMed] [CrossRef] [Google Scholar]7. Kenefick R.W., Cheuvront S.N. Physiological adjustments to hypohydration: Impact on thermoregulation. Auton. Neurosci. 2016;196:47–51. doi: 10.1016/j.autneu.2016.02.003. [PubMed] [CrossRef] [Google Scholar]8. Trangmar S.J., Gonzalez-Alonso J. New Insights into the Impact of Dehydration on Blood Flow and Metabolism during Exercise. Exerc. Sport Sci. Rev. 2017;45:146–153. doi: 10.1249/JES.0000000000000109. [PubMed] [CrossRef] [Google Scholar]9. Gonzalez-Alonso J., Crandall C.G., Johnson J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008;586:45–53. doi: 10.1113/jphysiol.2007.142158. [PMC free article] [PubMed] [CrossRef] [Google Scholar]10.
J. Appl. Physiol. 1985;59:1394–1401. doi: 10.1152/jappl.1985.59.5.1394. [PubMed] [CrossRef] [Google Scholar]6. Adams W.M., Ferraro E.M., Huggins R.A., Casa D.J. Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 2014;28:2380–2389. doi: 10.1519/JSC.0000000000000501. [PubMed] [CrossRef] [Google Scholar]7. Kenefick R.W., Cheuvront S.N. Physiological adjustments to hypohydration: Impact on thermoregulation. Auton. Neurosci. 2016;196:47–51. doi: 10.1016/j.autneu.2016.02.003. [PubMed] [CrossRef] [Google Scholar]8. Trangmar S.J., Gonzalez-Alonso J. New Insights into the Impact of Dehydration on Blood Flow and Metabolism during Exercise. Exerc. Sport Sci. Rev. 2017;45:146–153. doi: 10.1249/JES.0000000000000109. [PubMed] [CrossRef] [Google Scholar]9. Gonzalez-Alonso J., Crandall C.G., Johnson J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008;586:45–53. doi: 10.1113/jphysiol.2007.142158. [PMC free article] [PubMed] [CrossRef] [Google Scholar]10. Trangmar S.J., Gonzalez-Alonso J. Heat, Hydration and the Human Brain, Heart and Skeletal Muscles. Sports Med. 2019;49:69–85. doi: 10.1007/s40279-018-1033-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]11. Cheuvront S.N., Carter R., 3rd, Sawka M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003;2:202–208. doi: 10.1249/00149619-200308000-00006. [PubMed] [CrossRef] [Google Scholar]12. Cheuvront S.N., Kenefick R.W., Montain S.J., Sawka M.N. Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 2010;109:1989–1995. doi: 10.1152/japplphysiol.00367.2010. [PubMed] [CrossRef] [Google Scholar]13. Barr S.I. Effects of dehydration on exercise performance. Can. J. Appl. Physiol. 1999;24:164–172. doi: 10.1139/h99-014. [PubMed] [CrossRef] [Google Scholar]14. Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand. Exercise and fluid replacement.
Trangmar S.J., Gonzalez-Alonso J. Heat, Hydration and the Human Brain, Heart and Skeletal Muscles. Sports Med. 2019;49:69–85. doi: 10.1007/s40279-018-1033-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]11. Cheuvront S.N., Carter R., 3rd, Sawka M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003;2:202–208. doi: 10.1249/00149619-200308000-00006. [PubMed] [CrossRef] [Google Scholar]12. Cheuvront S.N., Kenefick R.W., Montain S.J., Sawka M.N. Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 2010;109:1989–1995. doi: 10.1152/japplphysiol.00367.2010. [PubMed] [CrossRef] [Google Scholar]13. Barr S.I. Effects of dehydration on exercise performance. Can. J. Appl. Physiol. 1999;24:164–172. doi: 10.1139/h99-014. [PubMed] [CrossRef] [Google Scholar]14. Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007;39:377–390. [PubMed] [Google Scholar]15. McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O′Connor F.G., Roberts W.O. National Athletic Trainers′ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [PMC free article] [PubMed] [CrossRef] [Google Scholar]16. Judelson D.A., Maresh C.M., Anderson J.M., Armstrong L.E., Casa D.J., Kraemer W.J., Volek J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007;37:907–921. doi: 10.2165/00007256-200737100-00006. [PubMed] [CrossRef] [Google Scholar]17. Coyle E.F. Physiological determinants of endurance exercise performance. J. Sci. Med. Sport. 1999;2:181–189. doi: 10.1016/S1440-2440(99)80172-8. [PubMed] [CrossRef] [Google Scholar]18. Adams J.D., Sekiguchi Y., Suh H.G., Seal A.D., Sprong C.A., Kirkland T.W., Kavouras S.
Med. Sci. Sports Exerc. 2007;39:377–390. [PubMed] [Google Scholar]15. McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O′Connor F.G., Roberts W.O. National Athletic Trainers′ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [PMC free article] [PubMed] [CrossRef] [Google Scholar]16. Judelson D.A., Maresh C.M., Anderson J.M., Armstrong L.E., Casa D.J., Kraemer W.J., Volek J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007;37:907–921. doi: 10.2165/00007256-200737100-00006. [PubMed] [CrossRef] [Google Scholar]17. Coyle E.F. Physiological determinants of endurance exercise performance. J. Sci. Med. Sport. 1999;2:181–189. doi: 10.1016/S1440-2440(99)80172-8. [PubMed] [CrossRef] [Google Scholar]18. Adams J.D., Sekiguchi Y., Suh H.G., Seal A.D., Sprong C.A., Kirkland T.W., Kavouras S. A. Dehydration Impairs Cycling Performance, Independently of Thirst: A Blinded Study. Med. Sci. Sports Exerc. 2018;50:1697–1703. doi: 10.1249/MSS.0000000000001597. [PubMed] [CrossRef] [Google Scholar]20. Bergeron M.F., Bahr R., Bartsch P., Bourdon L., Calbet J.A.L., Carlsen K.H., Castagna O., González-Alonso J., Lundby C., Maughan R.J., et al. International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br. J. Sports Med. 2012;46:770–779. doi: 10.1136/bjsports-2012-091296. [PubMed] [CrossRef] [Google Scholar]21. Racinais S., Alonso J.M., Coutts A.J., Flouris A.D., Girard O., Gonzalez-Alonso J., Hausswirth C., Jay O., Lee J.K., Mitchell N., et al. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015;49:1164–1173. doi: 10.1136/bjsports-2015-094915. [PMC free article] [PubMed] [CrossRef] [Google Scholar]22. Carter J.E., Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med.
A. Dehydration Impairs Cycling Performance, Independently of Thirst: A Blinded Study. Med. Sci. Sports Exerc. 2018;50:1697–1703. doi: 10.1249/MSS.0000000000001597. [PubMed] [CrossRef] [Google Scholar]20. Bergeron M.F., Bahr R., Bartsch P., Bourdon L., Calbet J.A.L., Carlsen K.H., Castagna O., González-Alonso J., Lundby C., Maughan R.J., et al. International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br. J. Sports Med. 2012;46:770–779. doi: 10.1136/bjsports-2012-091296. [PubMed] [CrossRef] [Google Scholar]21. Racinais S., Alonso J.M., Coutts A.J., Flouris A.D., Girard O., Gonzalez-Alonso J., Hausswirth C., Jay O., Lee J.K., Mitchell N., et al. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015;49:1164–1173. doi: 10.1136/bjsports-2015-094915. [PMC free article] [PubMed] [CrossRef] [Google Scholar]22. Carter J.E., Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med. Sci. Sports Exerc. 1989;21:532–539. doi: 10.1249/00005768-198910000-00007. [PubMed] [CrossRef] [Google Scholar]23. Coyle E.F., Hamilton M. Fluid replacement during exercise: Effects on physiological homeostasis and performance. In: Gisolfi C., Lamb D.R., editors. Fluid Homeostasis During Exercise. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 281–308. [Google Scholar]24. Mora-Rodriguez R., Hamouti N., Del Coso J., Ortega J.F. Fluid ingestion is more effective in preventing hyperthermia in aerobically trained than untrained individuals during exercise in the heat. Appl. Physiol. Nutr. Metab. 2013;38:73–80. doi: 10.1139/apnm-2012-0174. [PubMed] [CrossRef] [Google Scholar]25. Wittels P., Gunga H.C., Kirsch K., Kanduth B., Gunther T., Vormann J., Rocker L. Fluid regulation during prolonged physical strain with water and food deprivation in healthy, trained men. Wien. Klin. Wochenschr. 1996;108:788–794. [PubMed] [Google Scholar]26. Armstrong L.E. Hydration assessment techniques. Nutr.
Sci. Sports Exerc. 1989;21:532–539. doi: 10.1249/00005768-198910000-00007. [PubMed] [CrossRef] [Google Scholar]23. Coyle E.F., Hamilton M. Fluid replacement during exercise: Effects on physiological homeostasis and performance. In: Gisolfi C., Lamb D.R., editors. Fluid Homeostasis During Exercise. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 281–308. [Google Scholar]24. Mora-Rodriguez R., Hamouti N., Del Coso J., Ortega J.F. Fluid ingestion is more effective in preventing hyperthermia in aerobically trained than untrained individuals during exercise in the heat. Appl. Physiol. Nutr. Metab. 2013;38:73–80. doi: 10.1139/apnm-2012-0174. [PubMed] [CrossRef] [Google Scholar]25. Wittels P., Gunga H.C., Kirsch K., Kanduth B., Gunther T., Vormann J., Rocker L. Fluid regulation during prolonged physical strain with water and food deprivation in healthy, trained men. Wien. Klin. Wochenschr. 1996;108:788–794. [PubMed] [Google Scholar]26. Armstrong L.E. Hydration assessment techniques. Nutr. Rev. 2005;63:S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [PubMed] [CrossRef] [Google Scholar]27. Cheuvront S.N., Kenefick R.W. CORP: Improving the status quo for measuring whole body sweat losses. J. Appl. Physiol. 2017;123:632–636. doi: 10.1152/japplphysiol.00433.2017. [PubMed] [CrossRef] [Google Scholar]28. Baker L.B., Lang J.A., Kenney W.L. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur. J. Appl. Physiol. 2009;105:959–967. doi: 10.1007/s00421-009-0982-0. [PubMed] [CrossRef] [Google Scholar]29. Armstrong L.E., Casa D.J. Methods to Evaluate Electrolyte and Water Turnover of Athletes. Athl. Train. Sports Health Care. 2009;1:1–11. doi: 10.3928/19425864-20090625-06. [CrossRef] [Google Scholar]30. Cheuvront S.N., Kenefick R.W. Am I Drinking Enough? Yes, No, and Maybe. J. Am. Coll. Nutr. 2016;35:185–192. doi: 10.1080/07315724.2015.1067872. [PubMed] [CrossRef] [Google Scholar]31. Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M.
Rev. 2005;63:S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [PubMed] [CrossRef] [Google Scholar]27. Cheuvront S.N., Kenefick R.W. CORP: Improving the status quo for measuring whole body sweat losses. J. Appl. Physiol. 2017;123:632–636. doi: 10.1152/japplphysiol.00433.2017. [PubMed] [CrossRef] [Google Scholar]28. Baker L.B., Lang J.A., Kenney W.L. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur. J. Appl. Physiol. 2009;105:959–967. doi: 10.1007/s00421-009-0982-0. [PubMed] [CrossRef] [Google Scholar]29. Armstrong L.E., Casa D.J. Methods to Evaluate Electrolyte and Water Turnover of Athletes. Athl. Train. Sports Health Care. 2009;1:1–11. doi: 10.3928/19425864-20090625-06. [CrossRef] [Google Scholar]30. Cheuvront S.N., Kenefick R.W. Am I Drinking Enough? Yes, No, and Maybe. J. Am. Coll. Nutr. 2016;35:185–192. doi: 10.1080/07315724.2015.1067872. [PubMed] [CrossRef] [Google Scholar]31. Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M. F., Kenefick R.W., LaGasse K.E., Riebe D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [PubMed] [CrossRef] [Google Scholar]32. Cheuvront S.N., Sawka M.N. Hydration Assessment of Athletes. Sports Sci. Exch. 2005;18:1–5. [Google Scholar]33. Stolwijk J.A., Saltin B., Gagge A.P. Physiological factors associated with sweating during exercise. Aerosp. Med. 1968;39:1101–1105. [PubMed] [Google Scholar]34. Parsons K. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance. 3rd ed. CRC Press; Boca Raton, FL, USA: 2014. [Google Scholar]35. Baker L.B., Barnes K.A., Anderson M.L., Passe D.H., Stofan J.R. Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 2016;34:358–368. doi: 10.1080/02640414.2015.1055291. [PubMed] [CrossRef] [Google Scholar]36. Nadel E.R. Control of sweating rate while exercising in the heat. Med. Sci. Sports.
F., Kenefick R.W., LaGasse K.E., Riebe D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [PubMed] [CrossRef] [Google Scholar]32. Cheuvront S.N., Sawka M.N. Hydration Assessment of Athletes. Sports Sci. Exch. 2005;18:1–5. [Google Scholar]33. Stolwijk J.A., Saltin B., Gagge A.P. Physiological factors associated with sweating during exercise. Aerosp. Med. 1968;39:1101–1105. [PubMed] [Google Scholar]34. Parsons K. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance. 3rd ed. CRC Press; Boca Raton, FL, USA: 2014. [Google Scholar]35. Baker L.B., Barnes K.A., Anderson M.L., Passe D.H., Stofan J.R. Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 2016;34:358–368. doi: 10.1080/02640414.2015.1055291. [PubMed] [CrossRef] [Google Scholar]36. Nadel E.R. Control of sweating rate while exercising in the heat. Med. Sci. Sports. 1979;11:31–35. [PubMed] [Google Scholar]37. Horner K.M., Schubert M.M., Desbrow B., Byrne N.M., King N.A. Acute exercise and gastric emptying: A meta-analysis and implications for appetite control. Sports Med. 2015;45:659–678. doi: 10.1007/s40279-014-0285-4. [PubMed] [CrossRef] [Google Scholar]38. Budd G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [PubMed] [CrossRef] [Google Scholar]39. Kulka T.J., Kenney W.L. Heat balance limits in football uniforms how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30:29–39. doi: 10.3810/psm.2002.07.377. [PubMed] [CrossRef] [Google Scholar]40. Armstrong L.E., Johnson E.C., Casa D.J., Ganio M.S., McDermott B.P., Yamamoto L.M., Lopez R.M., Emmanuel H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010;45:117–127. doi: 10.4085/1062-6050-45.2.117. [PMC free article] [PubMed] [CrossRef] [Google Scholar]41.
1979;11:31–35. [PubMed] [Google Scholar]37. Horner K.M., Schubert M.M., Desbrow B., Byrne N.M., King N.A. Acute exercise and gastric emptying: A meta-analysis and implications for appetite control. Sports Med. 2015;45:659–678. doi: 10.1007/s40279-014-0285-4. [PubMed] [CrossRef] [Google Scholar]38. Budd G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [PubMed] [CrossRef] [Google Scholar]39. Kulka T.J., Kenney W.L. Heat balance limits in football uniforms how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30:29–39. doi: 10.3810/psm.2002.07.377. [PubMed] [CrossRef] [Google Scholar]40. Armstrong L.E., Johnson E.C., Casa D.J., Ganio M.S., McDermott B.P., Yamamoto L.M., Lopez R.M., Emmanuel H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010;45:117–127. doi: 10.4085/1062-6050-45.2.117. [PMC free article] [PubMed] [CrossRef] [Google Scholar]41. Hooper D.R., Cook B.M., Comstock B.A., Szivak T.K., Flanagan S.D., Looney D.P., DuPont W.H., Kraemer W.J. Synthetic garments enhance comfort, thermoregulatory response, and athletic performance compared with traditional cotton garments. J. Strength Cond. Res. 2015;29:700–707. doi: 10.1519/JSC.0000000000000783. [PubMed] [CrossRef] [Google Scholar]42. O′Brien C., Freund B.J., Sawka M.N., McKay J., Hesslink R.L., Jones T.E. Hydration assessment during cold-weather military field training exercises. Arct. Med. Res. 1996;55:20–26. [PubMed] [Google Scholar]43. Fusch C., Gfrorer W., Koch C., Thomas A., Grunert A., Moeller H. Water turnover and body composition during long-term exposure to high altitude (4900–7600 m) J. Appl. Physiol. 1996;80:1118–1125. doi: 10.1152/jappl.1996.80.4.1118. [PubMed] [CrossRef] [Google Scholar]44. Mitchell J.W., Nadel E.R., Stolwijk J.A. Respiratory weight losses during exercise. J. Appl. Physiol. 1972;32:474–476. doi: 10.1152/jappl.1972.32.4.474. [PubMed] [CrossRef] [Google Scholar]45.
Hooper D.R., Cook B.M., Comstock B.A., Szivak T.K., Flanagan S.D., Looney D.P., DuPont W.H., Kraemer W.J. Synthetic garments enhance comfort, thermoregulatory response, and athletic performance compared with traditional cotton garments. J. Strength Cond. Res. 2015;29:700–707. doi: 10.1519/JSC.0000000000000783. [PubMed] [CrossRef] [Google Scholar]42. O′Brien C., Freund B.J., Sawka M.N., McKay J., Hesslink R.L., Jones T.E. Hydration assessment during cold-weather military field training exercises. Arct. Med. Res. 1996;55:20–26. [PubMed] [Google Scholar]43. Fusch C., Gfrorer W., Koch C., Thomas A., Grunert A., Moeller H. Water turnover and body composition during long-term exposure to high altitude (4900–7600 m) J. Appl. Physiol. 1996;80:1118–1125. doi: 10.1152/jappl.1996.80.4.1118. [PubMed] [CrossRef] [Google Scholar]44. Mitchell J.W., Nadel E.R., Stolwijk J.A. Respiratory weight losses during exercise. J. Appl. Physiol. 1972;32:474–476. doi: 10.1152/jappl.1972.32.4.474. [PubMed] [CrossRef] [Google Scholar]45. Grundstein A., Williams C., Phan M., Cooper E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015;56:55–60. doi: 10.1016/j.apgeog.2014.10.014. [CrossRef] [Google Scholar]46. Cheuvront S.N., Caruso E.M., Heavens K.R., Karis A.J., Santee W.R., Troyanos C., D′Hemecourt P. Effect of WBGT Index Measurement Location on Heat Stress Category Classification. Med. Sci. Sports Exerc. 2015;47:1958–1964. doi: 10.1249/MSS.0000000000000624. [PubMed] [CrossRef] [Google Scholar]47. Casa D.J., DeMartini J.K., Bergeron M.F., Csillan D., Eichner E.R., Lopez R.M., Ferrara M.S., Miller K.C., O′Connor F., Sawka M.N., et al. National Athletic Trainers′ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]48. Minehan M.R., Riley M.D., Burke L.M. Effect of flavor and awareness of kilojoule content of drinks on preference and fluid balance in team sports.
Grundstein A., Williams C., Phan M., Cooper E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015;56:55–60. doi: 10.1016/j.apgeog.2014.10.014. [CrossRef] [Google Scholar]46. Cheuvront S.N., Caruso E.M., Heavens K.R., Karis A.J., Santee W.R., Troyanos C., D′Hemecourt P. Effect of WBGT Index Measurement Location on Heat Stress Category Classification. Med. Sci. Sports Exerc. 2015;47:1958–1964. doi: 10.1249/MSS.0000000000000624. [PubMed] [CrossRef] [Google Scholar]47. Casa D.J., DeMartini J.K., Bergeron M.F., Csillan D., Eichner E.R., Lopez R.M., Ferrara M.S., Miller K.C., O′Connor F., Sawka M.N., et al. National Athletic Trainers′ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]48. Minehan M.R., Riley M.D., Burke L.M. Effect of flavor and awareness of kilojoule content of drinks on preference and fluid balance in team sports. Int. J. Sport Nutr. Exerc. Metab. 2002;12:81–92. doi: 10.1123/ijsnem.12.1.81. [PubMed] [CrossRef] [Google Scholar]49. Burdon C.A., Johnson N.A., Chapman P.G., O′Connor H.T. Influence of beverage temperature on palatability and fluid ingestion during endurance exercise: A systematic review. Int. J. Sport Nutr. Exerc. Metab. 2012;22:199–211. doi: 10.1123/ijsnem.22.3.199. [PubMed] [CrossRef] [Google Scholar]50. Williams J., Tzortziou Brown V., Malliaras P., Perry M., Kipps C. Hydration strategies of runners in the London Marathon. Clin. J. Sport Med. 2012;22:152–156. doi: 10.1097/JSM.0b013e3182364c45. [PubMed] [CrossRef] [Google Scholar]51. Chorley J., Cianca J., Divine J. Risk factors for exercise-associated hyponatremia in non-elite marathon runners. Clin. J. Sport Med. 2007;17:471–477. doi: 10.1097/JSM.0b013e3181588790. [PubMed] [CrossRef] [Google Scholar]52. Maughan R.J., Shirreffs S.M. Development of individual hydration strategies for athletes. Int. J. Sport Nutr. Exerc. Metab. 2008;18:457–472.
Int. J. Sport Nutr. Exerc. Metab. 2002;12:81–92. doi: 10.1123/ijsnem.12.1.81. [PubMed] [CrossRef] [Google Scholar]49. Burdon C.A., Johnson N.A., Chapman P.G., O′Connor H.T. Influence of beverage temperature on palatability and fluid ingestion during endurance exercise: A systematic review. Int. J. Sport Nutr. Exerc. Metab. 2012;22:199–211. doi: 10.1123/ijsnem.22.3.199. [PubMed] [CrossRef] [Google Scholar]50. Williams J., Tzortziou Brown V., Malliaras P., Perry M., Kipps C. Hydration strategies of runners in the London Marathon. Clin. J. Sport Med. 2012;22:152–156. doi: 10.1097/JSM.0b013e3182364c45. [PubMed] [CrossRef] [Google Scholar]51. Chorley J., Cianca J., Divine J. Risk factors for exercise-associated hyponatremia in non-elite marathon runners. Clin. J. Sport Med. 2007;17:471–477. doi: 10.1097/JSM.0b013e3181588790. [PubMed] [CrossRef] [Google Scholar]52. Maughan R.J., Shirreffs S.M. Development of individual hydration strategies for athletes. Int. J. Sport Nutr. Exerc. Metab. 2008;18:457–472. doi: 10.1123/ijsnem.18.5.457. [PubMed] [CrossRef] [Google Scholar]53. Passe D., Horn M., Stofan J., Horswill C., Murray R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007;17:284–295. doi: 10.1123/ijsnem.17.3.284. [PubMed] [CrossRef] [Google Scholar]54. Hosseinlou A., Khamnei S., Zamanlu M. The effect of water temperature and voluntary drinking on the post rehydration sweating. Int. J. Clin. Exp. Med. 2013;6:683–687. [PMC free article] [PubMed] [Google Scholar]55. Hew-Butler T., Rosner M.H., Fowkes-Godek S., Dugas J.P., Hoffman M.D., Lewis D.P., Maughan R.J., Miller K.C., Montain S.J., Rehrer N.J., et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [PubMed] [CrossRef] [Google Scholar]56. Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis.
doi: 10.1123/ijsnem.18.5.457. [PubMed] [CrossRef] [Google Scholar]53. Passe D., Horn M., Stofan J., Horswill C., Murray R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007;17:284–295. doi: 10.1123/ijsnem.17.3.284. [PubMed] [CrossRef] [Google Scholar]54. Hosseinlou A., Khamnei S., Zamanlu M. The effect of water temperature and voluntary drinking on the post rehydration sweating. Int. J. Clin. Exp. Med. 2013;6:683–687. [PMC free article] [PubMed] [Google Scholar]55. Hew-Butler T., Rosner M.H., Fowkes-Godek S., Dugas J.P., Hoffman M.D., Lewis D.P., Maughan R.J., Miller K.C., Montain S.J., Rehrer N.J., et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [PubMed] [CrossRef] [Google Scholar]56. Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis. Sports Med. 2016;46:1699–1724. doi: 10.1007/s40279-016-0538-5. [PubMed] [CrossRef] [Google Scholar]57. Almond C.S., Shin A.Y., Fortescue E.B., Mannix R.C., Wypij D., Binstadt B.A., Duncan C.N., Olson D.P., Salerno A.E., Newburger J.W. Hyponatremia among runners in the Boston Marathon. N. Engl. J. Med. 2005;352:1550–1556. doi: 10.1056/NEJMoa043901. [PubMed] [CrossRef] [Google Scholar]58. Ishunina T.A., Swaab D.F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus; size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 1999;84:4637–4644. doi: 10.1210/jcem.84.12.6187. [PubMed] [CrossRef] [Google Scholar]59. Sar M., Stumpf W. Simultaneous localization of [3 H] estradiol and neurophysin I or arginine vasopressin in hypothalamic neurons demonstrated by a combined technique of dry-mount autoradiography and immunohistochemistry. Neurosci. Lett. 1980;17:179–184. doi: 10.1016/0304-3940(80)90081-6. [PubMed] [CrossRef] [Google Scholar]60. Barley O.R.
Sports Med. 2016;46:1699–1724. doi: 10.1007/s40279-016-0538-5. [PubMed] [CrossRef] [Google Scholar]57. Almond C.S., Shin A.Y., Fortescue E.B., Mannix R.C., Wypij D., Binstadt B.A., Duncan C.N., Olson D.P., Salerno A.E., Newburger J.W. Hyponatremia among runners in the Boston Marathon. N. Engl. J. Med. 2005;352:1550–1556. doi: 10.1056/NEJMoa043901. [PubMed] [CrossRef] [Google Scholar]58. Ishunina T.A., Swaab D.F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus; size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 1999;84:4637–4644. doi: 10.1210/jcem.84.12.6187. [PubMed] [CrossRef] [Google Scholar]59. Sar M., Stumpf W. Simultaneous localization of [3 H] estradiol and neurophysin I or arginine vasopressin in hypothalamic neurons demonstrated by a combined technique of dry-mount autoradiography and immunohistochemistry. Neurosci. Lett. 1980;17:179–184. doi: 10.1016/0304-3940(80)90081-6. [PubMed] [CrossRef] [Google Scholar]60. Barley O.R. , Chapman D.W., Abbiss C.R. Weight Loss Strategies in Combat Sports and Concerning Habits in Mixed Martial Arts. Int. J. Sports Physiol. Perform. 2018;13:933–939. doi: 10.1123/ijspp.2017-0715. [PubMed] [CrossRef] [Google Scholar]61. Bonci C.M., Bonci L.J., Granger L.R., Johnson C.L., Malina R.M., Milne L.W., Ryan R.R., Vanderbunt E.M. National athletic trainers′ association position statement: Preventing, detecting, and managing disordered eating in athletes. J. Athl Train. 2008;43:80–108. doi: 10.4085/1062-6050-43.1.80. [PMC free article] [PubMed] [CrossRef] [Google Scholar]62. Nuccio R.P., Barnes K.A., Carter J.M., Baker L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017;47:1951–1982. doi: 10.1007/s40279-017-0738-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]63. Garth A.K., Burke L.M. What do athletes drink during competitive sporting activities? Sports Med. 2013;43:539–564. doi: 10.
, Chapman D.W., Abbiss C.R. Weight Loss Strategies in Combat Sports and Concerning Habits in Mixed Martial Arts. Int. J. Sports Physiol. Perform. 2018;13:933–939. doi: 10.1123/ijspp.2017-0715. [PubMed] [CrossRef] [Google Scholar]61. Bonci C.M., Bonci L.J., Granger L.R., Johnson C.L., Malina R.M., Milne L.W., Ryan R.R., Vanderbunt E.M. National athletic trainers′ association position statement: Preventing, detecting, and managing disordered eating in athletes. J. Athl Train. 2008;43:80–108. doi: 10.4085/1062-6050-43.1.80. [PMC free article] [PubMed] [CrossRef] [Google Scholar]62. Nuccio R.P., Barnes K.A., Carter J.M., Baker L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017;47:1951–1982. doi: 10.1007/s40279-017-0738-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]63. Garth A.K., Burke L.M. What do athletes drink during competitive sporting activities? Sports Med. 2013;43:539–564. doi: 10. 1007/s40279-013-0028-y. [PubMed] [CrossRef] [Google Scholar]
1007/s40279-013-0028-y. [PubMed] [CrossRef] [Google Scholar]
Practical Hydration Solutions for Sports
Nutrients. 2019 Jul; 11(7): 1550.
,1,*,2,1,3,4,5,6,7,8,9,1,10,4,11,12,13,14,1,15 and 16
Luke N. Belval
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Yuri Hosokawa
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
Douglas J. Casa
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
William M. Adams
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
Lawrence E. Armstrong
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Lindsay B.
 Baker
Baker
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
Louise Burke
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
Samuel Cheuvront
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
George Chiampas
8U.S. Soccer, Chicago, IL 60616, USA
José González-Alonso
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
Robert A. Huggins
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Stavros A. Kavouras
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
Elaine C. Lee
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Brendon P. McDermott
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
Kevin Miller
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
Zachary Schlader
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
Stacy Sims
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
Rebecca L.
 Stearns
Stearns
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Chris Troyanos
15International Institute of Race Medicine, Plymouth, MA 02360, USA
Jonathan Wingo
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
8U. S. Soccer, Chicago, IL 60616, USA
S. Soccer, Chicago, IL 60616, USA
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
15International Institute of Race Medicine, Plymouth, MA 02360, USA
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
Received 2019 May 15; Accepted 2019 Jul 3.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
Abstract
Personalized hydration strategies play a key role in optimizing the performance and safety of athletes during sporting activities. Clinicians should be aware of the many physiological, behavioral, logistical and psychological issues that determine both the athlete’s fluid needs during sport and his/her opportunity to address them; these are often specific to the environment, the event and the individual athlete. In this paper we address the major considerations for assessing hydration status in athletes and practical solutions to overcome obstacles of a given sport. Based on these solutions, practitioners can better advise athletes to develop practices that optimize hydration for their sports.
Keywords: fluid replacement, athletics, exercise
1.
 Introduction
Introduction
Maintaining euhydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water contributes 50–70% of total body mass and is compartmentalized within both intracellular (65%) and extracellular (35%) spaces [1]. Euhydration is typically maintained over the course of day-to-day life via behavioral and biological controls [2]. However, exercise can cause an acute disruption to fluid balance, challenging the athlete’s goal of optimal performance and safety during exercise, especially in hot environmental conditions. The process of incurring a fluid deficit is known as dehydration, while the outcome is defined as hypohydration. The loss of body water during exercise exacerbates physiological and perceptual strain [3,4,5,6,7,8,9,10] and it is well established that these changes can impair endurance performance, particularly in hot environments and may increase the risk of exertional heat illness [11,12,13,14,15,16,17].
While the sensation of thirst, a centrally mediated response to body water deficits, is useful in dictating the need for fluid intake during daily life, thirst is relatively insensitive in acutely tracking hydration status during exercise [18,19]. Maintaining an optimal state of hydration during exercise becomes more complicated depending on the sport, type of activity and availability of fluid. Optimal hydration is dependent on many factors but can generally be defined during exercise as avoiding losses greater than 2–3% of body mass while also avoiding overhydration [15]. Furthermore, during exercise, it is not uncommon for individuals to involuntarily dehydrate, in which they consume less fluid than their fluid needs. Excessive fluid intake can also be problematic, with hyponatremia developing in severe cases of overhydration [15]. Inappropriate management of fluid intake resulting in hypohydration, or hyperhydration, can be detrimental for performance and in some circumstances, increases health risk.
Current consensus recommends that good hydration practices include: (1) beginning exercise in a state of euhydration, (2) preventing excessive hypohydration during exercise, and (3) replacing remaining losses following exercise prior to the next exercise bout [15,20,21]. These practices attenuate the adverse effects of acute dehydration on physical activity and health [15]. However, it is acknowledged that fluid needs are individualistic and rely on factors such as personal sweat rate, exercise mode, exercise intensity, environmental conditions and exercise duration () [14,15,22,23,24,25]. Furthermore, characteristics and rules unique to each sport environment in which it is played, event uniform and equipment, and the availability of fluid during both training and competition may greatly influence the ability to optimize hydration during activity. The Korey Stringer Institute and Gatorade convened a meeting to address these issues as they relate to athletes. The purpose of these proceedings is to discuss practical strategies to assess and tailor hydration for sports. This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
Factors that contribute to the risk of hypohydration or hyperhydration during exercise.
2. Hydration Assessment
Hydration assessment can be utilized to indicate one’s current hydration state, but if taken serially, it can also be used to track changes in hydration and indicate fluid needs (i.e., during a bout of physical activity). While various methods of hydration assessment exist, there is no single method that can serve as a criterion measure to assess hydration status in all settings (i.e., day-to-day life and exercise, etc.). Plasma osmolality, changes in plasma volume, and the volume, osmolality and specific gravity of urine are the most commonly published metrics to assess changes in hydration status in clinical settings [26]. The use of these measures in field applications is often impractical, due to the methods or equipment needed to acquire the measure (e. g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
In field applications, the careful assessment of changes in body mass over a bout of physical activity provides a reasonably accurate assessment of body water deficits incurred during the session, since sweat loss and fluid intake during the session underpin the major changes in body mass and body water content. This is true for most sporting activities conducted over a duration of <2–3 h; however, during very prolonged and strenuous exercise (e.g., ultra-endurance races), other factors that cause mass changes, metabolic water production and the liberation of stored water become numerically important and undermine the utility of this assessment [15,27,28]. A comparison of body mass pre- and post-exercise will help guide the athlete in understanding whether their hydration strategy during activity was effective in achieving acceptable fluid balance as well as knowing the volume of fluids that are needed following exercise to return to baseline hydration levels prior to the next exercise session. The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
A useful paradigm for tracking daily changes in hydration status in sporting situations is to consider a combination of assessments to track daily changes. The monitoring of daily changes in body mass, coupled with urine color and thirst sensation status provides adequate sensitivity for most athletic situations [30]. Cheuvront and Kenefick established useful criteria for these variables as body mass changes greater than 1.1%, a conscious desire for water (thirst), and dark-colored urine (>5 a.u. on an 8-a.u. scale [31]) indicating varying degrees of fluid inadequacy [32]. Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Practical Solutions:
(1)
Carefully monitor acute changes in body mass over an exercise bout to determine sweat rate, adequacy of fluid replacement and fluid needs for recovery for that session. Consider how well this can be used to evaluate general hydration strategies in similar situations.
(2)
Use changes in body mass, urine color and thirst upon awakening to track daily changes in hydration status.
3. Exercise Structure
Body fluid loss during sport or exercise largely results from sweating. Net fluid balance is modulated to a certain extent by drinking. Rate of sweating is primarily a function of metabolic heat production [33], but can be modified by environment, clothing, acclimatization and hydration status [7,34]. As the primary mechanism of heat dissipation in many environments, the evaporation of sweat is vital for regulating body temperature, even during exercise in temperate weather. However, this heat dissipation is accompanied by typical fluid losses of ~0.5–1.9 L/h [35].
Exercise intensity is the main factor that determines metabolic heat production, meaning that the rate of fluid losses from sweat for a given exercise session can be partially explained by the intensity of the exercise [36]. Total fluid losses are a result of the sweat rate of a given exercise intensity and the total duration of that activity [27]. In most circumstances there is an inverse relationship between the exercise intensity of a session and the duration of that session. However, given the wide variability in individual sweat rates, the unique interplay between intensity, duration and sweat rate must be considered in unison. For example, a runner with a 2 L/h sweat rate who completes a marathon in 2 h will accumulate the same fluid losses as a runner with a 1 L/h sweat rate that completes the race in 4 h. In and , we define exercise intensity of a range of sporting activities into three distinct categories (High, Moderate, Low), based on typical practice and competition structures on the principles described above but comprehensive plans should consider individual athletes.
Table 1
Team Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Basketball | High | High | Low | Low | Mod | Mod | Low | Low |
| Ice Hockey | High | High | Low | Low | Mod | High | Mod | Mod |
| Football | High | High | Mod | Mod | Mod | High | Mod | Mod |
| Baseball | High | High | Mod | Mod | Low | Low | Low | Low |
| Softball | High | High | Mod | Mod | Low | Low | Low | Low |
| Volleyball | High | High | Low | Low | Low | Low | Low | Low |
| Soccer | Mod | Low | Mod | Mod | Mod | High | Mod | High |
| Lacrosse | High | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Rugby | High | Low | Mod | Mod | Mod | High | Mod | High |
Table 2
Individual Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Tennis | High | Mod | Mod | Mod | High | High | Mod | Mod |
| Wrestling | High | High | Mod | Mod | High | High | High | Low |
| Gymnastics | High | High | Low | Low | Mod | Low | Low | Low |
| Running (<1 h) | Low | High | Mod | Mod | High | High | Low | Low |
| Running (1–2 h) | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Running (>2 h) | Low | High | Mod | Mod | Low | Mod | Mod | Mod |
| Cycling (<1 h) | High | High | Mod | Mod | High | High | Low | Low |
| Cycling (>2 h) | Mod | Mod | Mod | Mod | Mod | Mod | Low | High |
| Swimming | High | High | Low | Low | High | High | Low | Low |
| Triathlon (<2 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (2–5 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (5–9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Triathlon (>9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
For sports like cycling and running, the influence of exercise intensity and duration on fluid needs is very easy to determine given the consistent nature of exercise. demonstrates the relationship between duration and target fluid replacement for steady-state exercise. However, as shown in , some of the most common sports involve supramaximal exercise in short bursts with longer breaks. In this case, individuals should regard an overall average of exercise intensity rather than the maximal effort during the exercise bout when determining optimal fluid balance.
Target fluid replacement estimates to prevent >2 ± 1 % body mass (BM) loss as water (i.e., dehydration). The 70 kg athlete in the example would need to drink a volume of fluid equal to 2.6 ± 0.7 L to prevent >2 ± 1% dehydration when losing 4 L of body water, such as during a marathon (42.1 km). During shorter distances such as 5 or 10 km when fluid losses are unlikely to reach or exceed 2% dehydration, the same athlete would not need to ingest fluids during competition as fluid losses accumulate to <2% dehydration.
It should also be noted that exercise intensity influences gastric emptying rate [37]. Individuals striving to closely match sweat losses with fluid consumption can be challenged by maximal gastric emptying rates. However, when vigorous exercise is conducted (>70% VO2max), gastric emptying decreases predictably, most likely based on decreased splanchnic perfusion [37].
Practical Solutions:
(1)
Increased fluid intake is necessary with prolonged or intense exercise due to increased sweat production.
(2)
During vigorous exercise (>70% VO2max) understand that gastric emptying may limit fluid absorption. Athletes can train their gut to improve gastrointestinal comfort or adopt strategies to increase fluid intake before and after exercise.
4. Environment
At a fixed exercise intensity, the ambient environment further modulates sweat rate. The magnitude of evaporative, radiant, convective and conductive heat exchange between the body and the environment is a function of the gradients between the environment and the skin which provides the main physiological interface for heat exchange. A number of factors contribute to sweat rate including ambient and radiant temperature, humidity, clothing, and air velocity [34], all of which differ depending on the sport or activity ( and ). Therefore, individuals exercising in hot-humid environments with direct sunlight and minimal airflow will produce near maximal sweat rates and be at the greatest risk of hypohydration. Wet-bulb globe thermometry (WBGT) accounts for these environmental factors and can help inform fluid replacement decisions [38].
All clothing provides insulation and presents a barrier to heat loss, resulting in increased sweat rates to provide similar cooling to an unclothed situation [34]. Thus, sports/activities with specific clothing requirements, such as American football [39,40], are at greater risk of body fluid loss compared to similar activities in which clothing is minimal. Synthetic wicking materials can increase sweat fluid losses compared to cotton garments [41], potentially decreasing the thermal load but increasing the risk of dehydration. When the effects of hot, humid environmental conditions are combined with clothing and equipment, individuals can achieve near maximal sweat rates which can create a significant fluid deficit rapidly [40].
Other Environmental Considerations:
Exercising in the cold, or at high altitudes merits special considerations when determining the fluid needs of athletes. Athletes must also be vigilant and mindful of their fluid needs during exercise in the cold. Exercise in the cold can still produce copious sweating, especially when heavy clothing is worn, while also diminishing thirst sensitivity and reducing ad libitum fluid consumption, thus potentially leading to impaired fluid replacement and hypohydration [42]. If possible, athletes should know their individual fluid replacement needs, based upon sweat rate measurement, during exercise in hot and cold environments to ensure they can develop a plan for competing while optimally hydrated.
Athletes unaccustomed to exercising in higher altitudes may require additional fluids. Very high altitude (4900–7600 m) exposure tends to increase water and electrolyte losses, decrease plasma volume and total body water content [43]. In both cold air and high altitudes, respiratory water losses may increase and require additional fluid consumption due to low air water vapor pressures [44]. Therefore, athletes should acclimate to altitude over several days and maintain euhydration prior to competition to ensure optimal athletic performance.
and summarizes typical environmental conditions found among a range of sports into three distinct categories, and how these conditions contribute to the considerations around an individualized fluid plan. Of course, there are large regional differences in environmental conditions experienced for sports at the same time of year [45]. Local measurements utilizing WBGT allow for the greatest characterization of the environmental demands placed on athletes during exercise in the heat [46].
Practical Solutions:
(1)
Measure local environmental conditions to determine the risk of high sweat rates resulting in large fluid losses.
(2)
Increase fluid-replacement during exercise in hot and humid environments to account for increased sweat losses.
(3)
Account for clothing or equipment requirements when evaluating fluid needs.
(4)
Modify fluid intake when exercising in cold or altitude according to an estimation of fluid losses noting that thirst may be less reliable as a guide to dehydration under these conditions.
5. Fluid Availability
Fluid availability refers to the factors that dictate an athlete’s ability to replace fluid losses during activity. In many instances, the characteristics of the sport have a strong influence on the ability to drink during competition and in many scenarios prevent an athlete from “drinking to thirst” [21]. Meanwhile, training activities are often easily modified to allow for some degree of fluid replacement. In many instances, water-breaks during training can be determined on the basis of work-to-rest ratios set by environmental conditions with free access to fluid throughout the break [47]. Characteristics such as flavor and temperature affect the palatability of fluids and may increase voluntary intake when they are matched to the cultural preferences of the athletes and the prevailing conditions (e.g., cool drinks in a warm environment) [48,49].
In endurance sports which provide competitors with feed zones/water stations (e.g., running events), the number of water stations on a course and the frequency with which a competitor reaches them can influence drinking behavior. The International Association of Athletics Federations recommends that stations are placed approximately every 5 km, however, many races include more frequent stations which may influence athletes’ drinking strategies and behaviors [50]. Slower athletes with lower sweat rates who compete in such events, particularly over prolonged distances or duration, are often able to drink in volumes that exceed their true fluid losses and are at particular risk of developing hyponatremia [51]. Athletes taking part in these events should be educated on the importance of fluid balance and the prevention of hyperhydration. It should also be noted that in many events lasting up to 45 min, the risk of dehydration is low due to the limited duration across which sweat losses can accumulate. For faster and/or more competitive athletes, extra elements related to drinking while performing continuous exercise must be taken into consideration. This includes considerations around gastrointestinal comfort when fluid consumed during higher-intensity and “gut joggling” activities (e.g., high-speed running vs. the more “gliding” movements of cross-country skiing or cycling). Furthermore, the time lost in slowing down or moving out of an aerodynamic position to obtain or consume a drink must be factored into the overall race performance. This creates different factors in the cost:benefit analysis of an individual’s fluid intake plan.
The official rules and competition characteristics of “stop-start” sports such as team and racket sports create other influences, and often unique scenarios, around fluid availability. In some examples (e.g., soccer, rugby), governing rules limit the availability of fluids for athletes during competition. Soccer, for example, includes two 45-min halves (with a continuous running clock) in which fluid availability is extremely limited to players. At the other end of the spectrum are sports such as baseball, basketball and tennis with frequent rest breaks within playing time (e.g., time outs, change of ends or player rotations) during which fluids can be consumed. An athlete’s drinking strategy for a competition represents a unique instance for their particular sport based on their ability to rehydrate within the rules [52]. We support recent governing body rule changes and referee decisions to add breaks to competitions (Major League Soccer, FIFA soccer matches, US Open Tennis) to facilitate safe participation by the athletes. These changes likely augment athletic performance and safety simultaneously. Individuals should understand their sport and its fluid needs/fluid availability characteristics to prepare and practice optimal fluid plans for competition. Where rule changes, or alterations are allowed, individuals and teams should attempt to ask for these alterations (e.g., extended rest periods, additional breaks) in advance to formulate an appropriate drinking strategy. In all sports, athletes should aim to practice and fine-tune their personal drinking strategy for race/competition conditions. This will help individuals to confirm its feasibility, understand their personal responses and develop any necessary behavioral practices within the expected rules of competition.
In and , we define fluid availability into three distinct categories, based on particular sport variations. Sports were categorized as having high fluid availability if there are multiple opportunities for fluid consumption, rather than only during breaks. Low fluid availability was used to describe those activities involving governing rules, time constraints, or an inability to carry personal fluids during competition. Accessibility to fluid consumption during competition represents a major variable to be used in preparation of an optimal fluid replacement strategy.
Practical Solutions:
(1)
During training, ensure that there is ample access to fluids that are palatable to athletes.
(2)
Investigate or understand the opportunities for fluid intake during that are specific to a sport or event, and any other practical issues that determine fluid intake.
(3)
Consider the risks of hyperhydration as well as hypohydration for any sporting event or individual athlete, and prepare appropriate practice and education strategies.
(4)
Develop personalized fluid intake plans that incorporate fluid availability characteristics of the sport or event. Where there is a likelihood of hypohydration, be proactive and creative in making use of existing opportunities for fluid intake within sport rules and characteristics and be prepared to request for changes when there is a likelihood of a serious mismatch between fluid losses and the opportunity to address these.
(5)
Practice intended competition drinking plans ahead of time to determine their suitability and allow time for readjustment.
6. Intrinsic Factors
A number of intrinsic factors modulate the individual variances that are observed in fluid losses. One of the greatest considerations for an individual’s sweat rate is his or her body size. Larger individuals typically have higher sweat losses, with football linemen exhibiting some of the highest recorded sweat rates [14]. Therefore, required absolute drink volumes will be higher for these athletes. An individual’s thirst drive also dictates how much they desire to drink during exercise, but this may not match their actual fluid needs. Indeed, multiple authors report that athletes voluntarily dehydrate during exercise due to discrepancies in fluid losses and drinking behavior [53,54]. Case studies of individuals who have developed hyponatremia due to excessive drinking during exercise also note that they reported thirst as an underlying contributor to their fluid intake [55].
Heat acclimatization contributes to variations in an individual’s sweating rate responses. Individuals who are heat acclimatized exhibit greater sweat rates which can pose a greater risk of hypohydration [56]. Although the increased sweat provides extra heat dissipation, it also requires extra fluid intake.
Women may be at greater risk for exercise-induced hyponatremia. This risk has been attributed to their lower body weight and size, excess water ingestion, and longer racing times relative to men [57]. The greater incidence of hyponatremia in women is unlikely due to their greater levels of estradiol in plasma and tissue. Although female sex-hormones can also influence neural and hormonal control of thirst, fluid intake, sodium appetite and sodium regulation [58,59], there is no evidence that anything beyond stature and drinking behavior significantly impact their risk.
Practical Solutions:
7. Sport-Specific Factors
Weight Division, Acrobatic and Appearance-Based Sports
The culture and normal behaviors surrounding specific sports can greatly affect the hydration practices of its athletes. The three most prominent examples of the cultural effects of sports on hydration practices are weight division sports, acrobatic sports and appearance-based sports. In weight division sports (e.g., combat sports, horse racing, lightweight rowing, etc.), the practice of deliberately dehydrating to manipulate body mass to meet lighter competition weight classifications is common [60]. In many cases, athletes not only sacrifice their performance through these practices but also endanger their health and well-being. In a similar fashion, sports where body-image and appearance are emphasized (e.g., cheerleading, body building and gymnastics), dangerous practices, such as extreme fluid restriction may be used by athletes to cheat “unofficial” weight checks that are self-instigated or expected within their training environment. Finally, “acrobatic” feats such as gymnastics, jumping and climbing are aided by a high power to weight ratio, but should not rely on severe hypohydration to achieve this. Excessive use of dehydration to manage body mass goals should be corrected to avoid long-term health complications [61].
Practical Solutions:
8. Conclusions
Based on the factors in the above sections, along with published literature on typical fluid balance observations in various sports [62,63], we assigned risks of hypohydration to the sports in and . These determinations can be used as a general guideline for sports that pose large risks for fluid imbalances that may limit sport performance. The factors for individual situations or geographical locations may vary and should be considered based on the principles mentioned above to tailor the necessary fluid replacement accommodations. An example of using this paradigm to develop a hydration plan can be found in .
Table 3
Establishing a Hydration Plan.
| Guiding Question | Steps to Correct | Implementation Example |
|---|---|---|
| Are athletes in a state of optimal hydration? | ||
| Is the exercise prolonged or intense? | ||
| Is the exercise being performed in environmental conditions that lead to greater fluid losses? | ||
| Is fluid available throughout the entire duration of exercise? |
| |
| Are there individuals with intrinsic risk factors? |
| |
| Are there sport-specific factors that need to be considered? |
In this paper we present a paradigm that can be used by clinicians and practitioners to develop hydration strategies for sports based on fluid availability, environment and exercise intensity. These tools are provided to inform hydration education and practices in a dynamic and individualized manner so that athletes can adapt to different circumstances and optimize performance.
Author Contributions
All authors attended the meeting and contributed to drafting and revision of the manuscript. All authors approved the final version of the paper.
Funding
The meeting preceding this manuscript was funded by PepsiCo (Gatorade).
Conflicts of Interest
Douglas Casa is the Chief Executive Officer of the Korey Stringer Institute, a 503.c not for profit which subsists on the donations from our corporate partners who include Gatorade, CamelBak, NFL, NATA, Mission, Eagle Pharmaceuticals and Kestrel. He has also been a recipient of grant funds from the following entities to study hydration related products: GE Healthcare, Halo Wearables, Nix Inc., CamelBak. William Adams has consulted with the following entities regarding hydration and exercise performance or the development of hydration assessment devices: BSX Athletics; Samsung Oak Holdings, Inc; Nobo, Inc; Clif Bar &Company; The Gatorade Company, Inc. Lawrence Armstrong is a hydration consultant to Danone Nutricia Research, France and the Drinking Water Research Foundation, Alexandria VA, USA. Lindsay Baker is employed by the Gatorade Sports Science Institute, a division of PepsiCo, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc. Louise Burke was a member of the Gatorade Sports Science Institute’s Expert Panel from 2014–2015 for which her workplace received an honorarium. Jose Gonzalez-Alonso was a member of the Gatorade Sports Science Institute’s Expert Panel in 2017 for which his workplace received an honorarium. Stavros Kavouras has served as scientific consultant for Quest Diagnostics, Standard Process and Danone Research and has active grants with Danone Research. The funders had no role in the in the writing of the manuscript.
References
1. Sawka M., Pandolf K.B. Effects of body water loss on physiological function and exercise performance. In: Gisolfi C., Lamb D.R., editors. Perspectives in Exercise Science and Sports Medicine. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 1–38. [Google Scholar]2. Sawka M.N., Wenger C.B., Pandolf K.B. Thermoregulatory Responses to Acute Exercise-Heat Stress and Heat Acclimation. In: Terjung R., editor. Comprehensive Physiology. John Wiley & Sons; Hoboken, NJ, USA: 2011. pp. 97–151. [Google Scholar]3. Montain S.J., Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [PubMed] [CrossRef] [Google Scholar]4. Montain S.J., Sawka M.N., Latzka W.A., Valeri C.R. Thermal and cardiovascular strain from hypohydration: Influence of exercise intensity. Int. J. Sports Med. 1998;19:87–91. doi: 10.1055/s-2007-971887. [PubMed] [CrossRef] [Google Scholar]5. Sawka M.N., Young A.J., Francesconi R.P., Muza S.R., Pandolf K.B. Thermoregulatory and blood responses during exercise at graded hypohydration levels. J. Appl. Physiol. 1985;59:1394–1401. doi: 10.1152/jappl.1985.59.5.1394. [PubMed] [CrossRef] [Google Scholar]6. Adams W.M., Ferraro E.M., Huggins R.A., Casa D.J. Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 2014;28:2380–2389. doi: 10.1519/JSC.0000000000000501. [PubMed] [CrossRef] [Google Scholar]7. Kenefick R.W., Cheuvront S.N. Physiological adjustments to hypohydration: Impact on thermoregulation. Auton. Neurosci. 2016;196:47–51. doi: 10.1016/j.autneu.2016.02.003. [PubMed] [CrossRef] [Google Scholar]8. Trangmar S.J., Gonzalez-Alonso J. New Insights into the Impact of Dehydration on Blood Flow and Metabolism during Exercise. Exerc. Sport Sci. Rev. 2017;45:146–153. doi: 10.1249/JES.0000000000000109. [PubMed] [CrossRef] [Google Scholar]9. Gonzalez-Alonso J., Crandall C.G., Johnson J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008;586:45–53. doi: 10.1113/jphysiol.2007.142158. [PMC free article] [PubMed] [CrossRef] [Google Scholar]10. Trangmar S.J., Gonzalez-Alonso J. Heat, Hydration and the Human Brain, Heart and Skeletal Muscles. Sports Med. 2019;49:69–85. doi: 10.1007/s40279-018-1033-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]11. Cheuvront S.N., Carter R., 3rd, Sawka M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003;2:202–208. doi: 10.1249/00149619-200308000-00006. [PubMed] [CrossRef] [Google Scholar]12. Cheuvront S.N., Kenefick R.W., Montain S.J., Sawka M.N. Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 2010;109:1989–1995. doi: 10.1152/japplphysiol.00367.2010. [PubMed] [CrossRef] [Google Scholar]13. Barr S.I. Effects of dehydration on exercise performance. Can. J. Appl. Physiol. 1999;24:164–172. doi: 10.1139/h99-014. [PubMed] [CrossRef] [Google Scholar]14. Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007;39:377–390. [PubMed] [Google Scholar]15. McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O′Connor F.G., Roberts W.O. National Athletic Trainers′ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [PMC free article] [PubMed] [CrossRef] [Google Scholar]16. Judelson D.A., Maresh C.M., Anderson J.M., Armstrong L.E., Casa D.J., Kraemer W.J., Volek J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007;37:907–921. doi: 10.2165/00007256-200737100-00006. [PubMed] [CrossRef] [Google Scholar]17. Coyle E.F. Physiological determinants of endurance exercise performance. J. Sci. Med. Sport. 1999;2:181–189. doi: 10.1016/S1440-2440(99)80172-8. [PubMed] [CrossRef] [Google Scholar]18. Adams J.D., Sekiguchi Y., Suh H.G., Seal A.D., Sprong C.A., Kirkland T.W., Kavouras S.A. Dehydration Impairs Cycling Performance, Independently of Thirst: A Blinded Study. Med. Sci. Sports Exerc. 2018;50:1697–1703. doi: 10.1249/MSS.0000000000001597. [PubMed] [CrossRef] [Google Scholar]20. Bergeron M.F., Bahr R., Bartsch P., Bourdon L., Calbet J.A.L., Carlsen K.H., Castagna O., González-Alonso J., Lundby C., Maughan R.J., et al. International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br. J. Sports Med. 2012;46:770–779. doi: 10.1136/bjsports-2012-091296. [PubMed] [CrossRef] [Google Scholar]21. Racinais S., Alonso J.M., Coutts A.J., Flouris A.D., Girard O., Gonzalez-Alonso J., Hausswirth C., Jay O., Lee J.K., Mitchell N., et al. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015;49:1164–1173. doi: 10.1136/bjsports-2015-094915. [PMC free article] [PubMed] [CrossRef] [Google Scholar]22. Carter J.E., Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med. Sci. Sports Exerc. 1989;21:532–539. doi: 10.1249/00005768-198910000-00007. [PubMed] [CrossRef] [Google Scholar]23. Coyle E.F., Hamilton M. Fluid replacement during exercise: Effects on physiological homeostasis and performance. In: Gisolfi C., Lamb D.R., editors. Fluid Homeostasis During Exercise. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 281–308. [Google Scholar]24. Mora-Rodriguez R., Hamouti N., Del Coso J., Ortega J.F. Fluid ingestion is more effective in preventing hyperthermia in aerobically trained than untrained individuals during exercise in the heat. Appl. Physiol. Nutr. Metab. 2013;38:73–80. doi: 10.1139/apnm-2012-0174. [PubMed] [CrossRef] [Google Scholar]25. Wittels P., Gunga H.C., Kirsch K., Kanduth B., Gunther T., Vormann J., Rocker L. Fluid regulation during prolonged physical strain with water and food deprivation in healthy, trained men. Wien. Klin. Wochenschr. 1996;108:788–794. [PubMed] [Google Scholar]26. Armstrong L.E. Hydration assessment techniques. Nutr. Rev. 2005;63:S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [PubMed] [CrossRef] [Google Scholar]27. Cheuvront S.N., Kenefick R.W. CORP: Improving the status quo for measuring whole body sweat losses. J. Appl. Physiol. 2017;123:632–636. doi: 10.1152/japplphysiol.00433.2017. [PubMed] [CrossRef] [Google Scholar]28. Baker L.B., Lang J.A., Kenney W.L. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur. J. Appl. Physiol. 2009;105:959–967. doi: 10.1007/s00421-009-0982-0. [PubMed] [CrossRef] [Google Scholar]29. Armstrong L.E., Casa D.J. Methods to Evaluate Electrolyte and Water Turnover of Athletes. Athl. Train. Sports Health Care. 2009;1:1–11. doi: 10.3928/19425864-20090625-06. [CrossRef] [Google Scholar]30. Cheuvront S.N., Kenefick R.W. Am I Drinking Enough? Yes, No, and Maybe. J. Am. Coll. Nutr. 2016;35:185–192. doi: 10.1080/07315724.2015.1067872. [PubMed] [CrossRef] [Google Scholar]31. Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M.F., Kenefick R.W., LaGasse K.E., Riebe D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [PubMed] [CrossRef] [Google Scholar]32. Cheuvront S.N., Sawka M.N. Hydration Assessment of Athletes. Sports Sci. Exch. 2005;18:1–5. [Google Scholar]33. Stolwijk J.A., Saltin B., Gagge A.P. Physiological factors associated with sweating during exercise. Aerosp. Med. 1968;39:1101–1105. [PubMed] [Google Scholar]34. Parsons K. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance. 3rd ed. CRC Press; Boca Raton, FL, USA: 2014. [Google Scholar]35. Baker L.B., Barnes K.A., Anderson M.L., Passe D.H., Stofan J.R. Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 2016;34:358–368. doi: 10.1080/02640414.2015.1055291. [PubMed] [CrossRef] [Google Scholar]36. Nadel E.R. Control of sweating rate while exercising in the heat. Med. Sci. Sports. 1979;11:31–35. [PubMed] [Google Scholar]37. Horner K.M., Schubert M.M., Desbrow B., Byrne N.M., King N.A. Acute exercise and gastric emptying: A meta-analysis and implications for appetite control. Sports Med. 2015;45:659–678. doi: 10.1007/s40279-014-0285-4. [PubMed] [CrossRef] [Google Scholar]38. Budd G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [PubMed] [CrossRef] [Google Scholar]39. Kulka T.J., Kenney W.L. Heat balance limits in football uniforms how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30:29–39. doi: 10.3810/psm.2002.07.377. [PubMed] [CrossRef] [Google Scholar]40. Armstrong L.E., Johnson E.C., Casa D.J., Ganio M.S., McDermott B.P., Yamamoto L.M., Lopez R.M., Emmanuel H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010;45:117–127. doi: 10.4085/1062-6050-45.2.117. [PMC free article] [PubMed] [CrossRef] [Google Scholar]41. Hooper D.R., Cook B.M., Comstock B.A., Szivak T.K., Flanagan S.D., Looney D.P., DuPont W.H., Kraemer W.J. Synthetic garments enhance comfort, thermoregulatory response, and athletic performance compared with traditional cotton garments. J. Strength Cond. Res. 2015;29:700–707. doi: 10.1519/JSC.0000000000000783. [PubMed] [CrossRef] [Google Scholar]42. O′Brien C., Freund B.J., Sawka M.N., McKay J., Hesslink R.L., Jones T.E. Hydration assessment during cold-weather military field training exercises. Arct. Med. Res. 1996;55:20–26. [PubMed] [Google Scholar]43. Fusch C., Gfrorer W., Koch C., Thomas A., Grunert A., Moeller H. Water turnover and body composition during long-term exposure to high altitude (4900–7600 m) J. Appl. Physiol. 1996;80:1118–1125. doi: 10.1152/jappl.1996.80.4.1118. [PubMed] [CrossRef] [Google Scholar]44. Mitchell J.W., Nadel E.R., Stolwijk J.A. Respiratory weight losses during exercise. J. Appl. Physiol. 1972;32:474–476. doi: 10.1152/jappl.1972.32.4.474. [PubMed] [CrossRef] [Google Scholar]45. Grundstein A., Williams C., Phan M., Cooper E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015;56:55–60. doi: 10.1016/j.apgeog.2014.10.014. [CrossRef] [Google Scholar]46. Cheuvront S.N., Caruso E.M., Heavens K.R., Karis A.J., Santee W.R., Troyanos C., D′Hemecourt P. Effect of WBGT Index Measurement Location on Heat Stress Category Classification. Med. Sci. Sports Exerc. 2015;47:1958–1964. doi: 10.1249/MSS.0000000000000624. [PubMed] [CrossRef] [Google Scholar]47. Casa D.J., DeMartini J.K., Bergeron M.F., Csillan D., Eichner E.R., Lopez R.M., Ferrara M.S., Miller K.C., O′Connor F., Sawka M.N., et al. National Athletic Trainers′ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]48. Minehan M.R., Riley M.D., Burke L.M. Effect of flavor and awareness of kilojoule content of drinks on preference and fluid balance in team sports. Int. J. Sport Nutr. Exerc. Metab. 2002;12:81–92. doi: 10.1123/ijsnem.12.1.81. [PubMed] [CrossRef] [Google Scholar]49. Burdon C.A., Johnson N.A., Chapman P.G., O′Connor H.T. Influence of beverage temperature on palatability and fluid ingestion during endurance exercise: A systematic review. Int. J. Sport Nutr. Exerc. Metab. 2012;22:199–211. doi: 10.1123/ijsnem.22.3.199. [PubMed] [CrossRef] [Google Scholar]50. Williams J., Tzortziou Brown V., Malliaras P., Perry M., Kipps C. Hydration strategies of runners in the London Marathon. Clin. J. Sport Med. 2012;22:152–156. doi: 10.1097/JSM.0b013e3182364c45. [PubMed] [CrossRef] [Google Scholar]51. Chorley J., Cianca J., Divine J. Risk factors for exercise-associated hyponatremia in non-elite marathon runners. Clin. J. Sport Med. 2007;17:471–477. doi: 10.1097/JSM.0b013e3181588790. [PubMed] [CrossRef] [Google Scholar]52. Maughan R.J., Shirreffs S.M. Development of individual hydration strategies for athletes. Int. J. Sport Nutr. Exerc. Metab. 2008;18:457–472. doi: 10.1123/ijsnem.18.5.457. [PubMed] [CrossRef] [Google Scholar]53. Passe D., Horn M., Stofan J., Horswill C., Murray R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007;17:284–295. doi: 10.1123/ijsnem.17.3.284. [PubMed] [CrossRef] [Google Scholar]54. Hosseinlou A., Khamnei S., Zamanlu M. The effect of water temperature and voluntary drinking on the post rehydration sweating. Int. J. Clin. Exp. Med. 2013;6:683–687. [PMC free article] [PubMed] [Google Scholar]55. Hew-Butler T., Rosner M.H., Fowkes-Godek S., Dugas J.P., Hoffman M.D., Lewis D.P., Maughan R.J., Miller K.C., Montain S.J., Rehrer N.J., et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [PubMed] [CrossRef] [Google Scholar]56. Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis. Sports Med. 2016;46:1699–1724. doi: 10.1007/s40279-016-0538-5. [PubMed] [CrossRef] [Google Scholar]57. Almond C.S., Shin A.Y., Fortescue E.B., Mannix R.C., Wypij D., Binstadt B.A., Duncan C.N., Olson D.P., Salerno A.E., Newburger J.W. Hyponatremia among runners in the Boston Marathon. N. Engl. J. Med. 2005;352:1550–1556. doi: 10.1056/NEJMoa043901. [PubMed] [CrossRef] [Google Scholar]58. Ishunina T.A., Swaab D.F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus; size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 1999;84:4637–4644. doi: 10.1210/jcem.84.12.6187. [PubMed] [CrossRef] [Google Scholar]59. Sar M., Stumpf W. Simultaneous localization of [3 H] estradiol and neurophysin I or arginine vasopressin in hypothalamic neurons demonstrated by a combined technique of dry-mount autoradiography and immunohistochemistry. Neurosci. Lett. 1980;17:179–184. doi: 10.1016/0304-3940(80)90081-6. [PubMed] [CrossRef] [Google Scholar]60. Barley O.R., Chapman D.W., Abbiss C.R. Weight Loss Strategies in Combat Sports and Concerning Habits in Mixed Martial Arts. Int. J. Sports Physiol. Perform. 2018;13:933–939. doi: 10.1123/ijspp.2017-0715. [PubMed] [CrossRef] [Google Scholar]61. Bonci C.M., Bonci L.J., Granger L.R., Johnson C.L., Malina R.M., Milne L.W., Ryan R.R., Vanderbunt E.M. National athletic trainers′ association position statement: Preventing, detecting, and managing disordered eating in athletes. J. Athl Train. 2008;43:80–108. doi: 10.4085/1062-6050-43.1.80. [PMC free article] [PubMed] [CrossRef] [Google Scholar]62. Nuccio R.P., Barnes K.A., Carter J.M., Baker L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017;47:1951–1982. doi: 10.1007/s40279-017-0738-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]63. Garth A.K., Burke L.M. What do athletes drink during competitive sporting activities? Sports Med. 2013;43:539–564. doi: 10.1007/s40279-013-0028-y. [PubMed] [CrossRef] [Google Scholar]
Practical Hydration Solutions for Sports
Nutrients. 2019 Jul; 11(7): 1550.
,1,*,2,1,3,4,5,6,7,8,9,1,10,4,11,12,13,14,1,15 and 16
Luke N. Belval
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Yuri Hosokawa
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
Douglas J. Casa
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
William M. Adams
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
Lawrence E. Armstrong
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Lindsay B. Baker
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
Louise Burke
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
Samuel Cheuvront
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
George Chiampas
8U.S. Soccer, Chicago, IL 60616, USA
José González-Alonso
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
Robert A. Huggins
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Stavros A. Kavouras
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
Elaine C. Lee
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Brendon P. McDermott
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
Kevin Miller
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
Zachary Schlader
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
Stacy Sims
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
Rebecca L. Stearns
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Chris Troyanos
15International Institute of Race Medicine, Plymouth, MA 02360, USA
Jonathan Wingo
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
8U.S. Soccer, Chicago, IL 60616, USA
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
15International Institute of Race Medicine, Plymouth, MA 02360, USA
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
Received 2019 May 15; Accepted 2019 Jul 3.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
Abstract
Personalized hydration strategies play a key role in optimizing the performance and safety of athletes during sporting activities. Clinicians should be aware of the many physiological, behavioral, logistical and psychological issues that determine both the athlete’s fluid needs during sport and his/her opportunity to address them; these are often specific to the environment, the event and the individual athlete. In this paper we address the major considerations for assessing hydration status in athletes and practical solutions to overcome obstacles of a given sport. Based on these solutions, practitioners can better advise athletes to develop practices that optimize hydration for their sports.
Keywords: fluid replacement, athletics, exercise
1. Introduction
Maintaining euhydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water contributes 50–70% of total body mass and is compartmentalized within both intracellular (65%) and extracellular (35%) spaces [1]. Euhydration is typically maintained over the course of day-to-day life via behavioral and biological controls [2]. However, exercise can cause an acute disruption to fluid balance, challenging the athlete’s goal of optimal performance and safety during exercise, especially in hot environmental conditions. The process of incurring a fluid deficit is known as dehydration, while the outcome is defined as hypohydration. The loss of body water during exercise exacerbates physiological and perceptual strain [3,4,5,6,7,8,9,10] and it is well established that these changes can impair endurance performance, particularly in hot environments and may increase the risk of exertional heat illness [11,12,13,14,15,16,17].
While the sensation of thirst, a centrally mediated response to body water deficits, is useful in dictating the need for fluid intake during daily life, thirst is relatively insensitive in acutely tracking hydration status during exercise [18,19]. Maintaining an optimal state of hydration during exercise becomes more complicated depending on the sport, type of activity and availability of fluid. Optimal hydration is dependent on many factors but can generally be defined during exercise as avoiding losses greater than 2–3% of body mass while also avoiding overhydration [15]. Furthermore, during exercise, it is not uncommon for individuals to involuntarily dehydrate, in which they consume less fluid than their fluid needs. Excessive fluid intake can also be problematic, with hyponatremia developing in severe cases of overhydration [15]. Inappropriate management of fluid intake resulting in hypohydration, or hyperhydration, can be detrimental for performance and in some circumstances, increases health risk.
Current consensus recommends that good hydration practices include: (1) beginning exercise in a state of euhydration, (2) preventing excessive hypohydration during exercise, and (3) replacing remaining losses following exercise prior to the next exercise bout [15,20,21]. These practices attenuate the adverse effects of acute dehydration on physical activity and health [15]. However, it is acknowledged that fluid needs are individualistic and rely on factors such as personal sweat rate, exercise mode, exercise intensity, environmental conditions and exercise duration () [14,15,22,23,24,25]. Furthermore, characteristics and rules unique to each sport environment in which it is played, event uniform and equipment, and the availability of fluid during both training and competition may greatly influence the ability to optimize hydration during activity. The Korey Stringer Institute and Gatorade convened a meeting to address these issues as they relate to athletes. The purpose of these proceedings is to discuss practical strategies to assess and tailor hydration for sports. This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
Factors that contribute to the risk of hypohydration or hyperhydration during exercise.
2. Hydration Assessment
Hydration assessment can be utilized to indicate one’s current hydration state, but if taken serially, it can also be used to track changes in hydration and indicate fluid needs (i.e., during a bout of physical activity). While various methods of hydration assessment exist, there is no single method that can serve as a criterion measure to assess hydration status in all settings (i.e., day-to-day life and exercise, etc.). Plasma osmolality, changes in plasma volume, and the volume, osmolality and specific gravity of urine are the most commonly published metrics to assess changes in hydration status in clinical settings [26]. The use of these measures in field applications is often impractical, due to the methods or equipment needed to acquire the measure (e.g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
In field applications, the careful assessment of changes in body mass over a bout of physical activity provides a reasonably accurate assessment of body water deficits incurred during the session, since sweat loss and fluid intake during the session underpin the major changes in body mass and body water content. This is true for most sporting activities conducted over a duration of <2–3 h; however, during very prolonged and strenuous exercise (e.g., ultra-endurance races), other factors that cause mass changes, metabolic water production and the liberation of stored water become numerically important and undermine the utility of this assessment [15,27,28]. A comparison of body mass pre- and post-exercise will help guide the athlete in understanding whether their hydration strategy during activity was effective in achieving acceptable fluid balance as well as knowing the volume of fluids that are needed following exercise to return to baseline hydration levels prior to the next exercise session. The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
A useful paradigm for tracking daily changes in hydration status in sporting situations is to consider a combination of assessments to track daily changes. The monitoring of daily changes in body mass, coupled with urine color and thirst sensation status provides adequate sensitivity for most athletic situations [30]. Cheuvront and Kenefick established useful criteria for these variables as body mass changes greater than 1.1%, a conscious desire for water (thirst), and dark-colored urine (>5 a.u. on an 8-a.u. scale [31]) indicating varying degrees of fluid inadequacy [32]. Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Practical Solutions:
(1)
Carefully monitor acute changes in body mass over an exercise bout to determine sweat rate, adequacy of fluid replacement and fluid needs for recovery for that session. Consider how well this can be used to evaluate general hydration strategies in similar situations.
(2)
Use changes in body mass, urine color and thirst upon awakening to track daily changes in hydration status.
3. Exercise Structure
Body fluid loss during sport or exercise largely results from sweating. Net fluid balance is modulated to a certain extent by drinking. Rate of sweating is primarily a function of metabolic heat production [33], but can be modified by environment, clothing, acclimatization and hydration status [7,34]. As the primary mechanism of heat dissipation in many environments, the evaporation of sweat is vital for regulating body temperature, even during exercise in temperate weather. However, this heat dissipation is accompanied by typical fluid losses of ~0.5–1.9 L/h [35].
Exercise intensity is the main factor that determines metabolic heat production, meaning that the rate of fluid losses from sweat for a given exercise session can be partially explained by the intensity of the exercise [36]. Total fluid losses are a result of the sweat rate of a given exercise intensity and the total duration of that activity [27]. In most circumstances there is an inverse relationship between the exercise intensity of a session and the duration of that session. However, given the wide variability in individual sweat rates, the unique interplay between intensity, duration and sweat rate must be considered in unison. For example, a runner with a 2 L/h sweat rate who completes a marathon in 2 h will accumulate the same fluid losses as a runner with a 1 L/h sweat rate that completes the race in 4 h. In and , we define exercise intensity of a range of sporting activities into three distinct categories (High, Moderate, Low), based on typical practice and competition structures on the principles described above but comprehensive plans should consider individual athletes.
Table 1
Team Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Basketball | High | High | Low | Low | Mod | Mod | Low | Low |
| Ice Hockey | High | High | Low | Low | Mod | High | Mod | Mod |
| Football | High | High | Mod | Mod | Mod | High | Mod | Mod |
| Baseball | High | High | Mod | Mod | Low | Low | Low | Low |
| Softball | High | High | Mod | Mod | Low | Low | Low | Low |
| Volleyball | High | High | Low | Low | Low | Low | Low | Low |
| Soccer | Mod | Low | Mod | Mod | Mod | High | Mod | High |
| Lacrosse | High | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Rugby | High | Low | Mod | Mod | Mod | High | Mod | High |
Table 2
Individual Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Tennis | High | Mod | Mod | Mod | High | High | Mod | Mod |
| Wrestling | High | High | Mod | Mod | High | High | High | Low |
| Gymnastics | High | High | Low | Low | Mod | Low | Low | Low |
| Running (<1 h) | Low | High | Mod | Mod | High | High | Low | Low |
| Running (1–2 h) | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Running (>2 h) | Low | High | Mod | Mod | Low | Mod | Mod | Mod |
| Cycling (<1 h) | High | High | Mod | Mod | High | High | Low | Low |
| Cycling (>2 h) | Mod | Mod | Mod | Mod | Mod | Mod | Low | High |
| Swimming | High | High | Low | Low | High | High | Low | Low |
| Triathlon (<2 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (2–5 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (5–9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Triathlon (>9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
For sports like cycling and running, the influence of exercise intensity and duration on fluid needs is very easy to determine given the consistent nature of exercise. demonstrates the relationship between duration and target fluid replacement for steady-state exercise. However, as shown in , some of the most common sports involve supramaximal exercise in short bursts with longer breaks. In this case, individuals should regard an overall average of exercise intensity rather than the maximal effort during the exercise bout when determining optimal fluid balance.
Target fluid replacement estimates to prevent >2 ± 1 % body mass (BM) loss as water (i.e., dehydration). The 70 kg athlete in the example would need to drink a volume of fluid equal to 2.6 ± 0.7 L to prevent >2 ± 1% dehydration when losing 4 L of body water, such as during a marathon (42.1 km). During shorter distances such as 5 or 10 km when fluid losses are unlikely to reach or exceed 2% dehydration, the same athlete would not need to ingest fluids during competition as fluid losses accumulate to <2% dehydration.
It should also be noted that exercise intensity influences gastric emptying rate [37]. Individuals striving to closely match sweat losses with fluid consumption can be challenged by maximal gastric emptying rates. However, when vigorous exercise is conducted (>70% VO2max), gastric emptying decreases predictably, most likely based on decreased splanchnic perfusion [37].
Practical Solutions:
(1)
Increased fluid intake is necessary with prolonged or intense exercise due to increased sweat production.
(2)
During vigorous exercise (>70% VO2max) understand that gastric emptying may limit fluid absorption. Athletes can train their gut to improve gastrointestinal comfort or adopt strategies to increase fluid intake before and after exercise.
4. Environment
At a fixed exercise intensity, the ambient environment further modulates sweat rate. The magnitude of evaporative, radiant, convective and conductive heat exchange between the body and the environment is a function of the gradients between the environment and the skin which provides the main physiological interface for heat exchange. A number of factors contribute to sweat rate including ambient and radiant temperature, humidity, clothing, and air velocity [34], all of which differ depending on the sport or activity ( and ). Therefore, individuals exercising in hot-humid environments with direct sunlight and minimal airflow will produce near maximal sweat rates and be at the greatest risk of hypohydration. Wet-bulb globe thermometry (WBGT) accounts for these environmental factors and can help inform fluid replacement decisions [38].
All clothing provides insulation and presents a barrier to heat loss, resulting in increased sweat rates to provide similar cooling to an unclothed situation [34]. Thus, sports/activities with specific clothing requirements, such as American football [39,40], are at greater risk of body fluid loss compared to similar activities in which clothing is minimal. Synthetic wicking materials can increase sweat fluid losses compared to cotton garments [41], potentially decreasing the thermal load but increasing the risk of dehydration. When the effects of hot, humid environmental conditions are combined with clothing and equipment, individuals can achieve near maximal sweat rates which can create a significant fluid deficit rapidly [40].
Other Environmental Considerations:
Exercising in the cold, or at high altitudes merits special considerations when determining the fluid needs of athletes. Athletes must also be vigilant and mindful of their fluid needs during exercise in the cold. Exercise in the cold can still produce copious sweating, especially when heavy clothing is worn, while also diminishing thirst sensitivity and reducing ad libitum fluid consumption, thus potentially leading to impaired fluid replacement and hypohydration [42]. If possible, athletes should know their individual fluid replacement needs, based upon sweat rate measurement, during exercise in hot and cold environments to ensure they can develop a plan for competing while optimally hydrated.
Athletes unaccustomed to exercising in higher altitudes may require additional fluids. Very high altitude (4900–7600 m) exposure tends to increase water and electrolyte losses, decrease plasma volume and total body water content [43]. In both cold air and high altitudes, respiratory water losses may increase and require additional fluid consumption due to low air water vapor pressures [44]. Therefore, athletes should acclimate to altitude over several days and maintain euhydration prior to competition to ensure optimal athletic performance.
and summarizes typical environmental conditions found among a range of sports into three distinct categories, and how these conditions contribute to the considerations around an individualized fluid plan. Of course, there are large regional differences in environmental conditions experienced for sports at the same time of year [45]. Local measurements utilizing WBGT allow for the greatest characterization of the environmental demands placed on athletes during exercise in the heat [46].
Practical Solutions:
(1)
Measure local environmental conditions to determine the risk of high sweat rates resulting in large fluid losses.
(2)
Increase fluid-replacement during exercise in hot and humid environments to account for increased sweat losses.
(3)
Account for clothing or equipment requirements when evaluating fluid needs.
(4)
Modify fluid intake when exercising in cold or altitude according to an estimation of fluid losses noting that thirst may be less reliable as a guide to dehydration under these conditions.
5. Fluid Availability
Fluid availability refers to the factors that dictate an athlete’s ability to replace fluid losses during activity. In many instances, the characteristics of the sport have a strong influence on the ability to drink during competition and in many scenarios prevent an athlete from “drinking to thirst” [21]. Meanwhile, training activities are often easily modified to allow for some degree of fluid replacement. In many instances, water-breaks during training can be determined on the basis of work-to-rest ratios set by environmental conditions with free access to fluid throughout the break [47]. Characteristics such as flavor and temperature affect the palatability of fluids and may increase voluntary intake when they are matched to the cultural preferences of the athletes and the prevailing conditions (e.g., cool drinks in a warm environment) [48,49].
In endurance sports which provide competitors with feed zones/water stations (e.g., running events), the number of water stations on a course and the frequency with which a competitor reaches them can influence drinking behavior. The International Association of Athletics Federations recommends that stations are placed approximately every 5 km, however, many races include more frequent stations which may influence athletes’ drinking strategies and behaviors [50]. Slower athletes with lower sweat rates who compete in such events, particularly over prolonged distances or duration, are often able to drink in volumes that exceed their true fluid losses and are at particular risk of developing hyponatremia [51]. Athletes taking part in these events should be educated on the importance of fluid balance and the prevention of hyperhydration. It should also be noted that in many events lasting up to 45 min, the risk of dehydration is low due to the limited duration across which sweat losses can accumulate. For faster and/or more competitive athletes, extra elements related to drinking while performing continuous exercise must be taken into consideration. This includes considerations around gastrointestinal comfort when fluid consumed during higher-intensity and “gut joggling” activities (e.g., high-speed running vs. the more “gliding” movements of cross-country skiing or cycling). Furthermore, the time lost in slowing down or moving out of an aerodynamic position to obtain or consume a drink must be factored into the overall race performance. This creates different factors in the cost:benefit analysis of an individual’s fluid intake plan.
The official rules and competition characteristics of “stop-start” sports such as team and racket sports create other influences, and often unique scenarios, around fluid availability. In some examples (e.g., soccer, rugby), governing rules limit the availability of fluids for athletes during competition. Soccer, for example, includes two 45-min halves (with a continuous running clock) in which fluid availability is extremely limited to players. At the other end of the spectrum are sports such as baseball, basketball and tennis with frequent rest breaks within playing time (e.g., time outs, change of ends or player rotations) during which fluids can be consumed. An athlete’s drinking strategy for a competition represents a unique instance for their particular sport based on their ability to rehydrate within the rules [52]. We support recent governing body rule changes and referee decisions to add breaks to competitions (Major League Soccer, FIFA soccer matches, US Open Tennis) to facilitate safe participation by the athletes. These changes likely augment athletic performance and safety simultaneously. Individuals should understand their sport and its fluid needs/fluid availability characteristics to prepare and practice optimal fluid plans for competition. Where rule changes, or alterations are allowed, individuals and teams should attempt to ask for these alterations (e.g., extended rest periods, additional breaks) in advance to formulate an appropriate drinking strategy. In all sports, athletes should aim to practice and fine-tune their personal drinking strategy for race/competition conditions. This will help individuals to confirm its feasibility, understand their personal responses and develop any necessary behavioral practices within the expected rules of competition.
In and , we define fluid availability into three distinct categories, based on particular sport variations. Sports were categorized as having high fluid availability if there are multiple opportunities for fluid consumption, rather than only during breaks. Low fluid availability was used to describe those activities involving governing rules, time constraints, or an inability to carry personal fluids during competition. Accessibility to fluid consumption during competition represents a major variable to be used in preparation of an optimal fluid replacement strategy.
Practical Solutions:
(1)
During training, ensure that there is ample access to fluids that are palatable to athletes.
(2)
Investigate or understand the opportunities for fluid intake during that are specific to a sport or event, and any other practical issues that determine fluid intake.
(3)
Consider the risks of hyperhydration as well as hypohydration for any sporting event or individual athlete, and prepare appropriate practice and education strategies.
(4)
Develop personalized fluid intake plans that incorporate fluid availability characteristics of the sport or event. Where there is a likelihood of hypohydration, be proactive and creative in making use of existing opportunities for fluid intake within sport rules and characteristics and be prepared to request for changes when there is a likelihood of a serious mismatch between fluid losses and the opportunity to address these.
(5)
Practice intended competition drinking plans ahead of time to determine their suitability and allow time for readjustment.
6. Intrinsic Factors
A number of intrinsic factors modulate the individual variances that are observed in fluid losses. One of the greatest considerations for an individual’s sweat rate is his or her body size. Larger individuals typically have higher sweat losses, with football linemen exhibiting some of the highest recorded sweat rates [14]. Therefore, required absolute drink volumes will be higher for these athletes. An individual’s thirst drive also dictates how much they desire to drink during exercise, but this may not match their actual fluid needs. Indeed, multiple authors report that athletes voluntarily dehydrate during exercise due to discrepancies in fluid losses and drinking behavior [53,54]. Case studies of individuals who have developed hyponatremia due to excessive drinking during exercise also note that they reported thirst as an underlying contributor to their fluid intake [55].
Heat acclimatization contributes to variations in an individual’s sweating rate responses. Individuals who are heat acclimatized exhibit greater sweat rates which can pose a greater risk of hypohydration [56]. Although the increased sweat provides extra heat dissipation, it also requires extra fluid intake.
Women may be at greater risk for exercise-induced hyponatremia. This risk has been attributed to their lower body weight and size, excess water ingestion, and longer racing times relative to men [57]. The greater incidence of hyponatremia in women is unlikely due to their greater levels of estradiol in plasma and tissue. Although female sex-hormones can also influence neural and hormonal control of thirst, fluid intake, sodium appetite and sodium regulation [58,59], there is no evidence that anything beyond stature and drinking behavior significantly impact their risk.
Practical Solutions:
7. Sport-Specific Factors
Weight Division, Acrobatic and Appearance-Based Sports
The culture and normal behaviors surrounding specific sports can greatly affect the hydration practices of its athletes. The three most prominent examples of the cultural effects of sports on hydration practices are weight division sports, acrobatic sports and appearance-based sports. In weight division sports (e.g., combat sports, horse racing, lightweight rowing, etc.), the practice of deliberately dehydrating to manipulate body mass to meet lighter competition weight classifications is common [60]. In many cases, athletes not only sacrifice their performance through these practices but also endanger their health and well-being. In a similar fashion, sports where body-image and appearance are emphasized (e.g., cheerleading, body building and gymnastics), dangerous practices, such as extreme fluid restriction may be used by athletes to cheat “unofficial” weight checks that are self-instigated or expected within their training environment. Finally, “acrobatic” feats such as gymnastics, jumping and climbing are aided by a high power to weight ratio, but should not rely on severe hypohydration to achieve this. Excessive use of dehydration to manage body mass goals should be corrected to avoid long-term health complications [61].
Practical Solutions:
8. Conclusions
Based on the factors in the above sections, along with published literature on typical fluid balance observations in various sports [62,63], we assigned risks of hypohydration to the sports in and . These determinations can be used as a general guideline for sports that pose large risks for fluid imbalances that may limit sport performance. The factors for individual situations or geographical locations may vary and should be considered based on the principles mentioned above to tailor the necessary fluid replacement accommodations. An example of using this paradigm to develop a hydration plan can be found in .
Table 3
Establishing a Hydration Plan.
| Guiding Question | Steps to Correct | Implementation Example |
|---|---|---|
| Are athletes in a state of optimal hydration? | ||
| Is the exercise prolonged or intense? | ||
| Is the exercise being performed in environmental conditions that lead to greater fluid losses? | ||
| Is fluid available throughout the entire duration of exercise? |
| |
| Are there individuals with intrinsic risk factors? |
| |
| Are there sport-specific factors that need to be considered? |
In this paper we present a paradigm that can be used by clinicians and practitioners to develop hydration strategies for sports based on fluid availability, environment and exercise intensity. These tools are provided to inform hydration education and practices in a dynamic and individualized manner so that athletes can adapt to different circumstances and optimize performance.
Author Contributions
All authors attended the meeting and contributed to drafting and revision of the manuscript. All authors approved the final version of the paper.
Funding
The meeting preceding this manuscript was funded by PepsiCo (Gatorade).
Conflicts of Interest
Douglas Casa is the Chief Executive Officer of the Korey Stringer Institute, a 503.c not for profit which subsists on the donations from our corporate partners who include Gatorade, CamelBak, NFL, NATA, Mission, Eagle Pharmaceuticals and Kestrel. He has also been a recipient of grant funds from the following entities to study hydration related products: GE Healthcare, Halo Wearables, Nix Inc., CamelBak. William Adams has consulted with the following entities regarding hydration and exercise performance or the development of hydration assessment devices: BSX Athletics; Samsung Oak Holdings, Inc; Nobo, Inc; Clif Bar &Company; The Gatorade Company, Inc. Lawrence Armstrong is a hydration consultant to Danone Nutricia Research, France and the Drinking Water Research Foundation, Alexandria VA, USA. Lindsay Baker is employed by the Gatorade Sports Science Institute, a division of PepsiCo, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc. Louise Burke was a member of the Gatorade Sports Science Institute’s Expert Panel from 2014–2015 for which her workplace received an honorarium. Jose Gonzalez-Alonso was a member of the Gatorade Sports Science Institute’s Expert Panel in 2017 for which his workplace received an honorarium. Stavros Kavouras has served as scientific consultant for Quest Diagnostics, Standard Process and Danone Research and has active grants with Danone Research. The funders had no role in the in the writing of the manuscript.
References
1. Sawka M., Pandolf K.B. Effects of body water loss on physiological function and exercise performance. In: Gisolfi C., Lamb D.R., editors. Perspectives in Exercise Science and Sports Medicine. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 1–38. [Google Scholar]2. Sawka M.N., Wenger C.B., Pandolf K.B. Thermoregulatory Responses to Acute Exercise-Heat Stress and Heat Acclimation. In: Terjung R., editor. Comprehensive Physiology. John Wiley & Sons; Hoboken, NJ, USA: 2011. pp. 97–151. [Google Scholar]3. Montain S.J., Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [PubMed] [CrossRef] [Google Scholar]4. Montain S.J., Sawka M.N., Latzka W.A., Valeri C.R. Thermal and cardiovascular strain from hypohydration: Influence of exercise intensity. Int. J. Sports Med. 1998;19:87–91. doi: 10.1055/s-2007-971887. [PubMed] [CrossRef] [Google Scholar]5. Sawka M.N., Young A.J., Francesconi R.P., Muza S.R., Pandolf K.B. Thermoregulatory and blood responses during exercise at graded hypohydration levels. J. Appl. Physiol. 1985;59:1394–1401. doi: 10.1152/jappl.1985.59.5.1394. [PubMed] [CrossRef] [Google Scholar]6. Adams W.M., Ferraro E.M., Huggins R.A., Casa D.J. Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 2014;28:2380–2389. doi: 10.1519/JSC.0000000000000501. [PubMed] [CrossRef] [Google Scholar]7. Kenefick R.W., Cheuvront S.N. Physiological adjustments to hypohydration: Impact on thermoregulation. Auton. Neurosci. 2016;196:47–51. doi: 10.1016/j.autneu.2016.02.003. [PubMed] [CrossRef] [Google Scholar]8. Trangmar S.J., Gonzalez-Alonso J. New Insights into the Impact of Dehydration on Blood Flow and Metabolism during Exercise. Exerc. Sport Sci. Rev. 2017;45:146–153. doi: 10.1249/JES.0000000000000109. [PubMed] [CrossRef] [Google Scholar]9. Gonzalez-Alonso J., Crandall C.G., Johnson J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008;586:45–53. doi: 10.1113/jphysiol.2007.142158. [PMC free article] [PubMed] [CrossRef] [Google Scholar]10. Trangmar S.J., Gonzalez-Alonso J. Heat, Hydration and the Human Brain, Heart and Skeletal Muscles. Sports Med. 2019;49:69–85. doi: 10.1007/s40279-018-1033-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]11. Cheuvront S.N., Carter R., 3rd, Sawka M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003;2:202–208. doi: 10.1249/00149619-200308000-00006. [PubMed] [CrossRef] [Google Scholar]12. Cheuvront S.N., Kenefick R.W., Montain S.J., Sawka M.N. Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 2010;109:1989–1995. doi: 10.1152/japplphysiol.00367.2010. [PubMed] [CrossRef] [Google Scholar]13. Barr S.I. Effects of dehydration on exercise performance. Can. J. Appl. Physiol. 1999;24:164–172. doi: 10.1139/h99-014. [PubMed] [CrossRef] [Google Scholar]14. Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007;39:377–390. [PubMed] [Google Scholar]15. McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O′Connor F.G., Roberts W.O. National Athletic Trainers′ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [PMC free article] [PubMed] [CrossRef] [Google Scholar]16. Judelson D.A., Maresh C.M., Anderson J.M., Armstrong L.E., Casa D.J., Kraemer W.J., Volek J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007;37:907–921. doi: 10.2165/00007256-200737100-00006. [PubMed] [CrossRef] [Google Scholar]17. Coyle E.F. Physiological determinants of endurance exercise performance. J. Sci. Med. Sport. 1999;2:181–189. doi: 10.1016/S1440-2440(99)80172-8. [PubMed] [CrossRef] [Google Scholar]18. Adams J.D., Sekiguchi Y., Suh H.G., Seal A.D., Sprong C.A., Kirkland T.W., Kavouras S.A. Dehydration Impairs Cycling Performance, Independently of Thirst: A Blinded Study. Med. Sci. Sports Exerc. 2018;50:1697–1703. doi: 10.1249/MSS.0000000000001597. [PubMed] [CrossRef] [Google Scholar]20. Bergeron M.F., Bahr R., Bartsch P., Bourdon L., Calbet J.A.L., Carlsen K.H., Castagna O., González-Alonso J., Lundby C., Maughan R.J., et al. International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br. J. Sports Med. 2012;46:770–779. doi: 10.1136/bjsports-2012-091296. [PubMed] [CrossRef] [Google Scholar]21. Racinais S., Alonso J.M., Coutts A.J., Flouris A.D., Girard O., Gonzalez-Alonso J., Hausswirth C., Jay O., Lee J.K., Mitchell N., et al. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015;49:1164–1173. doi: 10.1136/bjsports-2015-094915. [PMC free article] [PubMed] [CrossRef] [Google Scholar]22. Carter J.E., Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med. Sci. Sports Exerc. 1989;21:532–539. doi: 10.1249/00005768-198910000-00007. [PubMed] [CrossRef] [Google Scholar]23. Coyle E.F., Hamilton M. Fluid replacement during exercise: Effects on physiological homeostasis and performance. In: Gisolfi C., Lamb D.R., editors. Fluid Homeostasis During Exercise. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 281–308. [Google Scholar]24. Mora-Rodriguez R., Hamouti N., Del Coso J., Ortega J.F. Fluid ingestion is more effective in preventing hyperthermia in aerobically trained than untrained individuals during exercise in the heat. Appl. Physiol. Nutr. Metab. 2013;38:73–80. doi: 10.1139/apnm-2012-0174. [PubMed] [CrossRef] [Google Scholar]25. Wittels P., Gunga H.C., Kirsch K., Kanduth B., Gunther T., Vormann J., Rocker L. Fluid regulation during prolonged physical strain with water and food deprivation in healthy, trained men. Wien. Klin. Wochenschr. 1996;108:788–794. [PubMed] [Google Scholar]26. Armstrong L.E. Hydration assessment techniques. Nutr. Rev. 2005;63:S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [PubMed] [CrossRef] [Google Scholar]27. Cheuvront S.N., Kenefick R.W. CORP: Improving the status quo for measuring whole body sweat losses. J. Appl. Physiol. 2017;123:632–636. doi: 10.1152/japplphysiol.00433.2017. [PubMed] [CrossRef] [Google Scholar]28. Baker L.B., Lang J.A., Kenney W.L. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur. J. Appl. Physiol. 2009;105:959–967. doi: 10.1007/s00421-009-0982-0. [PubMed] [CrossRef] [Google Scholar]29. Armstrong L.E., Casa D.J. Methods to Evaluate Electrolyte and Water Turnover of Athletes. Athl. Train. Sports Health Care. 2009;1:1–11. doi: 10.3928/19425864-20090625-06. [CrossRef] [Google Scholar]30. Cheuvront S.N., Kenefick R.W. Am I Drinking Enough? Yes, No, and Maybe. J. Am. Coll. Nutr. 2016;35:185–192. doi: 10.1080/07315724.2015.1067872. [PubMed] [CrossRef] [Google Scholar]31. Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M.F., Kenefick R.W., LaGasse K.E., Riebe D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [PubMed] [CrossRef] [Google Scholar]32. Cheuvront S.N., Sawka M.N. Hydration Assessment of Athletes. Sports Sci. Exch. 2005;18:1–5. [Google Scholar]33. Stolwijk J.A., Saltin B., Gagge A.P. Physiological factors associated with sweating during exercise. Aerosp. Med. 1968;39:1101–1105. [PubMed] [Google Scholar]34. Parsons K. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance. 3rd ed. CRC Press; Boca Raton, FL, USA: 2014. [Google Scholar]35. Baker L.B., Barnes K.A., Anderson M.L., Passe D.H., Stofan J.R. Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 2016;34:358–368. doi: 10.1080/02640414.2015.1055291. [PubMed] [CrossRef] [Google Scholar]36. Nadel E.R. Control of sweating rate while exercising in the heat. Med. Sci. Sports. 1979;11:31–35. [PubMed] [Google Scholar]37. Horner K.M., Schubert M.M., Desbrow B., Byrne N.M., King N.A. Acute exercise and gastric emptying: A meta-analysis and implications for appetite control. Sports Med. 2015;45:659–678. doi: 10.1007/s40279-014-0285-4. [PubMed] [CrossRef] [Google Scholar]38. Budd G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [PubMed] [CrossRef] [Google Scholar]39. Kulka T.J., Kenney W.L. Heat balance limits in football uniforms how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30:29–39. doi: 10.3810/psm.2002.07.377. [PubMed] [CrossRef] [Google Scholar]40. Armstrong L.E., Johnson E.C., Casa D.J., Ganio M.S., McDermott B.P., Yamamoto L.M., Lopez R.M., Emmanuel H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010;45:117–127. doi: 10.4085/1062-6050-45.2.117. [PMC free article] [PubMed] [CrossRef] [Google Scholar]41. Hooper D.R., Cook B.M., Comstock B.A., Szivak T.K., Flanagan S.D., Looney D.P., DuPont W.H., Kraemer W.J. Synthetic garments enhance comfort, thermoregulatory response, and athletic performance compared with traditional cotton garments. J. Strength Cond. Res. 2015;29:700–707. doi: 10.1519/JSC.0000000000000783. [PubMed] [CrossRef] [Google Scholar]42. O′Brien C., Freund B.J., Sawka M.N., McKay J., Hesslink R.L., Jones T.E. Hydration assessment during cold-weather military field training exercises. Arct. Med. Res. 1996;55:20–26. [PubMed] [Google Scholar]43. Fusch C., Gfrorer W., Koch C., Thomas A., Grunert A., Moeller H. Water turnover and body composition during long-term exposure to high altitude (4900–7600 m) J. Appl. Physiol. 1996;80:1118–1125. doi: 10.1152/jappl.1996.80.4.1118. [PubMed] [CrossRef] [Google Scholar]44. Mitchell J.W., Nadel E.R., Stolwijk J.A. Respiratory weight losses during exercise. J. Appl. Physiol. 1972;32:474–476. doi: 10.1152/jappl.1972.32.4.474. [PubMed] [CrossRef] [Google Scholar]45. Grundstein A., Williams C., Phan M., Cooper E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015;56:55–60. doi: 10.1016/j.apgeog.2014.10.014. [CrossRef] [Google Scholar]46. Cheuvront S.N., Caruso E.M., Heavens K.R., Karis A.J., Santee W.R., Troyanos C., D′Hemecourt P. Effect of WBGT Index Measurement Location on Heat Stress Category Classification. Med. Sci. Sports Exerc. 2015;47:1958–1964. doi: 10.1249/MSS.0000000000000624. [PubMed] [CrossRef] [Google Scholar]47. Casa D.J., DeMartini J.K., Bergeron M.F., Csillan D., Eichner E.R., Lopez R.M., Ferrara M.S., Miller K.C., O′Connor F., Sawka M.N., et al. National Athletic Trainers′ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]48. Minehan M.R., Riley M.D., Burke L.M. Effect of flavor and awareness of kilojoule content of drinks on preference and fluid balance in team sports. Int. J. Sport Nutr. Exerc. Metab. 2002;12:81–92. doi: 10.1123/ijsnem.12.1.81. [PubMed] [CrossRef] [Google Scholar]49. Burdon C.A., Johnson N.A., Chapman P.G., O′Connor H.T. Influence of beverage temperature on palatability and fluid ingestion during endurance exercise: A systematic review. Int. J. Sport Nutr. Exerc. Metab. 2012;22:199–211. doi: 10.1123/ijsnem.22.3.199. [PubMed] [CrossRef] [Google Scholar]50. Williams J., Tzortziou Brown V., Malliaras P., Perry M., Kipps C. Hydration strategies of runners in the London Marathon. Clin. J. Sport Med. 2012;22:152–156. doi: 10.1097/JSM.0b013e3182364c45. [PubMed] [CrossRef] [Google Scholar]51. Chorley J., Cianca J., Divine J. Risk factors for exercise-associated hyponatremia in non-elite marathon runners. Clin. J. Sport Med. 2007;17:471–477. doi: 10.1097/JSM.0b013e3181588790. [PubMed] [CrossRef] [Google Scholar]52. Maughan R.J., Shirreffs S.M. Development of individual hydration strategies for athletes. Int. J. Sport Nutr. Exerc. Metab. 2008;18:457–472. doi: 10.1123/ijsnem.18.5.457. [PubMed] [CrossRef] [Google Scholar]53. Passe D., Horn M., Stofan J., Horswill C., Murray R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007;17:284–295. doi: 10.1123/ijsnem.17.3.284. [PubMed] [CrossRef] [Google Scholar]54. Hosseinlou A., Khamnei S., Zamanlu M. The effect of water temperature and voluntary drinking on the post rehydration sweating. Int. J. Clin. Exp. Med. 2013;6:683–687. [PMC free article] [PubMed] [Google Scholar]55. Hew-Butler T., Rosner M.H., Fowkes-Godek S., Dugas J.P., Hoffman M.D., Lewis D.P., Maughan R.J., Miller K.C., Montain S.J., Rehrer N.J., et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [PubMed] [CrossRef] [Google Scholar]56. Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis. Sports Med. 2016;46:1699–1724. doi: 10.1007/s40279-016-0538-5. [PubMed] [CrossRef] [Google Scholar]57. Almond C.S., Shin A.Y., Fortescue E.B., Mannix R.C., Wypij D., Binstadt B.A., Duncan C.N., Olson D.P., Salerno A.E., Newburger J.W. Hyponatremia among runners in the Boston Marathon. N. Engl. J. Med. 2005;352:1550–1556. doi: 10.1056/NEJMoa043901. [PubMed] [CrossRef] [Google Scholar]58. Ishunina T.A., Swaab D.F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus; size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 1999;84:4637–4644. doi: 10.1210/jcem.84.12.6187. [PubMed] [CrossRef] [Google Scholar]59. Sar M., Stumpf W. Simultaneous localization of [3 H] estradiol and neurophysin I or arginine vasopressin in hypothalamic neurons demonstrated by a combined technique of dry-mount autoradiography and immunohistochemistry. Neurosci. Lett. 1980;17:179–184. doi: 10.1016/0304-3940(80)90081-6. [PubMed] [CrossRef] [Google Scholar]60. Barley O.R., Chapman D.W., Abbiss C.R. Weight Loss Strategies in Combat Sports and Concerning Habits in Mixed Martial Arts. Int. J. Sports Physiol. Perform. 2018;13:933–939. doi: 10.1123/ijspp.2017-0715. [PubMed] [CrossRef] [Google Scholar]61. Bonci C.M., Bonci L.J., Granger L.R., Johnson C.L., Malina R.M., Milne L.W., Ryan R.R., Vanderbunt E.M. National athletic trainers′ association position statement: Preventing, detecting, and managing disordered eating in athletes. J. Athl Train. 2008;43:80–108. doi: 10.4085/1062-6050-43.1.80. [PMC free article] [PubMed] [CrossRef] [Google Scholar]62. Nuccio R.P., Barnes K.A., Carter J.M., Baker L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017;47:1951–1982. doi: 10.1007/s40279-017-0738-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]63. Garth A.K., Burke L.M. What do athletes drink during competitive sporting activities? Sports Med. 2013;43:539–564. doi: 10.1007/s40279-013-0028-y. [PubMed] [CrossRef] [Google Scholar]
Practical Hydration Solutions for Sports
Nutrients. 2019 Jul; 11(7): 1550.
,1,*,2,1,3,4,5,6,7,8,9,1,10,4,11,12,13,14,1,15 and 16
Luke N. Belval
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Yuri Hosokawa
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
Douglas J. Casa
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
William M. Adams
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
Lawrence E. Armstrong
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Lindsay B. Baker
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
Louise Burke
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
Samuel Cheuvront
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
George Chiampas
8U.S. Soccer, Chicago, IL 60616, USA
José González-Alonso
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
Robert A. Huggins
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Stavros A. Kavouras
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
Elaine C. Lee
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Brendon P. McDermott
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
Kevin Miller
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
Zachary Schlader
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
Stacy Sims
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
Rebecca L. Stearns
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
Chris Troyanos
15International Institute of Race Medicine, Plymouth, MA 02360, USA
Jonathan Wingo
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
1Korey Stringer Institute, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
2Faculty of Sport Sciences, Waseda University, Saitama 359-1192, Japan
3Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC 27402, USA
4Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA
5Gatorade Sports Science Institute, Barrington, IL 60010, USA
6Sports Nutrition, Australian Institute of Sport, Canberra, ACT 2617, Australia
7Sports Science Synergy, LLC, Franklin, MA 02038, USA
8U.S. Soccer, Chicago, IL 60616, USA
9Centre for Human Performance, Exercise and Rehabilitation, Brunel University London, Uxbridge UB8 3PH, UK
10Hydration Science Lab, College of Health Solutions, Arizona State University, Phoenix, AZ 85004, USA
11Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, AR 72701, USA
12Department of Rehabilitation and Medical Sciences, Central Michigan University, Mount Pleasant, MI 48859, USA
13Department of Exercise and Nutrition Sciences, University at Buffalo, Buffalo, NY 14214, USA
14Faculty of Health, Sport and Human Performance, University of Waikato, Hamilton 3216, New Zealand
15International Institute of Race Medicine, Plymouth, MA 02360, USA
16Department of Kinesiology, University of Alabama, Tuscaloosa, AL 35487, USA
Received 2019 May 15; Accepted 2019 Jul 3.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).This article has been cited by other articles in PMC.
Abstract
Personalized hydration strategies play a key role in optimizing the performance and safety of athletes during sporting activities. Clinicians should be aware of the many physiological, behavioral, logistical and psychological issues that determine both the athlete’s fluid needs during sport and his/her opportunity to address them; these are often specific to the environment, the event and the individual athlete. In this paper we address the major considerations for assessing hydration status in athletes and practical solutions to overcome obstacles of a given sport. Based on these solutions, practitioners can better advise athletes to develop practices that optimize hydration for their sports.
Keywords: fluid replacement, athletics, exercise
1. Introduction
Maintaining euhydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water contributes 50–70% of total body mass and is compartmentalized within both intracellular (65%) and extracellular (35%) spaces [1]. Euhydration is typically maintained over the course of day-to-day life via behavioral and biological controls [2]. However, exercise can cause an acute disruption to fluid balance, challenging the athlete’s goal of optimal performance and safety during exercise, especially in hot environmental conditions. The process of incurring a fluid deficit is known as dehydration, while the outcome is defined as hypohydration. The loss of body water during exercise exacerbates physiological and perceptual strain [3,4,5,6,7,8,9,10] and it is well established that these changes can impair endurance performance, particularly in hot environments and may increase the risk of exertional heat illness [11,12,13,14,15,16,17].
While the sensation of thirst, a centrally mediated response to body water deficits, is useful in dictating the need for fluid intake during daily life, thirst is relatively insensitive in acutely tracking hydration status during exercise [18,19]. Maintaining an optimal state of hydration during exercise becomes more complicated depending on the sport, type of activity and availability of fluid. Optimal hydration is dependent on many factors but can generally be defined during exercise as avoiding losses greater than 2–3% of body mass while also avoiding overhydration [15]. Furthermore, during exercise, it is not uncommon for individuals to involuntarily dehydrate, in which they consume less fluid than their fluid needs. Excessive fluid intake can also be problematic, with hyponatremia developing in severe cases of overhydration [15]. Inappropriate management of fluid intake resulting in hypohydration, or hyperhydration, can be detrimental for performance and in some circumstances, increases health risk.
Current consensus recommends that good hydration practices include: (1) beginning exercise in a state of euhydration, (2) preventing excessive hypohydration during exercise, and (3) replacing remaining losses following exercise prior to the next exercise bout [15,20,21]. These practices attenuate the adverse effects of acute dehydration on physical activity and health [15]. However, it is acknowledged that fluid needs are individualistic and rely on factors such as personal sweat rate, exercise mode, exercise intensity, environmental conditions and exercise duration () [14,15,22,23,24,25]. Furthermore, characteristics and rules unique to each sport environment in which it is played, event uniform and equipment, and the availability of fluid during both training and competition may greatly influence the ability to optimize hydration during activity. The Korey Stringer Institute and Gatorade convened a meeting to address these issues as they relate to athletes. The purpose of these proceedings is to discuss practical strategies to assess and tailor hydration for sports. This manuscript will specifically focus on the factors that underlie fluid needs and provide guidance to clinicians and practitioners on how to plan for these needs in the context of a given activity.
Factors that contribute to the risk of hypohydration or hyperhydration during exercise.
2. Hydration Assessment
Hydration assessment can be utilized to indicate one’s current hydration state, but if taken serially, it can also be used to track changes in hydration and indicate fluid needs (i.e., during a bout of physical activity). While various methods of hydration assessment exist, there is no single method that can serve as a criterion measure to assess hydration status in all settings (i.e., day-to-day life and exercise, etc.). Plasma osmolality, changes in plasma volume, and the volume, osmolality and specific gravity of urine are the most commonly published metrics to assess changes in hydration status in clinical settings [26]. The use of these measures in field applications is often impractical, due to the methods or equipment needed to acquire the measure (e.g., a needle stick to draw blood or providing a urine sample) as well as the sensitivity of the measure.
In field applications, the careful assessment of changes in body mass over a bout of physical activity provides a reasonably accurate assessment of body water deficits incurred during the session, since sweat loss and fluid intake during the session underpin the major changes in body mass and body water content. This is true for most sporting activities conducted over a duration of <2–3 h; however, during very prolonged and strenuous exercise (e.g., ultra-endurance races), other factors that cause mass changes, metabolic water production and the liberation of stored water become numerically important and undermine the utility of this assessment [15,27,28]. A comparison of body mass pre- and post-exercise will help guide the athlete in understanding whether their hydration strategy during activity was effective in achieving acceptable fluid balance as well as knowing the volume of fluids that are needed following exercise to return to baseline hydration levels prior to the next exercise session. The methodology for assessing sweat losses is to assess the athlete’s body mass before and after exercise with care to avoid or account for substantial amounts of fluid trapped in hair and clothes. Accounting for any fluid consumed or urine excreted, the difference between the masses can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in post-exercise recovery plans [29].
A useful paradigm for tracking daily changes in hydration status in sporting situations is to consider a combination of assessments to track daily changes. The monitoring of daily changes in body mass, coupled with urine color and thirst sensation status provides adequate sensitivity for most athletic situations [30]. Cheuvront and Kenefick established useful criteria for these variables as body mass changes greater than 1.1%, a conscious desire for water (thirst), and dark-colored urine (>5 a.u. on an 8-a.u. scale [31]) indicating varying degrees of fluid inadequacy [32]. Two of these factors combined suggest daily fluid intake is likely inadequate, while all three factors indicate that daily fluid intake is very likely inadequate. It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Practical Solutions:
(1)
Carefully monitor acute changes in body mass over an exercise bout to determine sweat rate, adequacy of fluid replacement and fluid needs for recovery for that session. Consider how well this can be used to evaluate general hydration strategies in similar situations.
(2)
Use changes in body mass, urine color and thirst upon awakening to track daily changes in hydration status.
3. Exercise Structure
Body fluid loss during sport or exercise largely results from sweating. Net fluid balance is modulated to a certain extent by drinking. Rate of sweating is primarily a function of metabolic heat production [33], but can be modified by environment, clothing, acclimatization and hydration status [7,34]. As the primary mechanism of heat dissipation in many environments, the evaporation of sweat is vital for regulating body temperature, even during exercise in temperate weather. However, this heat dissipation is accompanied by typical fluid losses of ~0.5–1.9 L/h [35].
Exercise intensity is the main factor that determines metabolic heat production, meaning that the rate of fluid losses from sweat for a given exercise session can be partially explained by the intensity of the exercise [36]. Total fluid losses are a result of the sweat rate of a given exercise intensity and the total duration of that activity [27]. In most circumstances there is an inverse relationship between the exercise intensity of a session and the duration of that session. However, given the wide variability in individual sweat rates, the unique interplay between intensity, duration and sweat rate must be considered in unison. For example, a runner with a 2 L/h sweat rate who completes a marathon in 2 h will accumulate the same fluid losses as a runner with a 1 L/h sweat rate that completes the race in 4 h. In and , we define exercise intensity of a range of sporting activities into three distinct categories (High, Moderate, Low), based on typical practice and competition structures on the principles described above but comprehensive plans should consider individual athletes.
Table 1
Team Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Basketball | High | High | Low | Low | Mod | Mod | Low | Low |
| Ice Hockey | High | High | Low | Low | Mod | High | Mod | Mod |
| Football | High | High | Mod | Mod | Mod | High | Mod | Mod |
| Baseball | High | High | Mod | Mod | Low | Low | Low | Low |
| Softball | High | High | Mod | Mod | Low | Low | Low | Low |
| Volleyball | High | High | Low | Low | Low | Low | Low | Low |
| Soccer | Mod | Low | Mod | Mod | Mod | High | Mod | High |
| Lacrosse | High | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Rugby | High | Low | Mod | Mod | Mod | High | Mod | High |
Table 2
Individual Sport Factors That Influence Hypohydration.
| Sport | Availability of Fluid | Environment | Intensity | Hypohydration Risk | ||||
|---|---|---|---|---|---|---|---|---|
| Training | Competition | Training | Competition | Training | Competition | Training | Competition | |
| Tennis | High | Mod | Mod | Mod | High | High | Mod | Mod |
| Wrestling | High | High | Mod | Mod | High | High | High | Low |
| Gymnastics | High | High | Low | Low | Mod | Low | Low | Low |
| Running (<1 h) | Low | High | Mod | Mod | High | High | Low | Low |
| Running (1–2 h) | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Running (>2 h) | Low | High | Mod | Mod | Low | Mod | Mod | Mod |
| Cycling (<1 h) | High | High | Mod | Mod | High | High | Low | Low |
| Cycling (>2 h) | Mod | Mod | Mod | Mod | Mod | Mod | Low | High |
| Swimming | High | High | Low | Low | High | High | Low | Low |
| Triathlon (<2 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (2–5 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Low | Low |
| Run | Low | High | Mod | Mod | Mod | Mod | Low | Low |
| Triathlon (5–9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Triathlon (>9 h) | ||||||||
| Swim | Low | Low | Low | Low | Mod | Mod | Low | Low |
| Bike | Mod | High | Mod | Mod | Mod | Mod | Mod | Mod |
| Run | Low | High | Mod | Mod | Mod | Mod | Mod | Mod |
For sports like cycling and running, the influence of exercise intensity and duration on fluid needs is very easy to determine given the consistent nature of exercise. demonstrates the relationship between duration and target fluid replacement for steady-state exercise. However, as shown in , some of the most common sports involve supramaximal exercise in short bursts with longer breaks. In this case, individuals should regard an overall average of exercise intensity rather than the maximal effort during the exercise bout when determining optimal fluid balance.
Target fluid replacement estimates to prevent >2 ± 1 % body mass (BM) loss as water (i.e., dehydration). The 70 kg athlete in the example would need to drink a volume of fluid equal to 2.6 ± 0.7 L to prevent >2 ± 1% dehydration when losing 4 L of body water, such as during a marathon (42.1 km). During shorter distances such as 5 or 10 km when fluid losses are unlikely to reach or exceed 2% dehydration, the same athlete would not need to ingest fluids during competition as fluid losses accumulate to <2% dehydration.
It should also be noted that exercise intensity influences gastric emptying rate [37]. Individuals striving to closely match sweat losses with fluid consumption can be challenged by maximal gastric emptying rates. However, when vigorous exercise is conducted (>70% VO2max), gastric emptying decreases predictably, most likely based on decreased splanchnic perfusion [37].
Practical Solutions:
(1)
Increased fluid intake is necessary with prolonged or intense exercise due to increased sweat production.
(2)
During vigorous exercise (>70% VO2max) understand that gastric emptying may limit fluid absorption. Athletes can train their gut to improve gastrointestinal comfort or adopt strategies to increase fluid intake before and after exercise.
4. Environment
At a fixed exercise intensity, the ambient environment further modulates sweat rate. The magnitude of evaporative, radiant, convective and conductive heat exchange between the body and the environment is a function of the gradients between the environment and the skin which provides the main physiological interface for heat exchange. A number of factors contribute to sweat rate including ambient and radiant temperature, humidity, clothing, and air velocity [34], all of which differ depending on the sport or activity ( and ). Therefore, individuals exercising in hot-humid environments with direct sunlight and minimal airflow will produce near maximal sweat rates and be at the greatest risk of hypohydration. Wet-bulb globe thermometry (WBGT) accounts for these environmental factors and can help inform fluid replacement decisions [38].
All clothing provides insulation and presents a barrier to heat loss, resulting in increased sweat rates to provide similar cooling to an unclothed situation [34]. Thus, sports/activities with specific clothing requirements, such as American football [39,40], are at greater risk of body fluid loss compared to similar activities in which clothing is minimal. Synthetic wicking materials can increase sweat fluid losses compared to cotton garments [41], potentially decreasing the thermal load but increasing the risk of dehydration. When the effects of hot, humid environmental conditions are combined with clothing and equipment, individuals can achieve near maximal sweat rates which can create a significant fluid deficit rapidly [40].
Other Environmental Considerations:
Exercising in the cold, or at high altitudes merits special considerations when determining the fluid needs of athletes. Athletes must also be vigilant and mindful of their fluid needs during exercise in the cold. Exercise in the cold can still produce copious sweating, especially when heavy clothing is worn, while also diminishing thirst sensitivity and reducing ad libitum fluid consumption, thus potentially leading to impaired fluid replacement and hypohydration [42]. If possible, athletes should know their individual fluid replacement needs, based upon sweat rate measurement, during exercise in hot and cold environments to ensure they can develop a plan for competing while optimally hydrated.
Athletes unaccustomed to exercising in higher altitudes may require additional fluids. Very high altitude (4900–7600 m) exposure tends to increase water and electrolyte losses, decrease plasma volume and total body water content [43]. In both cold air and high altitudes, respiratory water losses may increase and require additional fluid consumption due to low air water vapor pressures [44]. Therefore, athletes should acclimate to altitude over several days and maintain euhydration prior to competition to ensure optimal athletic performance.
and summarizes typical environmental conditions found among a range of sports into three distinct categories, and how these conditions contribute to the considerations around an individualized fluid plan. Of course, there are large regional differences in environmental conditions experienced for sports at the same time of year [45]. Local measurements utilizing WBGT allow for the greatest characterization of the environmental demands placed on athletes during exercise in the heat [46].
Practical Solutions:
(1)
Measure local environmental conditions to determine the risk of high sweat rates resulting in large fluid losses.
(2)
Increase fluid-replacement during exercise in hot and humid environments to account for increased sweat losses.
(3)
Account for clothing or equipment requirements when evaluating fluid needs.
(4)
Modify fluid intake when exercising in cold or altitude according to an estimation of fluid losses noting that thirst may be less reliable as a guide to dehydration under these conditions.
5. Fluid Availability
Fluid availability refers to the factors that dictate an athlete’s ability to replace fluid losses during activity. In many instances, the characteristics of the sport have a strong influence on the ability to drink during competition and in many scenarios prevent an athlete from “drinking to thirst” [21]. Meanwhile, training activities are often easily modified to allow for some degree of fluid replacement. In many instances, water-breaks during training can be determined on the basis of work-to-rest ratios set by environmental conditions with free access to fluid throughout the break [47]. Characteristics such as flavor and temperature affect the palatability of fluids and may increase voluntary intake when they are matched to the cultural preferences of the athletes and the prevailing conditions (e.g., cool drinks in a warm environment) [48,49].
In endurance sports which provide competitors with feed zones/water stations (e.g., running events), the number of water stations on a course and the frequency with which a competitor reaches them can influence drinking behavior. The International Association of Athletics Federations recommends that stations are placed approximately every 5 km, however, many races include more frequent stations which may influence athletes’ drinking strategies and behaviors [50]. Slower athletes with lower sweat rates who compete in such events, particularly over prolonged distances or duration, are often able to drink in volumes that exceed their true fluid losses and are at particular risk of developing hyponatremia [51]. Athletes taking part in these events should be educated on the importance of fluid balance and the prevention of hyperhydration. It should also be noted that in many events lasting up to 45 min, the risk of dehydration is low due to the limited duration across which sweat losses can accumulate. For faster and/or more competitive athletes, extra elements related to drinking while performing continuous exercise must be taken into consideration. This includes considerations around gastrointestinal comfort when fluid consumed during higher-intensity and “gut joggling” activities (e.g., high-speed running vs. the more “gliding” movements of cross-country skiing or cycling). Furthermore, the time lost in slowing down or moving out of an aerodynamic position to obtain or consume a drink must be factored into the overall race performance. This creates different factors in the cost:benefit analysis of an individual’s fluid intake plan.
The official rules and competition characteristics of “stop-start” sports such as team and racket sports create other influences, and often unique scenarios, around fluid availability. In some examples (e.g., soccer, rugby), governing rules limit the availability of fluids for athletes during competition. Soccer, for example, includes two 45-min halves (with a continuous running clock) in which fluid availability is extremely limited to players. At the other end of the spectrum are sports such as baseball, basketball and tennis with frequent rest breaks within playing time (e.g., time outs, change of ends or player rotations) during which fluids can be consumed. An athlete’s drinking strategy for a competition represents a unique instance for their particular sport based on their ability to rehydrate within the rules [52]. We support recent governing body rule changes and referee decisions to add breaks to competitions (Major League Soccer, FIFA soccer matches, US Open Tennis) to facilitate safe participation by the athletes. These changes likely augment athletic performance and safety simultaneously. Individuals should understand their sport and its fluid needs/fluid availability characteristics to prepare and practice optimal fluid plans for competition. Where rule changes, or alterations are allowed, individuals and teams should attempt to ask for these alterations (e.g., extended rest periods, additional breaks) in advance to formulate an appropriate drinking strategy. In all sports, athletes should aim to practice and fine-tune their personal drinking strategy for race/competition conditions. This will help individuals to confirm its feasibility, understand their personal responses and develop any necessary behavioral practices within the expected rules of competition.
In and , we define fluid availability into three distinct categories, based on particular sport variations. Sports were categorized as having high fluid availability if there are multiple opportunities for fluid consumption, rather than only during breaks. Low fluid availability was used to describe those activities involving governing rules, time constraints, or an inability to carry personal fluids during competition. Accessibility to fluid consumption during competition represents a major variable to be used in preparation of an optimal fluid replacement strategy.
Practical Solutions:
(1)
During training, ensure that there is ample access to fluids that are palatable to athletes.
(2)
Investigate or understand the opportunities for fluid intake during that are specific to a sport or event, and any other practical issues that determine fluid intake.
(3)
Consider the risks of hyperhydration as well as hypohydration for any sporting event or individual athlete, and prepare appropriate practice and education strategies.
(4)
Develop personalized fluid intake plans that incorporate fluid availability characteristics of the sport or event. Where there is a likelihood of hypohydration, be proactive and creative in making use of existing opportunities for fluid intake within sport rules and characteristics and be prepared to request for changes when there is a likelihood of a serious mismatch between fluid losses and the opportunity to address these.
(5)
Practice intended competition drinking plans ahead of time to determine their suitability and allow time for readjustment.
6. Intrinsic Factors
A number of intrinsic factors modulate the individual variances that are observed in fluid losses. One of the greatest considerations for an individual’s sweat rate is his or her body size. Larger individuals typically have higher sweat losses, with football linemen exhibiting some of the highest recorded sweat rates [14]. Therefore, required absolute drink volumes will be higher for these athletes. An individual’s thirst drive also dictates how much they desire to drink during exercise, but this may not match their actual fluid needs. Indeed, multiple authors report that athletes voluntarily dehydrate during exercise due to discrepancies in fluid losses and drinking behavior [53,54]. Case studies of individuals who have developed hyponatremia due to excessive drinking during exercise also note that they reported thirst as an underlying contributor to their fluid intake [55].
Heat acclimatization contributes to variations in an individual’s sweating rate responses. Individuals who are heat acclimatized exhibit greater sweat rates which can pose a greater risk of hypohydration [56]. Although the increased sweat provides extra heat dissipation, it also requires extra fluid intake.
Women may be at greater risk for exercise-induced hyponatremia. This risk has been attributed to their lower body weight and size, excess water ingestion, and longer racing times relative to men [57]. The greater incidence of hyponatremia in women is unlikely due to their greater levels of estradiol in plasma and tissue. Although female sex-hormones can also influence neural and hormonal control of thirst, fluid intake, sodium appetite and sodium regulation [58,59], there is no evidence that anything beyond stature and drinking behavior significantly impact their risk.
Practical Solutions:
7. Sport-Specific Factors
Weight Division, Acrobatic and Appearance-Based Sports
The culture and normal behaviors surrounding specific sports can greatly affect the hydration practices of its athletes. The three most prominent examples of the cultural effects of sports on hydration practices are weight division sports, acrobatic sports and appearance-based sports. In weight division sports (e.g., combat sports, horse racing, lightweight rowing, etc.), the practice of deliberately dehydrating to manipulate body mass to meet lighter competition weight classifications is common [60]. In many cases, athletes not only sacrifice their performance through these practices but also endanger their health and well-being. In a similar fashion, sports where body-image and appearance are emphasized (e.g., cheerleading, body building and gymnastics), dangerous practices, such as extreme fluid restriction may be used by athletes to cheat “unofficial” weight checks that are self-instigated or expected within their training environment. Finally, “acrobatic” feats such as gymnastics, jumping and climbing are aided by a high power to weight ratio, but should not rely on severe hypohydration to achieve this. Excessive use of dehydration to manage body mass goals should be corrected to avoid long-term health complications [61].
Practical Solutions:
8. Conclusions
Based on the factors in the above sections, along with published literature on typical fluid balance observations in various sports [62,63], we assigned risks of hypohydration to the sports in and . These determinations can be used as a general guideline for sports that pose large risks for fluid imbalances that may limit sport performance. The factors for individual situations or geographical locations may vary and should be considered based on the principles mentioned above to tailor the necessary fluid replacement accommodations. An example of using this paradigm to develop a hydration plan can be found in .
Table 3
Establishing a Hydration Plan.
| Guiding Question | Steps to Correct | Implementation Example |
|---|---|---|
| Are athletes in a state of optimal hydration? | ||
| Is the exercise prolonged or intense? | ||
| Is the exercise being performed in environmental conditions that lead to greater fluid losses? | ||
| Is fluid available throughout the entire duration of exercise? |
| |
| Are there individuals with intrinsic risk factors? |
| |
| Are there sport-specific factors that need to be considered? |
In this paper we present a paradigm that can be used by clinicians and practitioners to develop hydration strategies for sports based on fluid availability, environment and exercise intensity. These tools are provided to inform hydration education and practices in a dynamic and individualized manner so that athletes can adapt to different circumstances and optimize performance.
Author Contributions
All authors attended the meeting and contributed to drafting and revision of the manuscript. All authors approved the final version of the paper.
Funding
The meeting preceding this manuscript was funded by PepsiCo (Gatorade).
Conflicts of Interest
Douglas Casa is the Chief Executive Officer of the Korey Stringer Institute, a 503.c not for profit which subsists on the donations from our corporate partners who include Gatorade, CamelBak, NFL, NATA, Mission, Eagle Pharmaceuticals and Kestrel. He has also been a recipient of grant funds from the following entities to study hydration related products: GE Healthcare, Halo Wearables, Nix Inc., CamelBak. William Adams has consulted with the following entities regarding hydration and exercise performance or the development of hydration assessment devices: BSX Athletics; Samsung Oak Holdings, Inc; Nobo, Inc; Clif Bar &Company; The Gatorade Company, Inc. Lawrence Armstrong is a hydration consultant to Danone Nutricia Research, France and the Drinking Water Research Foundation, Alexandria VA, USA. Lindsay Baker is employed by the Gatorade Sports Science Institute, a division of PepsiCo, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc. Louise Burke was a member of the Gatorade Sports Science Institute’s Expert Panel from 2014–2015 for which her workplace received an honorarium. Jose Gonzalez-Alonso was a member of the Gatorade Sports Science Institute’s Expert Panel in 2017 for which his workplace received an honorarium. Stavros Kavouras has served as scientific consultant for Quest Diagnostics, Standard Process and Danone Research and has active grants with Danone Research. The funders had no role in the in the writing of the manuscript.
References
1. Sawka M., Pandolf K.B. Effects of body water loss on physiological function and exercise performance. In: Gisolfi C., Lamb D.R., editors. Perspectives in Exercise Science and Sports Medicine. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 1–38. [Google Scholar]2. Sawka M.N., Wenger C.B., Pandolf K.B. Thermoregulatory Responses to Acute Exercise-Heat Stress and Heat Acclimation. In: Terjung R., editor. Comprehensive Physiology. John Wiley & Sons; Hoboken, NJ, USA: 2011. pp. 97–151. [Google Scholar]3. Montain S.J., Coyle E.F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [PubMed] [CrossRef] [Google Scholar]4. Montain S.J., Sawka M.N., Latzka W.A., Valeri C.R. Thermal and cardiovascular strain from hypohydration: Influence of exercise intensity. Int. J. Sports Med. 1998;19:87–91. doi: 10.1055/s-2007-971887. [PubMed] [CrossRef] [Google Scholar]5. Sawka M.N., Young A.J., Francesconi R.P., Muza S.R., Pandolf K.B. Thermoregulatory and blood responses during exercise at graded hypohydration levels. J. Appl. Physiol. 1985;59:1394–1401. doi: 10.1152/jappl.1985.59.5.1394. [PubMed] [CrossRef] [Google Scholar]6. Adams W.M., Ferraro E.M., Huggins R.A., Casa D.J. Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 2014;28:2380–2389. doi: 10.1519/JSC.0000000000000501. [PubMed] [CrossRef] [Google Scholar]7. Kenefick R.W., Cheuvront S.N. Physiological adjustments to hypohydration: Impact on thermoregulation. Auton. Neurosci. 2016;196:47–51. doi: 10.1016/j.autneu.2016.02.003. [PubMed] [CrossRef] [Google Scholar]8. Trangmar S.J., Gonzalez-Alonso J. New Insights into the Impact of Dehydration on Blood Flow and Metabolism during Exercise. Exerc. Sport Sci. Rev. 2017;45:146–153. doi: 10.1249/JES.0000000000000109. [PubMed] [CrossRef] [Google Scholar]9. Gonzalez-Alonso J., Crandall C.G., Johnson J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008;586:45–53. doi: 10.1113/jphysiol.2007.142158. [PMC free article] [PubMed] [CrossRef] [Google Scholar]10. Trangmar S.J., Gonzalez-Alonso J. Heat, Hydration and the Human Brain, Heart and Skeletal Muscles. Sports Med. 2019;49:69–85. doi: 10.1007/s40279-018-1033-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]11. Cheuvront S.N., Carter R., 3rd, Sawka M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003;2:202–208. doi: 10.1249/00149619-200308000-00006. [PubMed] [CrossRef] [Google Scholar]12. Cheuvront S.N., Kenefick R.W., Montain S.J., Sawka M.N. Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 2010;109:1989–1995. doi: 10.1152/japplphysiol.00367.2010. [PubMed] [CrossRef] [Google Scholar]13. Barr S.I. Effects of dehydration on exercise performance. Can. J. Appl. Physiol. 1999;24:164–172. doi: 10.1139/h99-014. [PubMed] [CrossRef] [Google Scholar]14. Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007;39:377–390. [PubMed] [Google Scholar]15. McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O′Connor F.G., Roberts W.O. National Athletic Trainers′ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [PMC free article] [PubMed] [CrossRef] [Google Scholar]16. Judelson D.A., Maresh C.M., Anderson J.M., Armstrong L.E., Casa D.J., Kraemer W.J., Volek J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007;37:907–921. doi: 10.2165/00007256-200737100-00006. [PubMed] [CrossRef] [Google Scholar]17. Coyle E.F. Physiological determinants of endurance exercise performance. J. Sci. Med. Sport. 1999;2:181–189. doi: 10.1016/S1440-2440(99)80172-8. [PubMed] [CrossRef] [Google Scholar]18. Adams J.D., Sekiguchi Y., Suh H.G., Seal A.D., Sprong C.A., Kirkland T.W., Kavouras S.A. Dehydration Impairs Cycling Performance, Independently of Thirst: A Blinded Study. Med. Sci. Sports Exerc. 2018;50:1697–1703. doi: 10.1249/MSS.0000000000001597. [PubMed] [CrossRef] [Google Scholar]20. Bergeron M.F., Bahr R., Bartsch P., Bourdon L., Calbet J.A.L., Carlsen K.H., Castagna O., González-Alonso J., Lundby C., Maughan R.J., et al. International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br. J. Sports Med. 2012;46:770–779. doi: 10.1136/bjsports-2012-091296. [PubMed] [CrossRef] [Google Scholar]21. Racinais S., Alonso J.M., Coutts A.J., Flouris A.D., Girard O., Gonzalez-Alonso J., Hausswirth C., Jay O., Lee J.K., Mitchell N., et al. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015;49:1164–1173. doi: 10.1136/bjsports-2015-094915. [PMC free article] [PubMed] [CrossRef] [Google Scholar]22. Carter J.E., Gisolfi C.V. Fluid replacement during and after exercise in the heat. Med. Sci. Sports Exerc. 1989;21:532–539. doi: 10.1249/00005768-198910000-00007. [PubMed] [CrossRef] [Google Scholar]23. Coyle E.F., Hamilton M. Fluid replacement during exercise: Effects on physiological homeostasis and performance. In: Gisolfi C., Lamb D.R., editors. Fluid Homeostasis During Exercise. Volume 3. Benchmark Press; Carmel, CA, USA: 1990. pp. 281–308. [Google Scholar]24. Mora-Rodriguez R., Hamouti N., Del Coso J., Ortega J.F. Fluid ingestion is more effective in preventing hyperthermia in aerobically trained than untrained individuals during exercise in the heat. Appl. Physiol. Nutr. Metab. 2013;38:73–80. doi: 10.1139/apnm-2012-0174. [PubMed] [CrossRef] [Google Scholar]25. Wittels P., Gunga H.C., Kirsch K., Kanduth B., Gunther T., Vormann J., Rocker L. Fluid regulation during prolonged physical strain with water and food deprivation in healthy, trained men. Wien. Klin. Wochenschr. 1996;108:788–794. [PubMed] [Google Scholar]26. Armstrong L.E. Hydration assessment techniques. Nutr. Rev. 2005;63:S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [PubMed] [CrossRef] [Google Scholar]27. Cheuvront S.N., Kenefick R.W. CORP: Improving the status quo for measuring whole body sweat losses. J. Appl. Physiol. 2017;123:632–636. doi: 10.1152/japplphysiol.00433.2017. [PubMed] [CrossRef] [Google Scholar]28. Baker L.B., Lang J.A., Kenney W.L. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur. J. Appl. Physiol. 2009;105:959–967. doi: 10.1007/s00421-009-0982-0. [PubMed] [CrossRef] [Google Scholar]29. Armstrong L.E., Casa D.J. Methods to Evaluate Electrolyte and Water Turnover of Athletes. Athl. Train. Sports Health Care. 2009;1:1–11. doi: 10.3928/19425864-20090625-06. [CrossRef] [Google Scholar]30. Cheuvront S.N., Kenefick R.W. Am I Drinking Enough? Yes, No, and Maybe. J. Am. Coll. Nutr. 2016;35:185–192. doi: 10.1080/07315724.2015.1067872. [PubMed] [CrossRef] [Google Scholar]31. Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M.F., Kenefick R.W., LaGasse K.E., Riebe D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994;4:265–279. doi: 10.1123/ijsn.4.3.265. [PubMed] [CrossRef] [Google Scholar]32. Cheuvront S.N., Sawka M.N. Hydration Assessment of Athletes. Sports Sci. Exch. 2005;18:1–5. [Google Scholar]33. Stolwijk J.A., Saltin B., Gagge A.P. Physiological factors associated with sweating during exercise. Aerosp. Med. 1968;39:1101–1105. [PubMed] [Google Scholar]34. Parsons K. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance. 3rd ed. CRC Press; Boca Raton, FL, USA: 2014. [Google Scholar]35. Baker L.B., Barnes K.A., Anderson M.L., Passe D.H., Stofan J.R. Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 2016;34:358–368. doi: 10.1080/02640414.2015.1055291. [PubMed] [CrossRef] [Google Scholar]36. Nadel E.R. Control of sweating rate while exercising in the heat. Med. Sci. Sports. 1979;11:31–35. [PubMed] [Google Scholar]37. Horner K.M., Schubert M.M., Desbrow B., Byrne N.M., King N.A. Acute exercise and gastric emptying: A meta-analysis and implications for appetite control. Sports Med. 2015;45:659–678. doi: 10.1007/s40279-014-0285-4. [PubMed] [CrossRef] [Google Scholar]38. Budd G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [PubMed] [CrossRef] [Google Scholar]39. Kulka T.J., Kenney W.L. Heat balance limits in football uniforms how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30:29–39. doi: 10.3810/psm.2002.07.377. [PubMed] [CrossRef] [Google Scholar]40. Armstrong L.E., Johnson E.C., Casa D.J., Ganio M.S., McDermott B.P., Yamamoto L.M., Lopez R.M., Emmanuel H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010;45:117–127. doi: 10.4085/1062-6050-45.2.117. [PMC free article] [PubMed] [CrossRef] [Google Scholar]41. Hooper D.R., Cook B.M., Comstock B.A., Szivak T.K., Flanagan S.D., Looney D.P., DuPont W.H., Kraemer W.J. Synthetic garments enhance comfort, thermoregulatory response, and athletic performance compared with traditional cotton garments. J. Strength Cond. Res. 2015;29:700–707. doi: 10.1519/JSC.0000000000000783. [PubMed] [CrossRef] [Google Scholar]42. O′Brien C., Freund B.J., Sawka M.N., McKay J., Hesslink R.L., Jones T.E. Hydration assessment during cold-weather military field training exercises. Arct. Med. Res. 1996;55:20–26. [PubMed] [Google Scholar]43. Fusch C., Gfrorer W., Koch C., Thomas A., Grunert A., Moeller H. Water turnover and body composition during long-term exposure to high altitude (4900–7600 m) J. Appl. Physiol. 1996;80:1118–1125. doi: 10.1152/jappl.1996.80.4.1118. [PubMed] [CrossRef] [Google Scholar]44. Mitchell J.W., Nadel E.R., Stolwijk J.A. Respiratory weight losses during exercise. J. Appl. Physiol. 1972;32:474–476. doi: 10.1152/jappl.1972.32.4.474. [PubMed] [CrossRef] [Google Scholar]45. Grundstein A., Williams C., Phan M., Cooper E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015;56:55–60. doi: 10.1016/j.apgeog.2014.10.014. [CrossRef] [Google Scholar]46. Cheuvront S.N., Caruso E.M., Heavens K.R., Karis A.J., Santee W.R., Troyanos C., D′Hemecourt P. Effect of WBGT Index Measurement Location on Heat Stress Category Classification. Med. Sci. Sports Exerc. 2015;47:1958–1964. doi: 10.1249/MSS.0000000000000624. [PubMed] [CrossRef] [Google Scholar]47. Casa D.J., DeMartini J.K., Bergeron M.F., Csillan D., Eichner E.R., Lopez R.M., Ferrara M.S., Miller K.C., O′Connor F., Sawka M.N., et al. National Athletic Trainers′ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015;50:986–1000. doi: 10.4085/1062-6050-50.9.07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]48. Minehan M.R., Riley M.D., Burke L.M. Effect of flavor and awareness of kilojoule content of drinks on preference and fluid balance in team sports. Int. J. Sport Nutr. Exerc. Metab. 2002;12:81–92. doi: 10.1123/ijsnem.12.1.81. [PubMed] [CrossRef] [Google Scholar]49. Burdon C.A., Johnson N.A., Chapman P.G., O′Connor H.T. Influence of beverage temperature on palatability and fluid ingestion during endurance exercise: A systematic review. Int. J. Sport Nutr. Exerc. Metab. 2012;22:199–211. doi: 10.1123/ijsnem.22.3.199. [PubMed] [CrossRef] [Google Scholar]50. Williams J., Tzortziou Brown V., Malliaras P., Perry M., Kipps C. Hydration strategies of runners in the London Marathon. Clin. J. Sport Med. 2012;22:152–156. doi: 10.1097/JSM.0b013e3182364c45. [PubMed] [CrossRef] [Google Scholar]51. Chorley J., Cianca J., Divine J. Risk factors for exercise-associated hyponatremia in non-elite marathon runners. Clin. J. Sport Med. 2007;17:471–477. doi: 10.1097/JSM.0b013e3181588790. [PubMed] [CrossRef] [Google Scholar]52. Maughan R.J., Shirreffs S.M. Development of individual hydration strategies for athletes. Int. J. Sport Nutr. Exerc. Metab. 2008;18:457–472. doi: 10.1123/ijsnem.18.5.457. [PubMed] [CrossRef] [Google Scholar]53. Passe D., Horn M., Stofan J., Horswill C., Murray R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007;17:284–295. doi: 10.1123/ijsnem.17.3.284. [PubMed] [CrossRef] [Google Scholar]54. Hosseinlou A., Khamnei S., Zamanlu M. The effect of water temperature and voluntary drinking on the post rehydration sweating. Int. J. Clin. Exp. Med. 2013;6:683–687. [PMC free article] [PubMed] [Google Scholar]55. Hew-Butler T., Rosner M.H., Fowkes-Godek S., Dugas J.P., Hoffman M.D., Lewis D.P., Maughan R.J., Miller K.C., Montain S.J., Rehrer N.J., et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [PubMed] [CrossRef] [Google Scholar]56. Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis. Sports Med. 2016;46:1699–1724. doi: 10.1007/s40279-016-0538-5. [PubMed] [CrossRef] [Google Scholar]57. Almond C.S., Shin A.Y., Fortescue E.B., Mannix R.C., Wypij D., Binstadt B.A., Duncan C.N., Olson D.P., Salerno A.E., Newburger J.W. Hyponatremia among runners in the Boston Marathon. N. Engl. J. Med. 2005;352:1550–1556. doi: 10.1056/NEJMoa043901. [PubMed] [CrossRef] [Google Scholar]58. Ishunina T.A., Swaab D.F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus; size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 1999;84:4637–4644. doi: 10.1210/jcem.84.12.6187. [PubMed] [CrossRef] [Google Scholar]59. Sar M., Stumpf W. Simultaneous localization of [3 H] estradiol and neurophysin I or arginine vasopressin in hypothalamic neurons demonstrated by a combined technique of dry-mount autoradiography and immunohistochemistry. Neurosci. Lett. 1980;17:179–184. doi: 10.1016/0304-3940(80)90081-6. [PubMed] [CrossRef] [Google Scholar]60. Barley O.R., Chapman D.W., Abbiss C.R. Weight Loss Strategies in Combat Sports and Concerning Habits in Mixed Martial Arts. Int. J. Sports Physiol. Perform. 2018;13:933–939. doi: 10.1123/ijspp.2017-0715. [PubMed] [CrossRef] [Google Scholar]61. Bonci C.M., Bonci L.J., Granger L.R., Johnson C.L., Malina R.M., Milne L.W., Ryan R.R., Vanderbunt E.M. National athletic trainers′ association position statement: Preventing, detecting, and managing disordered eating in athletes. J. Athl Train. 2008;43:80–108. doi: 10.4085/1062-6050-43.1.80. [PMC free article] [PubMed] [CrossRef] [Google Scholar]62. Nuccio R.P., Barnes K.A., Carter J.M., Baker L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017;47:1951–1982. doi: 10.1007/s40279-017-0738-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]63. Garth A.K., Burke L.M. What do athletes drink during competitive sporting activities? Sports Med. 2013;43:539–564. doi: 10.1007/s40279-013-0028-y. [PubMed] [CrossRef] [Google Scholar]
Importance of Hydration for Young Athletes
While drinking enough water may seem like a simple action, it impacts virtually every aspect of sports performance.
Staying hydrated increases energy, improves movement, recovery and agility, thermoregulation, and aids in mental clarity and activity – all of which can improve physical performance and reduce the risk of injuries.
Why is hydration important in sports?
Almost every measurement of performance – aerobic endurance, strength, power, speed, agility and reaction time – decreases with as little as 2% dehydration. Learn more about the signs and symptoms of dehydration.
Benefits of staying hydrated include:
- Improved muscle function. Hydrated muscles function better than dehydrated muscles.
- Regulated blood pressure. Staying hydrated helps maintain blood pressure during exercise so your heart doesn’t work harder to maintain normal blood pressure.
- Improved circulation. Staying hydrated also improves blood flow and circulation and thus the delivery of oxygen and nutrients to working muscles. Good hydration also helps remove metabolic by-products and waste from muscles, while replacing the water that is lost through sweat.
How can proper hydration help young athletes reduce injury risk?
Dehydration contributes to muscle fatigue, which can increase the risk for injury. Staying adequately hydrated can help reduce muscle fatigue and reduce the risk of injury.
As athletes exercise, the core body temperature rises. In response, the body sweats to dissipate excess heat so it doesn’t overheat. Staying hydrated replaces the water lost through sweating and is essential for thermoregulation, helping to prevent cramps, heat exhaustion and heat stroke.
Recommended daily water intake for athletes
Fluid needs vary based on activity, intensity, environmental conditions, body size of the athlete and training status. The more highly trained an athlete is, the more he or she will sweat and require more water.
To maintain optimal hydration throughout the day, young athletes should drink ½ to 1 ounce of water per pound of body weight. To maintain peak performance during exercise, minimize water weight loss to no more than 2% of your body weight. This means that a 100-pound athlete should lose no more than 2 pounds during a workout.
Athletes should drink plenty of water in the hours leading up to practice. Continue taking four to six big gulps of water every 15 to 20 minutes during exercise. After exercising, drink 24 ounces of water for every pound of water weight you lose during your workout.
Calculating sweat rate
Knowing an athlete’s sweat rate is important when monitoring hydration. Sweat rate is the amount or rate at which a person sweats. To calculate sweat rate, measure weight before and after a workout. The difference in the weight indicates how well the athlete is staying hydrated and whether it’s within the healthy guidelines. The weight difference plus any fluids consumed during workout equals the sweat rate. Understanding this number will guide the amount of fluid needed during the workouts or practices.
Water or sports drink: What is best for athletes?
If young athletes are working out for one hour or less, water is generally sufficient to keep hydrated. Sports drinks may be recommended in certain situations including when:
- Exercise lasts longer than 1 hour
- Engaging in intense workouts
- Practicing or playing in extreme environmental conditions, such as high heat and humidity
- Excessive sweating occurs, i.e., being a “heavy sweater”
In these situations, experts recommend a sports drink containing at least 110 to 240 mg of sodium per 8oz. serving. This will replace fluid and electrolytes lost through sweat.
Learn more
The specially trained experts at Children’s Health Andrews Institute Sports Performance powered by EXOS help young athletes perform their best while remaining healthy and safe. Contact us today to schedule an appointment.
Sign up for Performance Playbook
Receive the latest advice from our orthopedic and sports performance specialists – right in your inbox. Sign up for Performance Playbook, the monthly newsletter from Children’s Health Andrews Institute.
A brief history of hydration advice for athletes by Precision Hydration
Hydration advice for athletes has changed dramatically over the last ~100 years and we’ve taken a look at how things have changed during that time…
Contents:
Early 1900s – “Drink nothing”
The changes over time has been most clearly documented in the writings of Prof. Tim Noakes, along with two prominent ex-sports science students from his department at the University of Cape Town; Ross Tucker and Jonathan Dugas.
Their research into hydration concluded that, in the early 1900s, it was considered best practice to advise athletes to drink nothing, or as little as possible, during all athletic pursuits.
They highlight a quote from James E. Sullivan, Head of the Amateur Athletic Union, from 1909):
Don’t get in the habit of drinking and eating in a marathon race; some prominent runners do, but it is not beneficial.
Fast forward 50 years and the advice hadn’t really changed much.
In the 1960s, Tour de France rider Tommy Simpson’s trainer said…
Four small bottles for a long stage of the Tour, it is frowned upon to drink more. Avoid drinking when racing, especially in hot weather. Drink as little as possible, and with the liquid not too cold. It is only a question of will power.
1965 – The first sports drink
Then things started to change.
1965 was the year that Dr Robert Cade came up with the first iteration of the sports drink that eventually became known as ‘Gatorade’.
It was developed to combat the fatigue that the University of Florida football team – ‘The Gators’ – suffered in the oppressive heat and humidity that Florida is famous for.
The hypothesis was that this fatigue was often being caused by a combination of carbohydrate depletion, dehydration and electrolyte loss.
So a drink formulated with sugar, salts and water was developed and found to be remarkably effective.
Gatorade got off to a great start commercially and was named a sponsor of the NFL in 1969.
Rising sales led Gatorade’s marketers to promote the positive benefits of drinking and, increasingly, highlight the dangers of dehydration.
Image credit: Ethan McArthur via Unsplash (Copyright free).
In 1985, the Gatorade Sports Science Institute was set up.
It’s stated mission is to “help athletes optimize their health and performance through research and education in hydration and nutrition science”.
In the 80s and 90s, GSSI conducted studies into the effects of dehydration on performance.
Many of these studies appeared to demonstrate that dehydration was a serious performance limiter, especially during endurance sports in the heat.
And, over time, this message gradually became established as ‘fact’ within the sporting community.
1996 – “Replace 100% of Sweat Losses”
This reached its height in 1996, with the American College of Sports Medicine’s, ‘Position Stand on Exercise and Fluid Replacement’. It included the statement:
During exercise, athletes should start drinking early and at regular intervals in an attempt to consume fluids at a rate sufficient to replace all the water lost through sweating or consume the maximal amount that can be tolerated.
The movement from ‘nil by mouth’, to ‘consume as much as can be tolerated’ is one of those classic ‘pendulum swings’ in the world of sports science. Other examples include the High Carb vs Low Carb diet debate and Cushioned, Supportive running shoes vs Barefoot Running.
These polarisations tend to occur because human brains love simple answers and ‘either/or, black or white’ debates. We struggle with grey areas, even though that tends to be where the answers to complicated questions often reside!
Prof. Tim Noakes was amongst the first to question whether the ‘drink, drink, drink’ philosophy’ was really a good idea.
He uncovered a growing number of cases of hyponatremia – a sometimes fatal condition characterised by low blood sodium levels – in an increasing number of endurance athletes who had seemingly followed advice to drink as much as they could.
Noakes went on to write a thoroughly researched and emotionally-charged book called ‘Waterlogged. The Serious Problem of Overhydration in Endurance Sports’.
In this he suggests that hyponatremia has become a significant problem largely
because of the marketing efforts of the sports drink industry.
He makes the tragic point that there have been a number of preventable deaths
from over-drinking and that these could have been avoided with more balanced messaging.
It’s impossible to argue that the the sports drink industry, has not been influential in over-emphasising the dangers of dehydration and this counter argument has definitely started to have an impact.
2007 – Prevent >2% dehydration
In 2007 the American College of Sports Medicine updating it’s guidelines:
The goal of drinking during exercise is to prevent excessive Dehydration (>2% body weight loss) and excessive changes in electrolyte balance to avert compromised performance.
Because there is considerable variability in sweating rates and sweat electrolyte content between individuals, customized fluid replacement programs are recommended.
Individual sweat rates can be estimated by measuring body weight before and after exercise.
This was definitely a significant step away from ‘drink as much as tolerable’,
but it’s correctness and practical usefulness to athletes has still been challenged.
Noakes and his supporters cite numerous examples of world-class performances occurring when dehydration has exceeded 2%, sometimes by a significant amount.
Like when marathon runner Halie Gebraselassie lost almost 10% of his body weight during a 2:05:29 marathon winning performance in Dubai in 2009.
Data collected on large numbers of IRONMAN finishers in New Zealand and South Africa shows that most of the field ended up significantly dehydrated at the finish line and that some of the faster finishers were in fact some of the most dehydrated of all, losing in the region of 2-7% of their bodyweight.
This kind of evidence, along with real world experience from endurance athletes, suggests that an arbitrary, 2% dehydration limit is neither useful, nor correct in all scenarios.
The truth is significantly more complex and seeking a simpler, ‘one-size-fits-all’ solution can be counter-productive.
Waterlogged and “drink to thirst”
Noakes’ current theory is that athletes simply need to drink water to the dictates of thirst in order to avoid hyponatremia, whilst maintaining sufficient hydration levels for survival and the maintenance of performance.
This theory has won a lot of support in recent years.
He argues, quite compellingly, that the human body is designed to optimize its own hydration levels so, if you drink to thirst, that is basically all you need to know about hydration. End of story.
This approach has merit in many circumstances. It’s likely to be compatible with the main goal of avoiding over-drinking for most people in normal situations.
But, it’s also yet another oversimplification in the field of hydration ‘marketing’, as it’s unlikely to be true for all athletes, all of the time.
There’s evidence that a pre-planned hydration strategy may be more effective for those engaging in very high intensity, medium duration (i.e. ~1-3 hours) endurance events where maintenance of blood volume is critical to support very high levels of performance.
One reason ‘drinking water to thirst’ might not always work is because sweat contains relatively large, and quite variable, levels of electrolytes, so prolonged sweating can deplete the body of these finite reserves.
This is most likely to be the case during ultra-distance events, where total sweat losses can be significant over a long period of time, especially in the heat.
Maybe because of the human tendency towards tribalism, there are currently two opposing camps in hydration science. There’s those who back the ‘drink water to thirst’ argument and those who are proponents of a ‘drink to a plan’ approach (such as Dr Stavros Kavouras’ group working out of The University of Arkansas in the USA, for example).
As is so often the case when considering two completely opposing ideas, it’s a good idea to look for the middle ground for clues as to where truths are likely to be found.
What’s the best approach to hydration?
At the sharp end, it seems that opinion is moving towards a view that, whilst drinking to thirst is a sensible approach for shorter or lighter activities, during very long events in the heat, when total sweat and electrolyte losses are high, replenishment might need to be approached more proactively than would be the case in shorter bouts of activity.
Examples of the efficacy of this approach include this 2015 study by researchers in Spain, which showed faster racing times for athletes given salt supplements during a middle distance triathlon compared to a control group given placebos.
Here’s what 2016 Ironman 70.3 World Champ Tim Reed has to say about drinking to thirst…
Drinking to thirst is likely to be a good approach in day to day life, or endurance training completed at a very low intensity. But, in my opinion, it’s a terrible approach for those looking to maximize their performance in endurance events.
My thirst response doesn’t really kick in until I’ve already lost 1 liter of fluid or more. While that shouldn’t drastically affect my performance, I still continue to lose
far more than I replace after my thirst response has kicked in, and so inevitably have to slow my speed as my blood volume continues to decline.
When drinking to thirst, I can lose 4-4.5kgs in a 2 hour run, leaving my heart rate very high and my performance very lethargic.
During a race, my thirst response is even more subdued due to my ‘fight or flight’ system running on overdrive.
Perhaps there are athletes whose thirst response provides a more reliable guide, but in my experience with both coaching and racing, drinking to a schedule, particularly in the first half of events, leads to vastly better performance outcomes.”
Image credit: Dale Travers ©.
We also asked Sarah Crowley, who came 3rd at the 2017 IRONMAN World Champs and was the 2018 IRONMAN South America Champion, for her opinion on how best to approach hydration planning based on her own experiences…
Initially I had no idea what I needed to stay hydrated for long course triathlons, having come from ITU. I raced with one gel and a bottle of sports drink in my first 70.3. It ended badly.
After the race I got some good advice. It was to basically work out my general hydration and fuelling needs based on my weight and expected race times. I was also given some general advice to eat and drink at regular intervals.
I took this advice and repeatedly practiced and refined what and when I ate and drank by systematically testing different things during brick training sessions over a period of two years!
I would write down a list of exactly what I had and the intervals each time which meant I had a record of what went well and what didn’t.
People often asked me what I ate and drank, so I told them. I’d often hear after races that they had followed a very similar hydration and food strategy but that it didn’t go so well. My point being, it’s so individual and also dependant on the course and the weather that you can’t copy a formula, you must work out what works for you. I am constantly refining this.
Together, I think these two examples illustrate very nicely that, whilst drinking to thirst is a sensible guiding principal and basis for how to approach hydration for shorter/low sweat activities, a more proactive and individualised approach is probably what’s needed for longer, hotter and sweatier events where drinking water to thirst is unlikely to sufficient to maintain optimal performance and health.
Other scenarios where a pre-planned, but flexible and personalised, approach might be beneficial include…
1) During moderate duration, high intensity activities where the maintenance of blood volume to assist cardiac output, heat dissipation and other metabolic challenges is very important.
2) During days and weeks of back-to-back, hard or high intensity training or competition in hot conditions, where cumulative sweat losses have the potential to cause stepwise depletion in fluid and electrolyte levels in the body.
3) When individuals have exceptionally high sweat sodium losses and need to be more aggressive with replacement protocols to balance those out.
4) When the athlete is inexperienced and so all of the sensations associated with pushing their bodies very hard are relatively new and difficult to interpret accurately.
5) In environments where opportunities to access fluids are limited or constrained.
6) Where drinking at certain times and abstaining at others can be tactically advantageous, such as in bike racing or Long Distance triathlons.
Hopefully this brief summary of a hundred years or so of hydration advice leaves you in an informed position from which you can start understanding your own individual hydration needs and refine your strategy from there.
Further reading
Build A Better Athlete: Proper hydration tips
In the fifth nutrition article of our year-long Build A Better Athlete series, we focus on what might be the most important topic as we start to get into warmer weather — hydration. University of Michigan director of sports nutrition Caroline Mandel, a registered dietitian, says the goals of hydration are to delay fatigue, maintain mental focus, regulate body temperature (especially in hot environments), satisfy thirst and to improve the ability to recover from training and competition.
Yet, for how important staying hydrated is, Mandel says that research shows that most athletes typically only drink half of what they need.
ESPNHS: What’s the ideal amount of fluid an adolescent athlete should consume during training and competition?
Mandel: Fluid needs depend on the intensity and duration of the activity as well as the environmental conditions and the types of clothing/equipment worn. In general, high school athletes require 10 to 12 cups of fluid (water, fruit juice, milk, etc.) per day consumed at meals and snacks so they start exercise in a hydrated state. During exercise, athletes require 4 to 8 ounces of fluid every 15 to 20 minutes. Fluid intake can then be adjusted based on weight change and monitoring urine color and volume before and after exercise. An athlete is hydrated if he/she produces urine in a sufficient volume and that is light in color. If less than two hours prior to training or competition the athlete does not produce urine or if the urine is dark in color, they are not hydrated and should slowly drink more fluids. I recommend that athletes weigh themselves before and after training and competition at least two times per season to gauge their specific fluid needs. The goal is to start exercise in a hydrated state and drink adequately during exercise to prevent weight loss.
What types of fluids should you avoid while training? Which do you recommend?
Mandel: According to the American Academy of Pediatrics, energy drinks have no place in the diets of children and adolescents. The best fluid choices for young athletes are water and sports drinks. Water is a great hydrator and is fine for exercise that lasts less than an hour and exercise on cool days. For intense exercise that lasts longer than an hour and for exercise on hot and humid days, a sports drink that contains carbohydrate (no more than 14 grams per 8 fluid oz.) and electrolytes like sodium and potassium has been shown to improve voluntary hydration and prevent dehydration better than water alone. Milk, chocolate milk and fruit juices should be avoided during training or competition because their carbohydrate content is too high and causes an upset stomach. It also slows the rate of gastric emptying and fluid absorption.
ESPNHS: Are there any foods that can help keep you hydrated and can also provide essential nutrients?
Mandel: We consume around 80 percent of our daily fluid from beverages and around 20 percent from foods. Hydrating foods include fruits, vegetables and yogurt and even cooked beans, rice, pastas and cereals since they are cooked in water or other liquids. During exercise, blood is shunted away from the GI track to working muscles. Most solid foods are not well tolerated during intense exercise, so athletes should practice with hydrating foods during practices to find what works best for them.
ESPNHS: What are the warning signs of dehydration?
Mandel: Heat illness occurs in three stages:
• Heat cramps, which are categorized by excess sweating, fatigue, thirst and cramps, usually in the stomach, arms or legs. This condition is common in very hot weather or with moderate to heavy physical activity. You can usually treat heat cramps by drinking water or fluids containing electrolytes (such as sports drinks), resting and getting to a cool spot, like a shaded or air-conditioned area.
• Heat exhaustion occurs when you don’t act on the signs and symptoms of heat cramps and your condition worsens. Signs and symptoms of heat exhaustion include a headache, dizziness or lightheadedness, nausea, skin that feels cool and moist, and muscle cramps. Often with heat exhaustion, you can treat the condition yourself by following the same measures used to treat heat cramps, such as drinking cool beverages, getting into an air-conditioned area or taking a cool shower. If symptoms persist, seek medical attention immediately.
• Heat stroke. A body temperature of 104 degrees Fahrenheit or higher is the main sign of heatstroke. In heat stroke brought on by hot weather, your skin will feel hot and dry to the touch. However, in heatstroke brought on by strenuous exercise, your skin may feel moist. You may feel sick to your stomach or vomit. Your skin may turn red as your body temperature increases. Your breathing may become rapid and shallow. Your pulse may significantly increase because heat stress places a tremendous burden on your heart to help cool your body. You may experience a throbbing headache. You may have seizures, hallucinate, or have difficulty speaking or understanding what others are saying. You may pass out or fall into a state of deep unconsciousness (coma). Your muscles may feel tender or cramped in the early stages of heatstroke, but may later go rigid or limp.
ESPNHS: Is there ever such a thing as being over-hydrated while training?
Mandel: Hyponatremia is a potentially deadly disorder that results from over-consumption of fluids where the sodium content of the blood is diluted to dangerous levels. It is extremely rare in high athletes but has been seen in endurance events that last longer than 4 hours, such as marathons and triathlons, when participants consume large amounts of water over several hours without adequate sodium intake. Affected individuals may experience disorientation, altered mental status, headache, lethargy and seizures. Suspected hyponatremia is a medical emergency and is diagnosed by testing blood sodium levels. Treatment is through administering intravenous fluids containing sodium.
Hydration of the body | Mad Wave
20563
Hydration of the body
How much you need to drink to stay dry during training
09/12/2018
You, of course, have heard the expression “Water is life”, but have you ever wondered how familiar this phrase important for swimmers?
Influence of water balance on training
Water is the environment in which swimmers undergo most of their training, therefore athletes often do not understand how much they lose fluids and do not notice when they really feel thirsty, because it seems easier to do without drinking in the pool than during training on land.
Water is essential for all metabolic processes, many of which affect the maintenance and recovery of working capacity, as well as the effectiveness of training. Our muscles are 73% water, so hydration (from ancient Greek ὕδωρ “water”) plays a huge role in all processes – from muscle recovery to protein synthesis and absorption of nutrients.
From the mouth through the esophagus, water enters the stomach and then into the intestines. There it is actively absorbed, and together with the water, the substances dissolved by it are absorbed, and those that were in it from the very beginning – salts, minerals, trace elements, and those that entered our body along with food.Here water manifests itself as a powerful solvent that provides our cells with all the necessary substances. Once inside, the water travels through the blood vessels throughout the body. The blood itself consists of half of blood cells, and half of plasma, which is precisely water with organic and mineral compounds dissolved in it. Water, which has fulfilled its function of transferring the necessary substances throughout the body, before leaving it, performs another important action.As a result of biochemical reactions (processing of proteins and carbohydrates), natural waste remains – slags. Water also dissolves them, after which it leaves the body. Water is excreted not only in urine. About 50% of the consumed water is excreted through the kidneys, 15% is excreted through the intestines, another 15% is exhaled into the environment, the remaining 20% is evaporated through the skin.
“If you do not drink water, basic biochemical reactions do not occur in your body.”
Dave Salo, Especially for mad wave
Hydration also helps regulate body temperature and joint function – both are extremely important for swimming, so it is impossible to achieve good results with imbalances in water balance without harming your body.
The importance of hydration for swimmers also lies in the fact that our blood contains 93% water, and the blood transports oxygen and essential nutrients to provide the body with energy and maintain health. Getting enough water helps the heart pump blood more efficiently.
“A decrease in the required amount of fluid in the body by only 2% can lead to a decrease in performance by 10-20%. This is an impressive loss – you will be wasting a lot of effort during training without getting a significant improvement in results.”
Mad Wave Team
Dehydration of any degree can adversely affect a swimmer’s performance during a swim. With dehydration, swimmers get tired faster during training, react more slowly, and increase the risk of injury and seizures not only in the pool, but also outside it.
In short, you won’t be able to train and recover properly without proper hydration, so it is very important to provide the body with the necessary elements for this.
Signs of dehydration
One of the easiest ways to detect dehydration is when you are thirsty.But when this symptom appears, the body is most likely already dehydrated. Other symptoms of dehydration are general fatigue and stress. Since the brain tissue is 70-80% water, with dehydration, mental activity deteriorates, fatigue and irritability appear. All this, of course, affects the performance of the swimmer in the pool.
The most accurate way to check your water balance is the color of your urine. Light yellow urine indicates normal water balance, the darker the urine, the more dehydrated.
“Dehydration is accompanied by certain symptoms: the loss of 1% of fluid makes you feel thirsty, 2% – decreased stamina, 3% – decreased strength, 5% – increased heart rate, apathy, muscle weakness, nausea.”
Mad Wave Team
The most accurate way to check your water balance is the color of your urine. Light yellow urine indicates normal water balance, the darker the urine, the more dehydrated.
Dehydration rate:
Water balance: 0 to 1%
Minimum dehydration: 1 to 3%
Significant dehydration: 3 to 5%
Severe dehydration: more than 5%
Depending on the intensity of work, each a thousand meters that an athlete swims during training or pre-competition warm-up leads to a loss of 100-200 ml of fluid.Thus, a swimmer can lose up to 1 liter of fluid in an hour. And we already know that fluid loss of more than 2% of a swimmer’s body weight can reduce the effect of high-intensity work by 45%.
How to avoid dehydration?
It is only possible to eliminate dehydration naturally by drinking clean drinking water. Tea, coffee, beer, alcohol, artificial drinks, in addition to containing water, also contain dehydrating substances such as caffeine, as well as various chemical components.
The topic of hydration has been thoroughly studied by many international organizations and research institutes, but the most widespread opinion of the US National Academy of Medical Sciences is that the average man aged 19-30 needs about 3.7 liters. liquids per day, and a woman of the same age group 2.7 liters. These calculations are based on the assumption that 1 gram of liquid should be consumed for 1 calorie of food eaten.
The World Health Organization believes that a person needs to drink 30 ml of water per day for every kilogram of a person’s weight.This method of calculation is the most correct and optimal, since the amount of water consumed must correspond to the mass of a person. With a weight of 100 kg, you need to consume 3 liters every day, and a person weighing 60 kg – 1.8 liters.
Both of these methods are useful for maintaining the water balance of the average adult, but swimmers must also consider fluid loss during training in the water.
The American College of Sports Medicine recommends that for regular exercise, drink 480-600 ml of water at least 15 minutes before training and 100-250 ml every 15 minutes during training.To do this, it is advisable to have a liter bottle of water on the side of the pool. Do not forget to drink water strictly on schedule, and not when you feel thirsty.
If you train at high intensity, weigh yourself before and after training to get a more accurate idea of the amount of water lost by the body. For optimal performance and health, it is recommended to drink 600 to 720 ml of water for every 500 grams lost. Changes in body weight indicate a risk of dehydration and whether the body is getting enough fluids.
By following these guidelines, you will be able to maintain your fluid levels and exercise longer and harder without becoming overworked or dehydrated. At the same time, do not forget that the body of each person is unique, has its own metabolism and constitution, and you need to regulate your drinking regime, taking into account personal characteristics.
Hydration before, during and after training, how to avoid dehydration
Do you know how many liters of water should you drink every day? How much liquid should you consume, during sports activities ? Do you know how to properly hydrate your body before, during and after training? Learn How To Prevent Dehydration , Optimal Drinking Regimen And Which Drinks Are Ideal For Athletes .
Water is the essence of all living things , and a person can live without it for only a few days. Water makes up 75% of body weight in infants and 90,050 55-70% in adults 90,051. [1] Regular drinking regimen is incredibly important for human health , the proper functioning of organs and the maintenance of the internal balance of the body. Any chemical reaction in the body, including the production of energy or the process of breaking down and storing glucose, requires water .Only when there is sufficient fluid in the body, enzymes and hormones can develop their potential and fully utilize their effect. [21]
Sources of hydration and fluid intake
Naturally, the main source of hydration of the body is water . However, it is possible to supplement body fluids by consuming water-rich foods . These are basically 90,050 watery fruits and vegetables 90,051. In the table you can find separation of products by the amount of water .[3]
| Water% | Foods |
|---|---|
| 90 – 99% | skim milk, melon, strawberries, lettuce, cabbage, celery, spinach, cucumbers, boiled pumpkin | fruit juice, yogurt, apple, grapefruit, orange, carrot, broccoli, pear, pineapple |
| 70 – 79% | banana, avocado, cottage cheese, ricotta, potatoes, corn, shrimps |
| 60 | pasta, legumes, salmon, ice cream, chicken breasts |
| 50 – 59% | beef, feta cheese, steak |
| 40 – 49% | pizza |
| 30 – 396% bread , confectionery | |
| 20 – 29% | pies, muffins |
| 10 – 19% | butter, margarine, raisins |
| 0 – 9% | nuts, chocolate biscuits, cr eckers, cereals, pretzels, peanut butter |
| 0% | vegetable oils, sugar |
The amount of liquid that a person receives from drinks and meals varies depending on the diet .While in the US, according to American experts, people get about 22% of their liquid from food, 90,050 in Europe this figure is clearly higher than 90,051, especially in countries where people consume a lot of fruits and vegetables, such as Greece. [2]
Ideal daily fluid intake
Many people suffer from a lack of fluid without even knowing it. For a healthy person, it is necessary to consume about 2.5 liters of liquid per day for normal breathing, sweating and excretion.This is why the general standards indicate a minimum fluid intake of 2 to 3 liters per day . [21] However, this is the minimum value that needs to be increased during physical and sporting activity or on hot summer days.
This means that you must drink at least 8-12 cups of water per day , 5 of which must be pure water. But again, these figures do not take into account the outside temperature and physical activity .
A good way to calculate ideal daily fluid intake for is to multiply your body weight (in kilograms) by 50 ml. [21] For example, 80 kg x 50 ml = 4000 ml , this means that if you weigh 80 kg, your daily fluid intake from food and beverages should be 4 liters . You can more accurately calculate your optimal fluid intake with the hydration calculator.
Dehydration as a problem of lack of fluid
The opposite of correct hydration is dehydration (or dehydration).The term dehydration means 90,050 a decrease in the volume of fluid in the body and therefore a negative balance of water in the human body. Dehydration can be caused by lack of fluid intake or increased fluid loss due to excessive sweating or excretion . By standards, a person is considered dehydrated if he / she loses more than 2% of his / her weight due to lack of fluid. [17] Dehydration is a medical condition that is manifested by symptoms such as:
- dry mouth
- minimal urination during the day
- general weakness
- dizziness
- dark, less transparent urine color
- dry,
chapped lips 9005 skin – after toko, how to pinch the skin, it slowly returns to its original place [17]
The symptoms of dehydration should not be underestimated, so we recommend to regularly consume liquid in order to avoid complications caused by dehydration.
You can link to products:
Health effects of dehydration
Dehydration is a serious health problem and can be fatal if a person does not drink for 3-4 days. [25] Among the 90,050 serious consequences of dehydration, should be noted [15] [16]:
- Delirium – mental disorder, occurring with impaired perception and thinking , which can lead to irreversible acquired dementia
- problems with kidney function
- dysfunction of the heart
- headaches
- dry skin
- digestive problems
- other chronic diseases
Essential Tips to Avoid Dehydration
The best prevention is Drinking liquid (water) regularly, even if you don’t feel thirsty or notice the warning signs of dehydration. This will help you develop the water habit and protect yourself from lack of fluids.
- Drink fluids regularly before, during, and after training.
- Drink fluids according to the pre-scheduled schedule .
- If you cannot control your fluid intake, install the application on your smartphone, which will do it for you and warn you when you need to consume fluid.
- Check your urine color . If it is the color of apple juice, then you are probably dehydrated. If your urine is light yellow, you have enough fluid in your body.
- Take shaker with you to your workout and drink it regularly, every 15-20 minutes.
- Drink less caffeine drinks . They are diuretic and can dehydrate you.
- Avoid alcoholic beverages. Even a cold glass of beer on a hot day is more diuretic than hydrating.
- Wear quality clothing , depending on the season, which will prevent overheating or hypothermia of your body. Wear lightweight clothing made from high quality materials when exercising. After training , change into dry clothes as soon as possible .
- If you suddenly and unexpectedly experience fatigue, headache or dizziness, Drink water! [17]
Everyone should protect themselves from dehydration, but primarily applies to athletes who are at risk of fluid and mineral deficiencies due to perspiration .
Fluid replenishment during physical activity
Some put forward theories that has fluid intake during physical and sports activity is undesirable. The development of awareness of correct hydration in sports has evolved over the years. So, if you were going to run the 90,050 marathon in the 1900s 90,051, you would be advised 90,050 not to drink the 90,051 liquid during the entire competition, based on the fact that it is harmful.Jackie Meckler, five-time Comrades Marathon winner, ran the 89-kilometer track in less than 6 hours , taking minimum fluid , he later said: “Running a marathon without drinking was considered the main goal of runners and proof of fitness success. ”[18]
Tom Simpson , the 1960 World Cycling Champion, also said that four small bottles of water for a long distance such as the Tour de France are sufficient.According to him, cyclists should avoid drinking fluids while racing , especially in warm weather. It’s just a matter of willpower . [18]
Liquid overdose
One extreme replaced the other with , and liquid overdose has become a trend in sports. Excessive water consumption is just as dangerous as dehydration. Liquid amount causes plasma dilution and low sodium levels. This condition is known as hyponatremia and can be fatal. The first recorded death from hyponatremia dates back to 1981, when a marathon runner died of “water intoxication” . Between 1985 and 2002 the idea of drinking plenty of fluids predominated among athletes, especially in the field of endurance sports. Doctors, at the time, recommended 90,050 to drink up to 1,200 ml per hour , which caused 247 cases of hyponatremia, of which 90,050 7 were fatal 90,051. [18]
After 2007 the situation has stabilized, and today we understand that if you consume more liquid , then problems will also arise.[18]
Dehydration in athletes
Athletes often lose 6-10% of body weight during exercise, which can lead to dehydration if the correct amount of fluid is not supplemented in time. Typically, the amount of 90,050 voluntarily consumed liquid is lower than than the amount of liquid consumed . [17] Already in a relatively mild form of dehydration, athletes begin to experience symptoms such as:
- Decreased performance
- Deteriorated stamina
- Increased fatigue
- Poor thermoregulation
- Application great efforts for physical activity [6] [7]
These are the reasons why hydrate the body, which also reduces stress caused by physical activity.[8] Research has shown that 90,050 novice athletes 90,051 are at 90,050 risk of dehydration 90,051 due to dramatic 90,050 increases in physical activity. [9] [10]
Effect of temperature on dehydration during sports
Numerous studies confirm that 90,050 athletes are more susceptible to dehydration if they exercise at more than 90,050 high temperatures . [11] [12] [13] In one hour of exercise, Athlete loses approximately 4 cups of fluid , depending on body weight and sweating intensity.The more intense the workout and the warmer the environment, the more fluid 9051. [5] Sports activity at high temperatures with insufficient fluid intake can have serious consequences in the long term such as:
- fever
- stroke
- heart problems
- low blood pressure
- poor blood flow to muscles [14]
Dehydration during training
If you experience dehydration symptoms described above during or at the end of your workout do the following:
- Stop exercising and rest
- Move to a cool
- Take off excess clothing
- Take sports drinks to rehydrate to replenish fluid and minerals at the same time
- Drink at least 2 liters of water over the next 2-4 hours.
- do not load the body for the next 24 hours and continue to consume enough liquid
- , in principle, you should feel better in a couple of hours, but rehydration of the body can take place within 36 hours [17]
If you want to avoid the problems caused by dehydration, you should 9050 regularly drink fluids before, during and after training and constantly throughout the day. Below we give the optimal amount of liquid.
Hydration before, during and after training
In this section, we will guide you how to properly take liquid before exercise, during exercise, and after exercise. At the same time, you will learn which drinks are good for hydration . [22]
Pre-workout fluid intake
If you are exercising at the gym, jogging, skiing or swimming, you should drink 2 glasses of liquid 2 hours before training .Half an hour before training, drink another 250 ml of water . [22] You can drink Pure Water or choose a product that will give you energy during your workout, helping to improve performance . We recommend taking a pre-workout drink like BCAA or ionic drink.
Before choosing a suitable product, , be sure to familiarize yourself with its composition. The perfect pre-workout combination is 14g carbs, 28mg potassium, and 100mg sodium per 250ml.In this case, glucose, sucrose or fructose should act as a carbohydrate, because they are quickly and easily absorbed . Please be aware that no gas is present in pre-workout drink , as this may irritate the stomach. [4]
Drinking fluids during exercise
During physical activity, try to drink from 100 to 150 ml every 15-20 minutes . This will help to maintain the required 9050 fluid level in your muscles and relieve fatigue.[4]
Suitable drinks during exercise are fortified water or amino acid drinks. To get an idea of how hydration works during workout , we have prepared a table comparing fluid intake by gender. The information in table is based on an example of a 28-year-old man and woman exercising in normal conditions. [20]
| Gender | Workout intensity | Workout time | Fluid | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Woman 168 cm 65 kg | low | 60 minutes | 700 ml | 1000 ml | |||||||
| medium | 60 minutes | 800 ml | |||||||||
| medium | 90 minutes | 1 300 ml | |||||||||
| high | 60 minutes | 1 000 ml | 90 minutes | 1 500 ml | |||||||
| Male 178 cm 85 kg | low | 60 minutes | 700 ml | ||||||||
| low | 90 minutes | 1 100 ml | |||||||||
| 60 minutes minutes | 900 ml | ||||||||||
| medium | 90 minutes | 1 300 ml | |||||||||
| high | 60 minutes | 1,000 ml | |||||||||
| high | 90 minutes | 1,600 ml |
Drinking fluids after training
If you’ve exercised for more than an hour , fruit juice diluted with water, ionic drink, or RTD drink is ideal for fluid recovery to add enough vitamins, carbohydrates, and minerals to supplement the electrolytes you consumed during exercise (sodium , potassium, magnesium).[4] If you are not satisfied with plain water try coconut water , which contains enough potassium, magnesium, calcium and phosphorus. [20]
After training , combine pure water with sports drinks to avoid hyponatremia (low sodium levels). Sodium, along with potassium and magnesium, is excreted from the body in sweat, therefore it is very important to supplement these minerals . Likewise, 90,050 people with increased sweating should get more fluids than the recommended post-workout.[20]
Often athletes create an individual hydration plan . This is a fluid intake schedule that minimizes water loss and helps maintain fluid balance. [24]
Unsuitable fluid sources before, during and after exercise
Flavored sweet waters and concentrated fruit juices are not a suitable liquid source as high sugar drinks are dehydrating.If you like plain water, drink unsweetened, non-nutritive mineral water that does not contain sugar. You can also add mint leaves, lemon or other fruit pieces to the water.
What’s your favorite drink before, during and after your workout? Do you drink sports drinks or do you prefer pure water? Leave a comment on about your drinking regimen. Share this article to let your friends and acquaintances learn more about hydration.
Sources:
[1] Nicolaidis S. Physiology of thirst. In: Arnaud MJ, editor. Hydration Throughout Life. Montrouge: John Libbey Eurotext; 1998. p. 247.– https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2
4/#R1
[2] Moreno LA, Sarria A, Popkin Bm – The nutrition transition in Spain: a European Mediterranean country. – https://www.ncbi.nlm.nih.gov/pubmed/12373620
[3] Altman P. Blood and Other Body Fluids. Washington DC: Federation of American Societies for Experimental Biology; 1961.- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2
4/#R1
[4] Kathleen M. Zelman, Drink Up for Sports and Fitness, The best beverages to help you stay hydrated – – https://www.webmd.com/fitness-exercise/features/drink-up-sports-fitness#1
[5] Carolyn J. Strange – Feel Your Best With Water – – ttps: //www.webmd. com / food-recipes / features / feel-your-best-with-water # 1
[6] Montain SJ, Coyle EF – Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise.- – https://www.ncbi.nlm.nih.gov/pubmed/1447078
[7] Cheuvront SN, Carter R, Sawka MN – Fluid balance and endurance exercise performance. – – https://www.ncbi.nlm.nih.gov/pubmed/12834575
[8] Paik IY, Jeong MH, Jin HE, Kim YI, Suh AR, Cho SY, Roh HT, Jin CH, Suh SH – FLuid replacement following dehydration reduces oxidate stress during recovery. – – https://www.ncbi.nlm.nih.gov/pubmed/19344695
[9] Bergeron MF, McKeag DB, Casa DJ, Clarkson PM, Dick RW, Eichner ER, Horswill CA, Luke AC, Mueller F , Munce A, ROberts WO, ROwland TW – Youth football: het stress and injury risk – – https: // www.ncbi.nlm.nih.gov/pubmed/16118592
[10] Godek SF, Godek JJ, Bartolozzi AR – Hydration status in college football players during consecutive days of twice-a-day preseason -– https: //www.ncbi .nlm.nih.gov / pubmed / 15827364
[11] Cheuvront SN, Carter R, Sawka MN – Fluid balance and endurance exercise performance. – – https://www.ncbi.nlm.nih.gov/pubmed/12834575
[12] Cheuvront SN, Carter R, Castellani JW, Sawka MN – Hypohydration impairs endurance exercise performance in temperate but not cold air.- – https://www.ncbi.nlm.nih.gov/pubmed/16024524
[13] Kenefick RW, Mahood NV, Hazzard MP, Quinn TJ, Castellani JW – Hypohydration effects on thermoregulation during moderate exercise in the cold. – – https://www.ncbi.nlm.nih.gov/pubmed/15045503
[14] Maughan RJ, Watson P, Shirreffs SM – Heat and cold: what does the enviroment do to the marathon runner? – https://www.ncbi.nlm.nih.gov/pubmed/17465618
[15] Culp KR, Wakefield B, Dyck MJ, Cacchione PZ, DeCrane S, Decker S.- Bioelectrical impedance analysis and other hydration parameters as risk factors for delirium in rural nursing home residents. – – https://www.ncbi.nlm.nih.gov/pubmed/15345731
[16] Lawlor PG – Delirium and dehydration: some fluid for thought? – – https://www.ncbi.nlm.nih.gov/pubmed/12353122
[17] Gastrolyte – Physical exercise: dehydration and sport – – https://gastrolyte.com.au/dehydration/dehydration-and- sport /
[18] Caster Semenya, Oscar Pistorius – Fluid intake, dehydration and exercise: Part I // History of fluid intake and conflict of interest – – https: // sport scientists.com / 2007/10 / fluid-intake-dehydration-and-exercise-part-i-history-of-fluid-intake-and-a-conflict-of-interest /? doing_wp_cron = 1543477151.44261


 g., running races, soccer matches etc.), maximize opportunities for rehydration
g., running races, soccer matches etc.), maximize opportunities for rehydration