How has the CDC changed its mask guidance. What factors influenced this decision. Who is still advised to wear masks. How should individuals decide whether to continue masking in public.
The Evolution of CDC’s Mask Recommendations
The Centers for Disease Control and Prevention (CDC) has recently updated its guidelines regarding face mask usage in public spaces. This shift marks a significant change in the approach to managing COVID-19 in the United States. The new recommendations reflect the evolving nature of the pandemic and the current state of population immunity.
Key Changes in CDC Guidance
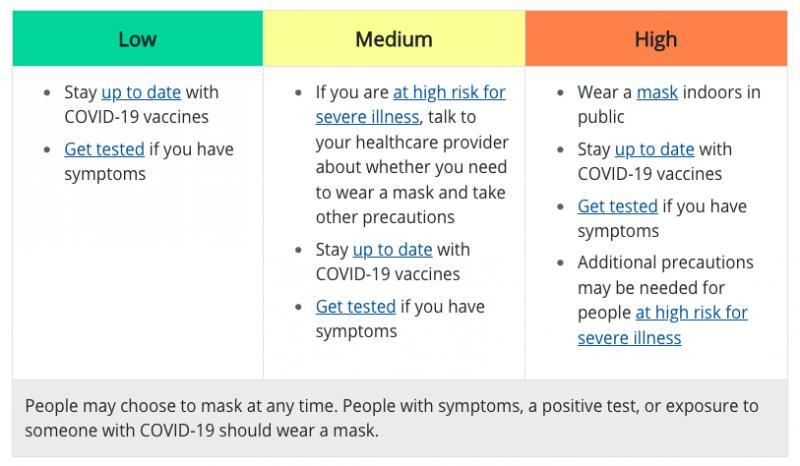
- Mask recommendations now tied to COVID-19 Community Levels
- No masks required in indoor public spaces for low Community Level areas
- Immunocompromised individuals in medium-risk areas should consult healthcare providers
- Universal indoor masking recommended only in high-risk areas
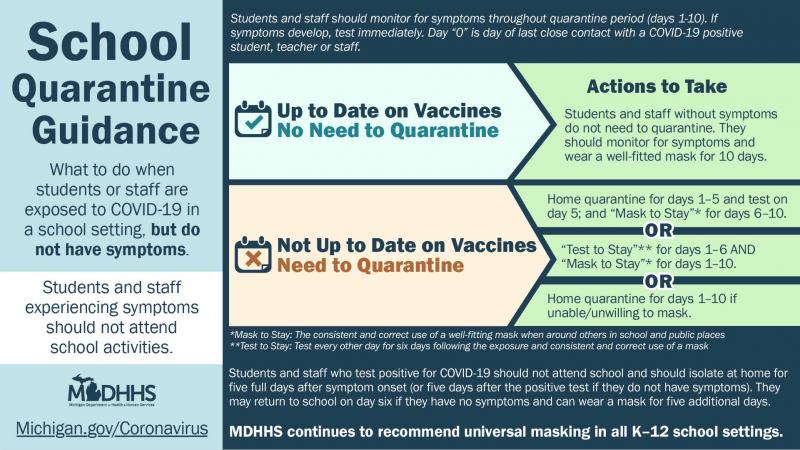
- Removal of routine screening testing recommendation in K-12 schools
- Elimination of quarantine recommendation after COVID-19 exposure
These changes represent a departure from previous blanket recommendations for indoor masking regardless of local conditions. The CDC’s new approach aims to provide more nuanced guidance based on local risk levels and individual circumstances.

Understanding COVID-19 Community Levels
The CDC’s new mask recommendations are closely tied to COVID-19 Community Levels. These levels are determined by a combination of factors, including hospitalization rates and case numbers in a given area.
How are Community Levels Determined?
- New COVID-19 hospital admissions per 100,000 population in the past 7 days
- Percent of staffed inpatient beds occupied by COVID-19 patients
- New COVID-19 cases per 100,000 population in the past 7 days
Based on these metrics, counties are classified as having low, medium, or high Community Levels. This classification system allows for more targeted recommendations that reflect the current risk in each area.
The Science Behind the CDC’s Decision
The CDC’s decision to relax mask guidelines was not made lightly. It was based on several key factors that indicate a shift in the pandemic landscape.
Population Immunity
One of the primary reasons for the change in guidance is the high level of population immunity in the United States. Over 95% of Americans aged 16 and older have some form of immunity, either through vaccination, previous infection, or both. This widespread immunity has significantly reduced the risk of severe COVID-19 for most individuals.

Availability of Treatments and Preventive Measures
The increasing availability of effective COVID-19 treatments, such as Paxlovid, has played a crucial role in the CDC’s decision. These treatments have lowered the risk of hospitalization and death for those who do contract the virus. Additionally, the widespread availability of vaccines and boosters has provided robust protection against severe outcomes.
Who Should Still Consider Wearing Masks?
While the new guidelines provide more flexibility, certain groups may still benefit from continued mask-wearing in public spaces.
- Immunocompromised individuals
- People at high risk for severe COVID-19
- Those living with or caring for vulnerable individuals
- Individuals in areas with high Community Levels
- Anyone who feels more comfortable wearing a mask
Is it necessary for everyone to continue wearing masks in all public settings? According to the new CDC guidelines, it is not. However, individuals should assess their personal risk and the Community Level in their area when making decisions about mask usage.

Navigating Personal Mask Decisions
With the relaxation of universal masking recommendations, many individuals are facing decisions about when and where to wear masks. Several factors can help guide these personal choices.
Assessing Personal Risk
How can individuals determine their personal risk level? Consider the following factors:
- Age
- Underlying health conditions
- Vaccination status
- Exposure to high-risk individuals
Those who are older, have certain health conditions, or are not fully vaccinated may have a higher risk of severe COVID-19 and may choose to continue masking in public settings.
Considering Local Conditions
Are local COVID-19 rates relevant to personal masking decisions? Absolutely. The CDC recommends checking your county’s Community Level regularly. In areas with high levels, universal indoor masking is still recommended regardless of vaccination status.
Situational Factors
Should mask usage vary based on the specific situation? Indeed, certain environments may warrant mask-wearing even in low-risk areas. These might include:
- Crowded indoor spaces
- Public transportation
- Healthcare settings
- Poorly ventilated areas
In these situations, individuals might choose to wear masks for added protection, regardless of local Community Levels.
The Impact on Public Health Measures
The CDC’s updated mask guidance represents a significant shift in public health strategy. This change raises questions about the future of COVID-19 management and the role of personal responsibility in public health.
Transition to Endemic Management
Does this change signal a move towards treating COVID-19 as endemic? Many public health experts view this shift as a step towards living with COVID-19 as a persistent but manageable disease, similar to influenza. This approach acknowledges that while COVID-19 remains a threat, the tools and knowledge we now possess allow for a more targeted response.
Emphasis on Personal Responsibility
How does this change affect individual responsibility in public health? The new guidelines place greater emphasis on personal risk assessment and decision-making. Individuals are now tasked with staying informed about local conditions and making choices based on their circumstances and risk tolerance.

Continued Importance of Vaccination
Have vaccines become less important with the new mask guidelines? On the contrary, the CDC continues to emphasize the critical role of vaccination and boosters in preventing severe COVID-19 outcomes. The relaxed mask guidelines are possible in large part due to the success of vaccination efforts.
Challenges and Criticisms of the New Guidelines
While many have welcomed the updated CDC guidelines, they have not been without criticism. Understanding these concerns provides a more comprehensive view of the situation.
Timing Concerns
Is it too soon to relax mask guidelines? Some public health experts argue that the change comes prematurely, given ongoing case numbers and the potential for new variants. They express concern that relaxed measures could lead to increased transmission, particularly among vulnerable populations.
Protection for Vulnerable Groups
How do the new guidelines affect protection for high-risk individuals? Critics point out that universal masking provided an additional layer of protection for immunocompromised individuals and those unable to be vaccinated. The shift to individual choice may leave these groups more exposed in public settings.

Variability in Implementation
Will the new guidelines be implemented consistently across different regions? The response to the CDC’s updated recommendations has varied among states and localities. Some areas continue to maintain stricter masking policies, leading to potential confusion and inconsistency in public health measures.
Looking Ahead: The Future of Mask Usage
As we navigate this new phase of the pandemic, questions arise about the long-term role of masks in public health and society.
Normalization of Situational Masking
Will mask-wearing become a common practice during respiratory illness seasons? The pandemic has increased awareness of the effectiveness of masks in preventing the spread of respiratory viruses. It’s possible that seasonal or situational mask-wearing may become more common, particularly during flu seasons or in healthcare settings.
Preparedness for Future Pandemics
How will this experience shape our response to future health crises? The lessons learned from COVID-19, including the role of masks in disease prevention, are likely to inform public health strategies for future pandemics or outbreaks.

Ongoing Research and Guidelines
Will mask guidelines continue to evolve? As our understanding of COVID-19 and other respiratory diseases grows, it’s likely that public health recommendations, including those related to mask usage, will continue to be refined based on the latest scientific evidence.
In conclusion, the CDC’s updated mask guidelines represent a significant shift in the approach to managing COVID-19 in the United States. While providing more flexibility, they also place greater responsibility on individuals to assess their risk and make informed decisions about mask usage. As we move forward, it’s crucial to stay informed about local conditions, consider personal and community risk factors, and remain adaptable as the situation continues to evolve.
CDC Relaxes Face Covering Guidelines: What Changed?
The COVID-19 pandemic has brought numerous changes to our daily lives over the past few years. One of the most visible changes has been the widespread use of face masks in public places. For much of the pandemic, the Centers for Disease Control and Prevention (CDC) recommended wearing a face covering when in public as one of several key mitigation strategies, along with social distancing, handwashing, and vaccination.
In February 2023, the CDC announced relaxed guidelines around wearing masks in public indoor spaces, citing high rates of population immunity from vaccines and prior infection as well as the availability of COVID-19 treatments and preventative tools. This represented a major shift in federal public health guidance around masks.
What exactly changed in the new guidelines?
Previously, the CDC recommended wearing a well-fitting face mask in indoor public places regardless of the COVID-19 Community Levels in the area. Their new guidance ties mask recommendations to COVID-19 Community Levels, which are based on hospitalizations and case rates.
In counties with low Community Levels, masks are no longer recommended in indoor public spaces, including schools. For areas with medium Community Levels, those who are immunocompromised or at high risk for severe disease are advised to speak with their healthcare provider about whether they need to mask. Masks are recommended indoors for everyone in areas with high Community Levels.
Additionally, the CDC no longer recommends routine screening testing in K-12 schools regardless of Community Levels. They also removed the recommendation to quarantine following exposure to COVID-19, aligning with guidance for other respiratory viruses.
Why did the CDC change their guidance now?

The CDC cited the high level of population immunity in the U.S. as one factor allowing them to relax the face covering recommendations. Over 95% of Americans ages 16 and older have some immunity through vaccination, previous infection, or both. This makes the risk of medically significant COVID-19 much lower for most people.
They also noted the increasing availability of COVID treatments, like Paxlovid, that lower the risk of hospitalization and death. Better access to preventative tools like vaccines and boosters also played a role.
The widespread availability of these vaccines, treatments, and preventative measures puts us in a different place with COVID-19 compared to earlier in the pandemic. The CDC leveraged the improved landscape to reevaluate masking guidance. However, they continue to emphasize staying up-to-date on vaccines and boosters as key prevention strategies.
How was the change received?
Response to the CDC’s relaxed guidelines has been mixed. Some public health experts and officials have praised the shift as reflecting the current state of the pandemic and the high levels of population immunity. They see it as a move toward living with COVID as an endemic virus.
However, others have argued that the change comes too soon given still elevated case counts and the possibility of new variants arising. Critics note that people who are immunocompromised or unvaccinated remain at high risk and masks protected these groups.
The response across states and localities has varied as well. While many have aligned with the new CDC guidance, some areas are still maintaining universal indoor masking policies for now. Overall, the shifts signal a new chapter in the pandemic response.
Still wearing a mask in public?: What to consider

For those wondering if they should continue masking in public following the guideline changes, there are a few key factors to consider:
- Your personal risk level – Age, underlying conditions, and vaccine status affect vulnerability.
- Local COVID-19 Community Levels – Check your county’s levels per CDC guidelines.
- Your comfort level – Some may prefer to continue masking in crowded indoor spaces.
- Situational factors – Masking may make sense on planes, buses, etc. where distancing is hard.
- Immunocompromised household or family members – Their risk may impact your choices.
While masks are no longer universally recommended, the CDC does still suggest masking if you are in an area with high transmission or if you are at high risk. And you may choose to mask in any indoor public space based on your comfort level.
As we enter this transition period, don’t be afraid to assess and reassess your own masking needs and comfort. Having high quality masks, like N95s, on hand gives you the flexibility to mask in higher risk situations as needed. Masks remain an important tool, even if no longer universally required.
The bottom line is that individuals can make informed choices about masking based on their circumstances, now that we have entered a phase of more tailored recommendations from public health authorities. While fewer people may choose to mask routinely, masks will likely remain part of our collective toolkit for managing COVID-19 risks long-term.
When Are Masks Still Recommended?
The recent changes to CDC guidelines around wearing masks in public indoor spaces have left many wondering if masks are still recommended in certain situations. While masks are no longer advised at all times in public settings for most people, there are instances where masking remains an important preventative measure.
As we enter this transition period, it’s helpful to understand where and when masking may still make sense based on your circumstances. While mask use is now more tailored, masks continue to be an important tool for protecting ourselves and others.
High COVID-19 Community Levels
Per CDC guidelines, masks are still recommended for all public indoor activities in counties with high COVID-19 Community Levels, which are based on local case rates and hospitalizations. This includes schools and workplaces. You can check your county’s level on the CDC website to determine if you live in a high transmission area where masking is still advised.
Crowded indoor spaces
Masking may make sense in crowded indoor public settings like busy grocery stores, concert venues, transportation hubs, etc. where distancing can be challenging. Masks provide protection in close proximity to others whose vaccination status may be unknown.
Immunocompromised individuals
Those who are immunocompromised or at high risk for severe illness may need to continue routine public masking based on the recommendation of their healthcare provider. Their personal risk level may still warrant extra precautions like masking.
Unvaccinated individuals
Since being unvaccinated increases vulnerability to COVID-19, those who are not up to date on vaccines are advised to mask indoors by the CDC. Masking provides protection for both unvaccinated individuals themselves and vulnerable people around them.
When feeling unwell
If you are experiencing any symptoms of respiratory illness like COVID-19, flu or common cold, wearing a high-quality mask can reduce transmission risk. Staying home when sick is ideal, but masking in public when unwell can help protect others.
Healthcare settings

Hospitals, clinics, and other healthcare facilities may still require universal masking given the higher risk of exposure and vulnerable patient populations. Follow any facility-specific guidance on masking.
Public transportation
The CDC still advises masking when using any form of public transportation, including airplanes, buses, trains, etc. where social distancing is difficult. This setting poses higher transmission risks.
Personal preference
Some people may choose to continue masking in indoor public spaces based on personal comfort level. Even healthy individuals may prefer masking for extra precaution in densely crowded indoor areas.
The bottom line is that while universal public masking is no longer recommended by the CDC, there remain many situations where wearing a mask is sensible based on health risks, setting-specific factors, and personal choice.
What kind of mask should I wear?
The CDC continues to recommend opting for the most protective, well-fitting mask possible if you choose to mask. Based on their research, here is how different masks compare in terms of protection:
- N95, KN95, KF94 respirators provide highest protection
- Surgical masks are next most protective
- Cloth masks provide least protection
N95s, KN95s or KF94s are your best choice and come with minimal discomfort. Prioritize these over surgical or cloth masks whenever feasible. Make sure any mask fits snugly against your face without gaps.
Masking tips
To get the most out of masking:
- Opt for a high-filtration respirator like N95s when possible
- Make sure mask fits tightly against your face
- Wash cloth masks or swap surgical masks daily
- Practice good hand hygiene when donning and doffing
- Avoid touching face when wearing mask
Masking is still an important tool amidst ongoing changes to COVID guidance and precautions. Understanding when and how to mask empowers us to make informed choices about protecting ourselves and vulnerable groups as the pandemic evolves.
Can Businesses Still Require Masks? What About Schools?
With the CDC relaxing public masking guidelines in February 2023, many are wondering if masks can still be mandated by certain entities like businesses and schools. The new federal guidance shifts decision-making on masking policies to state and local authorities as well as individual organizations.
While masks are no longer universally recommended in public indoor spaces by the CDC, requirements around masking in specific settings are now more nuanced. Here is how the landscape may vary for businesses and schools with the updated guidance.
Can businesses require masks?
Yes, private businesses and venues can still impose their own masking policies regardless of state or local rules. Since they operate on private property, businesses have the authority to implement COVID-19 safety protocols as they see fit, including requiring masks.
Many major retailers dropped universal mask mandates following the relaxed CDC guidelines. However, some have kept mask requirements in place for employees, while others have made masks optional for vaccinated customers and workers. Policies vary across companies.
Smaller local businesses also have flexibility here. Cafe or restaurant owners, for example, can decide to maintain a masks-required policy to protect staff and patrons at their discretion.
In short, businesses retain the right to require masking on their premises despite the rollout of new CDC recommendations. Patrons can choose whether or not to patronize businesses based on their comfort with the policies.
What about schools and childcare centers?

K-12 schools and childcare centers are able to set their own masking rules as well, in consultation with state and local authorities. The CDC no longer recommends universal indoor masking in schools at all COVID-19 Community Levels.
However, some school districts have opted to take a more cautious approach by keeping masking rules in place for now, despite the relaxed guidance. On the other hand, many districts made masks optional following the update.
Decisions around school masking policies incorporate factors like local COVID conditions, input from health departments, and parent feedback. Schools aim to balance health risks against learning considerations when setting rules.
Colleges and universities also have the flexibility to require students and staff to mask up on campus regardless of CDC guidelines. Some have maintained campus-wide mandates, while others have eased requirements.
Can states or cities override business or school masking policies?
In most cases, state or local laws and rules take precedence over organizational policies. So if your city or county mandates masks in public spaces, businesses and schools in that jurisdiction need to abide, even if their own preference is to go mask-optional.
Some states have banned universal masking mandates altogether, limiting the ability of local districts to require masks in schools against state law. Meanwhile, a few Democratic-led states have taken the opposite approach by keeping statewide school mask mandates in effect.
If businesses or schools adopt stricter mask policies than what their locality requires, they have that right as well. But they cannot go against any statewide or local masking rules and requirements.
Bottom line: the entity with the broader authority in a given area gets to make the rules on masking that organizations and individuals in that jurisdiction then need to follow.
How might policies continue to evolve?
As COVID conditions and risks change in coming months, businesses, schools, and government authorities may reevaluate their stances on masking rules. There may be shifts back and forth between mask requirements and loosened policies.
For example, a surge in infections or a dangerous new variant could prompt reconsidering masking mandates after a period of lax rules. On the other hand, reduced COVID hospitalizations might lead to easing up on existing mandates.
Individuals and families should stay updated on COVID trends in their local area and any changes to relevant masking policies. Having some masks on hand means you can quickly adapt to shifts in rules and recommendations as the situation develops.
While masks may no longer be universally required, they will likely remain part of the equation in managing COVID risks and protecting vulnerable groups. Understanding current policies empowers us to make informed choices for our health and safety.
Will There Be Pushback Against the New Guidelines?
The CDC’s recent update to its mask guidance, stating that most Americans no longer need to wear masks indoors, has been met with a mix of relief and apprehension. While many are eager to return to a maskless normal, others worry this step has come too soon. As people wrestle with how to move forward, one question looms: Will there be pushback against the new guidelines?
On the one hand, the updated guidance is a testament to how far we’ve come since the beginning of the pandemic. With high rates of vaccination and immunity, plummeting hospitalizations and deaths, and increased supplies of treatments and tests, the CDC determined the time was right to adjust its recommendations. Many find this long-overdue good news worth celebrating.
However, these changes did not come without controversy. Notably, the guidelines do not distinguish based on local infection rates, leaving many wondering if the CDC brushed aside critical nuances in its broad national policy shift. Additionally, high-risk individuals may feel left behind, as the CDC still advises them to take precautions while most move on restriction-free. With immunity waning over time and new variants on the rise, some believe loosening restrictions now is too optimistic or downright dangerous.
Implementing this policy change will likely prove messy as well. Without masks required, how can businesses and venues verify who is vaccinated or high-risk? Confusion around exceptions and variability between local policies could breed conflict. And after two years of masks, many simply feel uncomfortable abandoning them so abruptly. Adjusting from vigilance to nonchalance overnight is unlikely to come easily for some.
Ultimately, individuals and institutions must weigh their unique circumstances against the CDC’s guidance to determine their own best path forward. For many, this will likely involve continuing to mask in higher risk settings like travel and large crowds. Workplaces may need to negotiate accommodations for those desiring ongoing protections. And select localities with high transmission may choose to uphold broad indoor mandates a while longer. With immunity, treatments, and social norms all evolving, policy changes evoke mixed reactions.
While pushback against aspects of the CDC’s updated guidance seems inevitable, we must also keep perspective. This milestone reflects progress made through immense scientific innovation and public health efforts over two arduous years. With flexibility and empathy on all sides, we can move into this next phase responsibly, respecting those eager to shed masks and those needing more time to adjust. Open communication and acknowledgment of uncertainties, risks, and needs—of both individuals and communities—will be critical. If we extend grace to one another, we can continue making measured progress together.
What the coming months may hold is unclear. But with cautious optimism and care for one another, we can give this new guidance a fair chance while remaining ready to reinstate precautions if conditions call for it. This time of transition will require patience and goodwill. But by working through it as a unified community, we can keep moving forward safely.
How Do Vaccination Rates Impact the Changes?

The CDC’s updated mask guidance, which no longer recommends face coverings for most indoor settings, has sparked debate on whether loosening restrictions is prudent when vaccination rates still vary widely. How does a community’s vaccination coverage impact the risks and benefits of this policy shift?
Areas with high vaccination uptake are arguably better positioned to ease mask rules safely. Evidence shows vaccines provide strong protection against severe COVID-19 outcomes. High community coverage limits chains of transmission and reduces infection prevalence. This creates an environment where ditching masks is less likely to overwhelm hospitals or harm the vulnerable. However, no area’s rates are high enough to eradicate risk entirely.
Low vaccination areas face tougher choices. With more virus circulating, limited immunity, and strained healthcare systems, loosening restrictions could be perilous. However, doubling down on mandates risks further polarizing factions of the public health response. And ongoing masking fatigue may limit compliance anyway. There are reasonable arguments on both sides for these communities.
Vaccine equity issues also factor in. Lower rates among disadvantaged groups reflect access barriers more than hesitancy. Continued masking may unfairly burden these groups in high transmission areas. And the immunocompromised for whom vaccines underperform will face higher risk exposure in their communities regardless of broader coverage.
Layered mitigation strategies beyond just masks are worth considering too. Improving ventilation and filtration, promoting testing and treatment access, and backing vaccination with outreach and mandates can make reopening safer at any coverage level. But budgets and politics constrain solutions.
Ultimately, no single metric can dictate the “right” policy. Leaders must weigh factors like health system capacity, economic and social impacts, virus trajectory, population behaviors, emerging science, and constituent concerns when calibrating restrictions. Communities can make different responsible choices based on their circumstances.
While higher vaccination rates may enable easing measures like masking, they alone cannot determine policy. holistic assessment of local contexts, equitable supports for the disadvantaged, and flexible adaptation as conditions change will be key to navigating this transition responsibly.
Though coverage has improved, America’s vaccination story remains unfinished. This patchwork protection means impact of loosening restrictions will vary. But with coordinated efforts to keep driving immunization and smart precautions scaled to local risk, communities can progress safely toward post-pandemic life – at their own pace.
What Does This Mean for Future Pandemics?
As we navigate the winding down of COVID-19 restrictions, an important question emerges – how will this experience shape pandemic response in the future? Specifically, what might the changes around masking guidance indicate about the role of face coverings in managing future outbreaks?
On one hand, the past two years have cemented masks as a powerful public health tool. Early in the pandemic, mixed messaging caused confusion. But research has since demonstrated masks’ effectiveness at preventing transmission, especially when worn properly and combined with other measures. Having this evidence and infrastructure in place could facilitate quicker, more consistent masking recommendations when future threats arise.
However, the contentiousness surrounding masks also gives pause. A vocal minority has resisted them adamantly, fueling politicization. Widespread frustrations around mandated usage and mask fatigue have mounted over time. And enforcement has proven difficult. These experiences could make officials hesitant to recommend or require masks again, even if scientifically warranted.
Messaging around masks has also evolved. While first touted as directly protective, guidance now positions them more as a tool to reduce community spread. This nuance, along with increased availability of vaccines and treatments, could make masks a relatively deprioritized strategy moving forward.
Additionally, future pathogens may differ significantly from SARS-CoV-2. Depending on vectors, virulence, prevalence, and other factors, containment approaches like distancing or PPE use could become more or less vital. Each new threat warrants tailoring strategies to its unique profile.
In essence, while COVID-19 underscored masks’ benefits, it also revealed numerous challenges. How these lessons balance out will determine if and when masking once again becomes a frontline response. Officials may promote early, consistent usage in future pandemics. Or they may pursue other control measures first to preserve public willingness and leverage emerging innovations. Most likely, context-specific determinations will guide strategy.
As with every aspect of pandemic response, we must let science and circumstances, not politics or inflexible thinking, guide future decisions. This crisis provided hard-won lessons, but each new threat differs. With safety as the priority, our policies must evolve as new challenges arise.
Why Did It Take So Long for the CDC to Relax Guidelines?

After two years of nearly universal indoor masking, the CDC’s lifting of face covering recommendations for most Americans in February 2022 came as a watershed moment. Yet it also prompted the question – with cases and hospitalizations plummeting for weeks, why did it take so long for the CDC to relax guidelines?
Shifting public health policy requires balancing act of factors, and in a crisis like COVID-19, erring on the side of caution. As critics charged the CDC reacted too slowly, defenders cited their duty to wait for overwhelming data before acting. Gradualism provided time to monitor trends after each Omicron surge, analyze wider impacts of loosening restrictions elsewhere, and develop contingency plans should conditions worsen again.
Scientific uncertainties have likewise abounded, especially around new variants. Questions around how much protection prior infections confer, the durability of vaccine effectiveness, and the population’s remaining susceptibility levels demanded careful study before easing mandates. And modeling projected trajectories for when hospital capacity could withstand another case rise without being overwhelmed.
Beyond science, implementation challenges necessitated patience. Clear communication around nuanced guidance took time to develop. Schools and businesses needed warning to prepare revised policies. Vulnerable groups required access to medical masks and tests to manage their own risk. And backing any guidance shift with further vaccination outreach was vital.
Polling also made clear that public opinion remained divided on masking’s necessity. Dropping mandates immediately could have undermined compliance among those still favoring precautions. Gradual relaxation based on local data allowed people time to get comfortable with additional risk as norms evolved.
In retrospect, the CDC may have slow-walked certain policies like post-exposure quarantines. But regarding masks, their cautious approach balanced prudence and optimism responsibly. Moving deliberately based on data prevented whiplash in guidance. And it built public trust – no small feat after years of mixed messaging.
While many grew understandably impatient, the CDC’s commitment to evidence-based guidance has proven critical. We cannot forget hard lessons about disregarding science for haste. Through steady progress rooted in facts, we will reach the end of this crisis safely.
Do Masks Still Help Slow the Spread of COVID-19?

With masking requirements easing, it’s natural to ask – are face coverings still a worthwhile COVID-19 precaution for those concerned about transmission, or have they outlived their usefulness? According to experts, masks do continue reducing viral spread and remain an important tool, though guidelines are shifting.
It’s true masks play a lesser role with high vaccination rates, immunity from prior infections, and the Omicron variant causing less severe disease overall. Plus, pandemic fatigue has diminished tolerance for ongoing mandates. Still, strong evidence confirms masks’ ability to contain airborne droplets and aerosols, blocking infected wearers from spreading virus and protecting others nearby.
Mask quality matters greatly. Tight-fitting respirators like N95s offer far more protection than loose-fitting cloth masks, both for the wearer and those sharing indoor air. Promoting affordable access to high-filtration masks for vulnerable groups could enable safer eased restrictions.
Additionally, prevalence varies by community. Masks make more impact where circulation remains higher, especially heading into future waves. Targeted regional or situational masking policies may be warranted even as universal mandates lift.
For individuals, factors like personal risk tolerance, proximity to crowds, and local transmission levels help determine if voluntarily masking remains prudent. And respecting businesses or events implementing ongoing mask rules, which offer options for the still-cautious, builds goodwill in this transitional period.
However, we cannot ignore that overbearing requirements have diminished public trust and exhausted patience. Hence the emphasis is now on personal choice and targeted policies for higher-risk spaces. Preserving individual autonomy boosts compliance where masks can still curb spread.
In short, masks absolutely still slow viral transmission through this pandemic’s twilight stages, even if mandates are lifting. By continuing to offer free, quality respirators to vulnerable groups, provide evidence-based guidance, and encourage situational masking where risk is higher, we sustain an important layer of protection without alienation.
Wearing high-filtration masks around those at risk, in crowded indoor settings, or when local transmission is elevated remains an act of public health and compassion. As we transition out of this crisis, voluntary masking to protect others, along with vaccines and treatments, will ease our path towards safely resuming normal life.
Will People Feel Pressured to Remove Masks Too Soon?
The CDC’s updated guidance on mask wearing has left many feeling confused. While vaccinated individuals can now safely go without masks in most settings, some worry this new advice may lead to undue social pressure to remove masks prematurely.
This burst of perplexity stems from the nuanced nature of the CDC’s recommendation. Vaccines provide excellent protection against COVID-19, leading the CDC to relax guidelines for vaccinated people. However, with only around 35% of Americans fully vaccinated, many are not yet protected. So how can we tell who needs to keep masking?
The CDC faces a communication conundrum. Their guidance aims to reward vaccinated people by giving them permission to unmask. But broadcasting this message may unintentionally pressure unvaccinated people to go maskless too. With vaccination status invisible, it could spawn situations where unmasked people are assumed protected – even if they’re not.
Some see this policy as an incentive to get vaccinated. But others worry it’s unfair to those who remain unvaccinated for legitimate reasons. Children under 12 still can’t get vaccinated, and some adults have medical conditions preventing vaccination.
Rather than liberation, these groups may feel singled out and stigmatized for ongoing mask use. And service workers may face backlash when trying to enforce business mask mandates.
So how can we thoughtfully unwind mask wearing without ostracizing the unvaccinated? Some suggest we should keep masking in crowded public settings, regardless of vaccine status. This shows solidarity with those who remain unprotected, avoiding singling any group out.
Others argue this is unfair to the vaccinated, delaying their return to normalcy. Some believe we should respect individual choice: Those uncomfortable with the risk can choose to keep their masks, while vaccinated people can unmask. Of course, this relies on the social graciousness to accept those still masking without judgment.
There are no easy solutions. The CDC based their guidelines on the scientific evidence that vaccines drastically reduce transmission risks. But applying blanket policy to a diverse population fraught with mistrust was always going to be tricky. Still, we should avoid vilifying unmasked vaccinated people as selfish or reckless. For most, going mask-free is just the CDC-sanctioned reward for getting their shots.
Perhaps a little grace on all sides would go a long way. We could focus less on judging others’ choices and more on controlling our own actions. Get vaccinated if you’re able, but respect those who keep masking. Wear a mask yourself in crowded areas if it makes you more comfortable, without assuming the worst of those who don’t. Amidst confusing policies and agitated passions, remembering compassion may be our best path forward.
How Will This Impact Immunocompromised Individuals?

The CDC’s updated masking guidance has sparked concerns about how it will affect immunocompromised people. This group remains at high risk for COVID-19, even after vaccination. So for them, ongoing masking is critical protection.
Those with compromised immune systems don’t produce as robust responses to vaccines. Data shows they’re less likely to develop protective antibodies after vaccination compared to healthy people. This means vaccines provide less shielding for these vulnerable individuals.
So while the CDC now says vaccinated folks can safely unmask, this blanket guidance doesn’t really apply to the immunocompromised. They still need to mask up for self-protection, even after getting their shots.
But with masking guidelines now relaxed, some worry immunocompromised people will face pressure to unmask before it’s safe. Masks have become a social cue signaling vaccination status. The prevailing attitude may shift to “no mask = vaccinated”, even though this isn’t true for all.
Immunocompromised people shouldn’t have to out themselves as high risk just to justify wearing a mask. But if they keep masking while others shed masks, it could raise questions. Rather than liberation, they may feel marked as abnormal or assume greater exposure risks.
There are also concerns around equity and access. Lower vaccination rates among disadvantaged groups means they’ll remain higher risk. Yet their jobs may not permit masking if everyone else sheds masks. This could force invidious choices between health and livelihood.
So how can we support ongoing masking for those who need it? Some propose keeping mandates in critical areas like healthcare, transit and schools. Others believe public education can foster acceptance of mask wearers post-mandates.
But any policy should balance freedoms for the protected against protections for the vulnerable. There are no perfect solutions, but we must acknowledge trade-offs.
Perhaps the best approach is compassion. As we unzip our masks, don’t assume others have the same freedoms. Immunocompromised people don’t cease to exist just because the mandates ended. Make space for those who need to keep masking without stigma or judgment. Amidst our eagerness to unwind restrictions, caring for the vulnerable remains vital.
Do Masks Provide Any Continued Benefits Besides COVID-19?

With COVID-19 restrictions unwinding, you may be eager to shed your mask. But before stashing them away, consider the other benefits masks can provide even beyond the pandemic.
The main purpose of masking is reducing respiratory droplet spread, curbing COVID transmission. But masks can also filter out other airborne irritants. This helps limit exposure to pollutants, allergens, and even common colds and flu.
Research shows places mandating masks saw a dramatic decline in seasonal flu rates over the past year. Masking created a barrier against flu virus particles, demonstrating the wider protective effects masks offer.
So for those susceptible to illness, wearing a mask in crowded indoor settings may still prove useful post-pandemic. Masks provide a simple way to reduce risks from communicable diseases, especially amidst flu season or localized outbreaks.
Beyond infection control, masks could offer some continued benefits:
- Reduced seasonal allergy symptoms when worn outdoors due to filtering airborne pollen
- Less exposure to air pollution when commuting or traveling through high traffic areas
- An added barrier against smoke, dust, or chemical irritants
- Privacy and reduction of facial recognition ability
However, potential downsides like discomfort, muffled speech, and barriers to communication mean most people are unlikely to mask indefinitely without a compelling reason.
But masks still offer useful versatility in specific circumstances. Wearing one when feeling ill prevents spreading germs to others. Those facing significant health risks may choose ongoing masking for self-protection. And masking could provide insurance against future outbreaks of new viruses.
So while we may happily shed masks in lower risk everyday contexts, it’s helpful to remember the wider benefits they can provide. Adding masks to your personal toolkit gives you options to whip one out when it could prove useful beyond just COVID-19.
How Did Other Countries Handle Mask Requirements During the Pandemic?
As the CDC relaxes mask guidance, it’s interesting to look at how other countries approached masks throughout the pandemic. Policies varied globally, providing real-world data on the impacts of different masking strategies.
Some East Asian countries like China, Japan, and South Korea mandated masks early on. Citizens were accustomed to masking during flu season, making adoption smooth. This likely slowed viral spread and helped them avoid the drastic lockdowns seen elsewhere.
In Europe, mask rules fragmented across borders. Spain mandated masks nationally in mid-2020. Germany required them on transit and in shops. The UK didn’t mandate masks until mid-2021. Differing policies caused confusion across Europe’s open borders.
The Africa CDC pushed widespread masking early in the pandemic. Rwanda was the first Sub-Saharan country mandating masks in 2020. Mask supply issues hampered adoption in poorer regions, but cultural norms made masks more accepted than in the West.
Here in the US, masking was politicized from the start. With the CDC flip-flopping early advice, states enacted a hodgepodge of policies. Mandates emerged slowly throughout 2020, becoming widespread only after dire winter surges.
In Canada, masks were initially recommended rather than required. But by late 2020, masks were mandated in public indoor spaces across most provinces. Compliance proved relatively high despite lack of strong enforcement.
In Latin America, masks were mandated broadly. But deep poverty made access difficult, especially for rural populations. Noncompliance also remained an issue where tight enforcement proved impossible.
Globally, early and consistent messaging proved most effective at normalizing masking. But adoption varied across different cultural attitudes, access issues, political climates, and enforcement capacities.
As mandates unwind, we’ll have to watch how masking behaviors persist voluntarily. But the pandemic provided insight on how to promote public health behaviors going forward, even beyond COVID-19.
What If COVID-19 Cases Start Rising Again? Could Masks Return?

After over a year with masks, it feels liberating to finally cast them off! But what if this COVID respite doesn’t last? If cases rise again, some wonder whether masks could make a comeback.
There are reasons to be cautiously optimistic that mask mandates are subsiding for good. Cases have plunged as vaccines rollout. And summer’s arrival curbs seasonal spread. This one-two punch makes it unlikely we’ll see a major surge anytime soon.
But the pandemic’s twists and turns taught us nothing is guaranteed. New variants could evade vaccines or weather dampen seasonal effects. If transmission reignites, updated mask guidance isn’t off the table.
The CDC has pledged to base all policies on the data and science. If these pointed to rising risks again, masking would likely be back on the menu. But rather than widespread mandates, local requirements may be more targeted.
For example, if an aggressive new variant emerged in a specific region, area-specific masking could contain spread. Schools could require masks if pediatric cases spiked before kids can vaccinate. Or masks could be advised in crowded indoor spaces like concerts if outbreaks festered there.
Targeted interventions boost protection where it’s needed most without overburdening lower-risk contexts. So masks aren’t all or nothing; policies can deploy them strategically based on local conditions.
But after the whiplash and fatigue of shifting policies, governments may hesitate to yo-yo mask rules again. Messaging would need to clearly explain any backtracking to maintain public trust and cooperation.
And some worry masks risks becoming political kryptonite if mandates return after being lifted. Those celebrating mask freedom may not tolerate their return gracefully.
Still, public health remains the top priority if circumstances deteriorate. Hopefully vaccines and seasonality can suppress COVID long term. But if we need masks to control spread once more, health authorities will put science first, politics aside.
For now, let’s bask in our mask liberation! But stay ready to grab masks as needed if COVID’s crafty twists write future plot points we didn’t see coming.
How Can You Determine If It’s Safe to Go Maskless in Your Area?

The CDC’s new masking guidance allows vaccinated people to ditch masks in most settings. But how can you gauge if conditions are ripe to go maskless where you live?
The first consideration is your personal vaccination status. If you’re fully vaccinated, your individual risk is low. But what about community-level risk? Here are some tips for assessing local transmission:
- Track COVID case rates and test positivity percentages in your county. Consistently low and declining numbers signal safer conditions.
- Check whether there are any local outbreaks or new concerning variants emerging. Targeted hotspots may warrant continued precautions.
- Note if your area has high vaccination rates. Higher community coverage offers protection through herd immunity.
- See if local healthcare facilities are still overwhelmed by COVID cases. Strained hospitals indicate ongoing elevated risk.
Also evaluate the location you’ll be in. Outdoor or well-ventilated spaces are safer than crowded indoor venues. Distancing is still wise in packed settings.
Policies offer clues too. Areas discontinuing school and business mask mandates signal officials deem conditions now lower risk.
Of course, your personal risk tolerance also matters. If you’re immunocompromised or live with vulnerable people, you may opt for continued caution regardless of vaccination status or local case rates.
In the end, while masking guidance has changed, sound judgment still applies. Track local data trends, assess your situation, and make thoughtful decisions. With prudence and compassion, we can collectively move forward safely.
What Other Steps Can You Take to Protect Yourself If Not Wearing a Mask?
Shedding your mask feels liberating, but how else can you stay safe if going maskless? Here are some tips:
- Get vaccinated and boosted. Vaccines provide powerful protection against COVID-19.
- Distance yourself in crowded spaces. Six feet of space still lowers risk.
- Opt for outdoor activities over indoor when possible. Open air disperses droplets.
- Avoid high-risk venues like packed bars or large concerts. Close crowds raise chances of spread.
- Increase ventilation indoors by opening windows. Good airflow dilutes viral particles.
- Practice good respiratory etiquette by covering coughs and sneezes.
- Consider wearing a mask if feeling any symptoms to avoid infecting others.
- Carry a mask to use situationally, like on transit or at the doctor’s office if they require it.
- Monitor your local COVID trends and adjust activities accordingly if cases spike.
Transitioning to a masks-optional reality calls for continued vigilance. While vaccination protects well against severe disease, mild breakthrough infections remain possible.
Using layered precautions provides the best safeguarding without needing masks constantly. Get shots, keep your distance, choose outdoor over indoor, avoid crowds, and stay home if feeling ill.
With thoughtfulness and compassion for those still facing elevated risks, we can collectively move forward in this new phase – even without masks.

