How do small digital thermometers work. What are the different types of digital thermometers available. When should you use a small digital thermometer. What is the proper technique for taking temperature readings. What are normal temperature ranges for different body locations. How can you ensure the most accurate readings with a digital thermometer. What are special considerations for checking a baby or child’s temperature.
The Science Behind Small Digital Thermometers
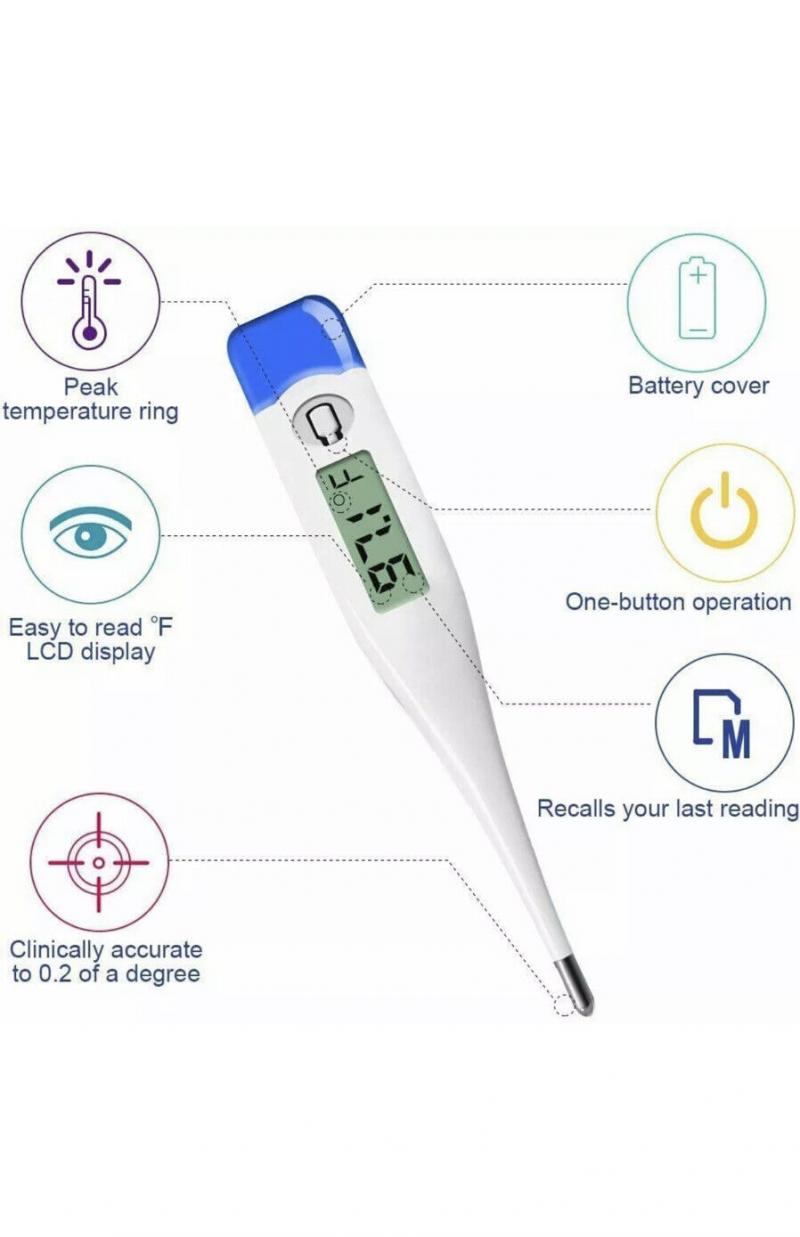
Small digital thermometers have revolutionized the way we monitor body temperature. These compact devices utilize a thermistor, a type of resistor sensitive to temperature changes, to provide quick and accurate readings. But how exactly do they work?
At the heart of a digital thermometer is a tiny circuit board that applies voltage across the thermistor. As the temperature changes, so does the thermistor’s resistance, affecting the current flow. The thermometer’s microchip then interprets this data to determine the temperature.

Most small digital thermometers are designed for oral, rectal, or underarm use. When placed in these bodily locations, the thermistor at the tip senses the surrounding temperature and relays the information to the digital display.
Advantages of Digital Thermometers
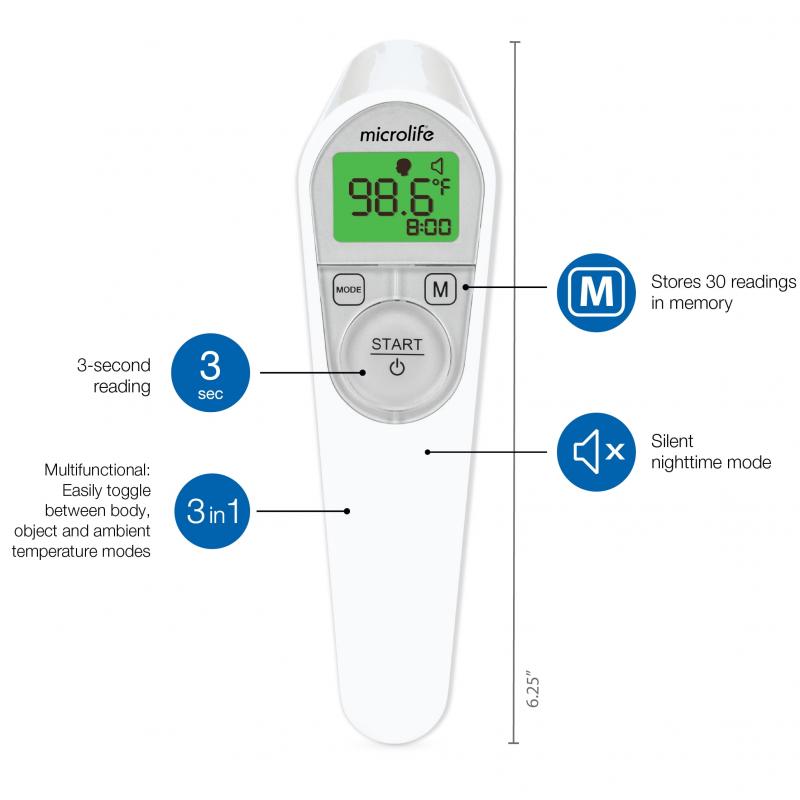
- Rapid results – typically within seconds
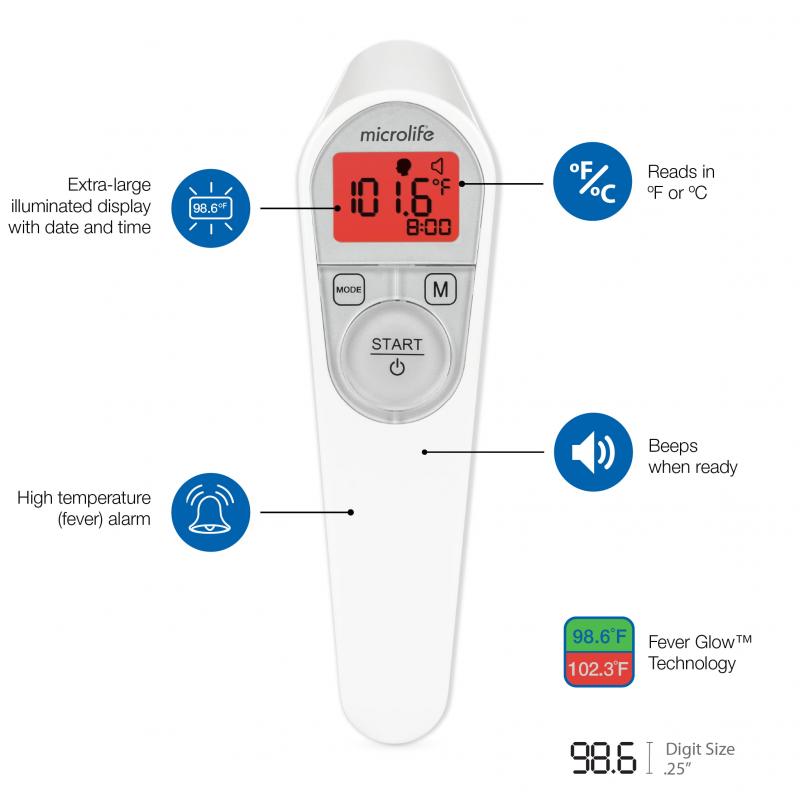
- Easy-to-read digital display
- Silent operation for undisturbed measurements
- Compact and portable design
- Enhanced safety due to absence of glass or mercury
- Memory function to store past readings
- Some models offer flexible or bendable designs
Exploring the Various Types of Small Digital Thermometers
The world of small digital thermometers has expanded beyond traditional oral and rectal models. Today, there’s a wide array of specialized thermometers designed for different body locations and specific needs.
Innovative Thermometer Designs
- Forehead thermometers: These use infrared technology to measure the temperature of the temporal artery.
- Ear thermometers: Equipped with an infrared sensor to read the tympanic membrane temperature.
- Pacifier thermometers: Ideal for infants, these take temperature readings from a baby’s mouth.
- Armpit thermometers: Specially designed for underarm temperature measurements.
- Finger thermometers: These compact devices measure temperature from the fingertip.
Each type of thermometer has its unique advantages and may be more suitable for certain situations or age groups. For instance, ear thermometers are often preferred for older children, while pacifier thermometers can be a godsend for fussy infants.
When to Reach for Your Digital Thermometer
Understanding when to use a small digital thermometer is crucial for monitoring health and detecting potential illnesses early. But what are the key indicators that warrant a temperature check?
It’s advisable to take temperature readings in the following situations:
- When experiencing symptoms like feeling warm, flushed, chilled, or sweaty
- In case of a sore throat or persistent coughing
- When experiencing body aches, chills, and other flu-like symptoms
- After a seizure episode
- For ongoing monitoring of a chronic condition
- When a baby appears fussy or unwell
Regular temperature monitoring can provide early warning signs of infection or other health issues. It’s an essential tool in your home healthcare arsenal, helping you make informed decisions about when to seek medical attention.
Mastering the Art of Accurate Temperature Measurement
Taking an accurate temperature reading isn’t just about having the right equipment – it’s also about using the proper technique. How can you ensure you’re getting the most precise measurements with your small digital thermometer?
Steps for Proper Temperature Taking
- Familiarize yourself with the instructions specific to your thermometer model.
- Clean the thermometer tip thoroughly before and after each use.
- For oral temperatures, wait 15-20 minutes after eating or drinking to avoid skewed results.
- When using orally, place the thermometer tip under the tongue towards the back of the mouth.
- Remain still with your mouth closed while the thermometer is sensing the temperature.
- Wait for the beep or signal indicating the reading is complete.
- Record the temperature reading along with the date and time for future reference.
By following these steps, you can significantly improve the accuracy of your temperature readings, providing more reliable information about your health status.
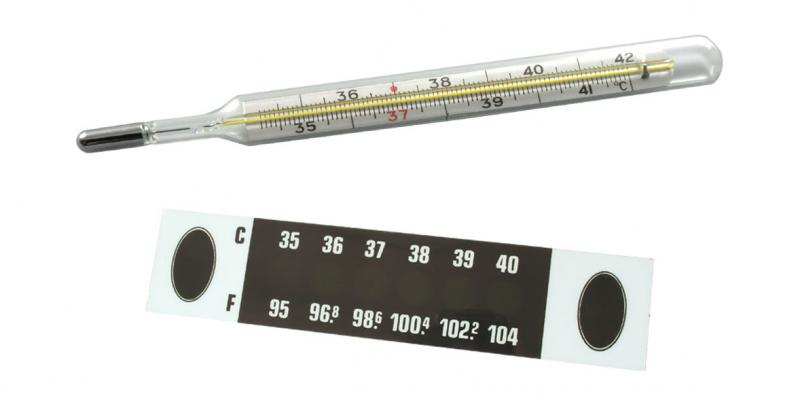
Understanding Normal Temperature Ranges
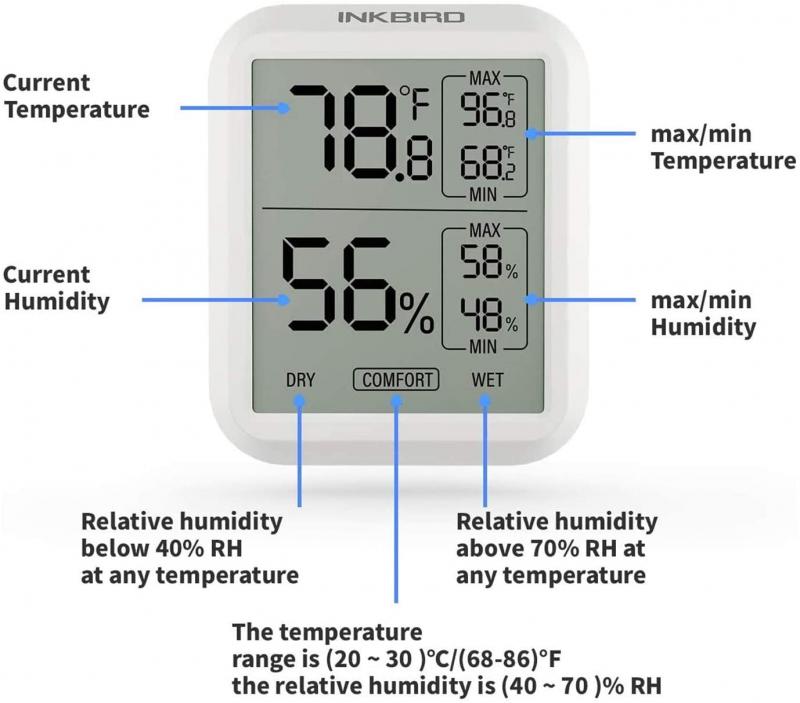
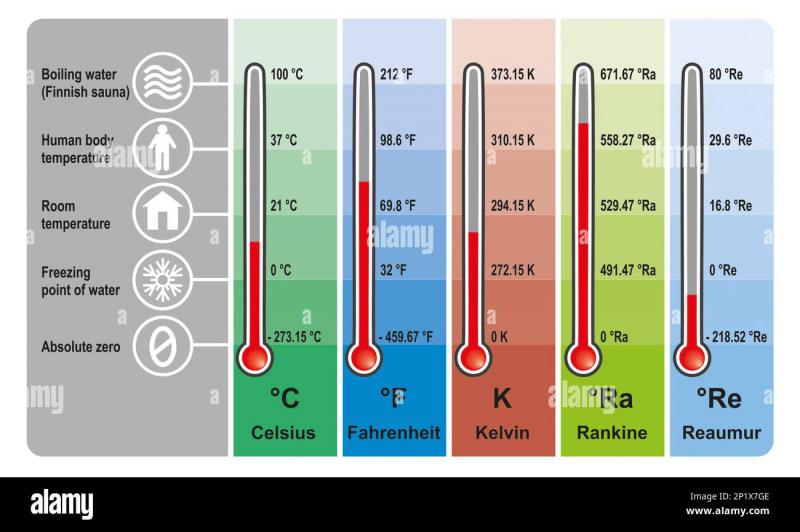
While 98.6°F (37°C) is often cited as the “normal” body temperature, the reality is more nuanced. Normal temperature can vary based on factors such as the individual, time of day, and the method of measurement.

Temperature Ranges by Measurement Method
- Oral: 97.8°F – 99°F (36.5°C – 37.2°C)
- Underarm: 97.5°F – 99°F (36.4°C – 37.2°C)
- Rectal: 99.6°F – 100.4°F (37.5°C – 38°C)
- Ear: 97.5°F – 99.5°F (36.4°C – 37.5°C)
Is a temperature outside these ranges always cause for concern? Not necessarily. Individual variations and other factors can influence your temperature. However, consistent readings outside these ranges, especially when accompanied by other symptoms, may warrant medical attention.
Recognizing Signs of a Fever
A fever is generally defined as a temperature over 100.4°F (38°C). Key indicators of a fever include:
- Feeling unusually warm or experiencing chills
- Flushed skin
- Excessive sweating
- Shivering
- Warm, dry skin
- Decreased energy and appetite
- Body aches and pains
Any fever over 104°F or lasting more than a few days warrants immediate medical attention. Remember, fever is often a sign that your body is fighting an infection, but persistent high temperatures can be dangerous.
Ensuring Accuracy: Tips and Tricks for Digital Thermometer Use
While small digital thermometers are generally accurate, several factors can influence their readings. How can you maximize the accuracy of your temperature measurements?

Factors Affecting Thermometer Accuracy
- Placement: Oral and rectal readings tend to be more accurate than ear or forehead measurements.
- Consistency: Taking multiple readings can help confirm the accuracy of the result.
- User error: Not following instructions properly can lead to inaccurate readings.
- Environmental factors: Ambient temperature can impact the thermometer’s performance.
- Calibration: Over time, a thermometer’s accuracy may decline, necessitating recalibration or replacement.
Best Practices for Accurate Readings
- Use oral mode for the highest accuracy when possible.
- Take three readings spaced apart and calculate the average.
- Use disposable probe covers if available to maintain hygiene and consistency.
- Allow sufficient time for the thermometer to equilibrate in its measurement location.
- Periodically compare your digital thermometer’s readings with those of a traditional glass thermometer.
- Replace the battery regularly to ensure optimal performance.
By following these guidelines, you can significantly enhance the reliability of your temperature measurements, providing more accurate information for health monitoring and decision-making.

Special Considerations for Measuring Children’s Temperatures
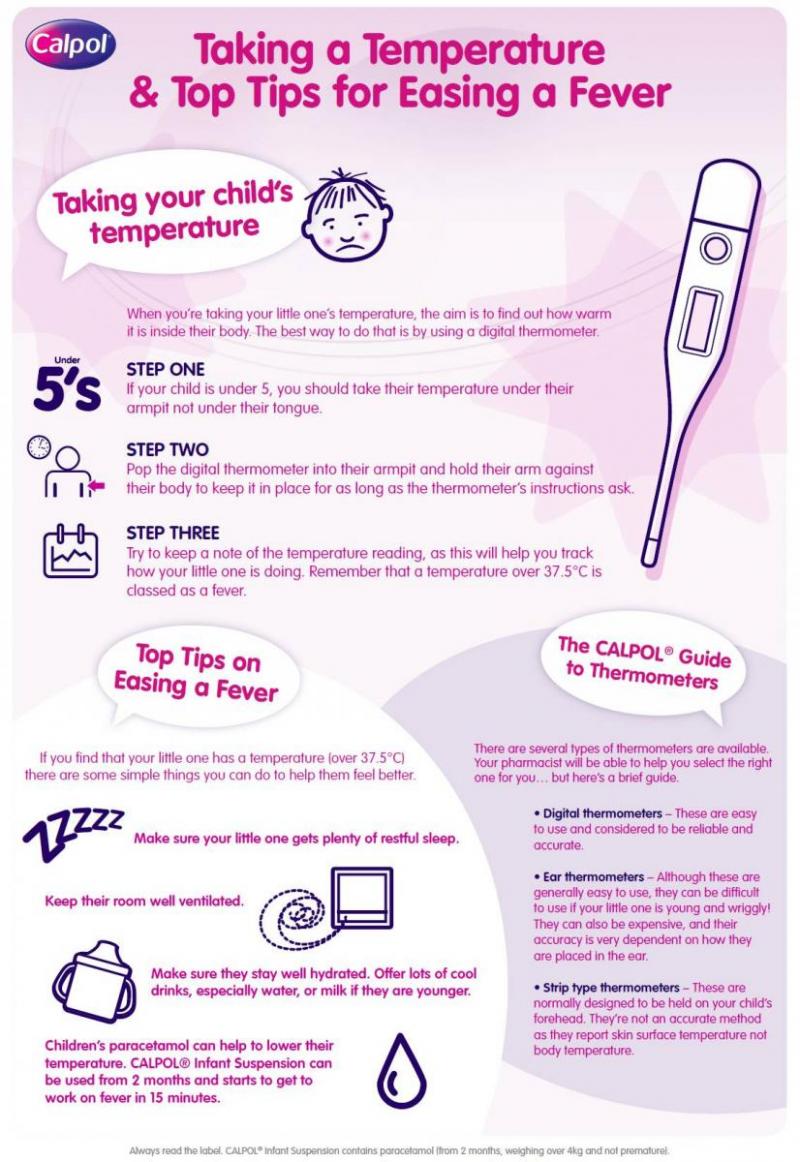
Taking a temperature reading from a child, especially an infant or toddler, can present unique challenges. How can you ensure accurate readings while keeping the child comfortable and cooperative?
Strategies for Temperature Taking in Children
- Use distraction techniques such as toys, books, or singing to keep the child calm and still.
- Apply a small amount of petroleum jelly to aid probe insertion for rectal temperatures.
- For infants, rectal temperature is often the most accurate method. Gently insert the probe only 1/4 to 1/2 inch.
- Consider using a pacifier thermometer for babies who readily accept pacifiers.
- For older children, ear or forehead thermometers can be less invasive and more comfortable.
Is there a best time to take a child’s temperature? Ideally, choose a time when the child is calm and hasn’t recently been active or consumed hot or cold foods or drinks. Early morning or late evening often work well for baseline readings.

Age-Specific Temperature Taking Methods
Different age groups may require different approaches to temperature taking:
- Newborns to 3 months: Rectal temperature is recommended for highest accuracy.
- 3 months to 3 years: Rectal temperature is still preferred, but armpit temperature can be a good alternative.
- 4 years and older: Oral temperature becomes a viable option, along with ear or forehead readings.
Remember, regardless of the method used, it’s crucial to follow the manufacturer’s instructions for your specific thermometer model to ensure the most accurate results.
Interpreting Temperature Readings: When to Seek Medical Attention
While having a small digital thermometer at home is invaluable for monitoring health, it’s equally important to know how to interpret the readings. When does a temperature reading indicate a need for medical attention?
Temperature Thresholds by Age
- 0-3 months: Any temperature of 100.4°F (38°C) or higher requires immediate medical attention.
- 3-6 months: A temperature above 102°F (38.9°C) warrants a call to the doctor.
- 6 months and older: A temperature higher than 102°F (38.9°C) that persists for more than a day should be evaluated by a healthcare provider.
Is fever always a cause for concern? Not necessarily. Fever is often a sign that the body is fighting off an infection. However, very high fevers or those accompanied by other concerning symptoms should be evaluated by a medical professional.

Additional Signs That Warrant Medical Attention
Beyond just temperature, look out for these symptoms that may indicate a need for medical evaluation:
- Severe headache or neck stiffness
- Persistent vomiting or diarrhea
- Difficulty breathing or chest pain
- Unusual skin rash, especially if it doesn’t blanch when pressed
- Signs of dehydration such as decreased urination or dry mouth
- Extreme lethargy or difficulty waking
- Seizures or convulsions
Remember, these guidelines are general. Trust your instincts – if you’re concerned about your or your child’s health, don’t hesitate to seek medical advice.
Maintaining Your Digital Thermometer: Care and Storage Tips
Proper care and storage of your small digital thermometer not only extends its lifespan but also ensures continued accuracy in readings. How can you best maintain your thermometer?
Essential Thermometer Care Tips
- Clean the thermometer before and after each use with alcohol or soap and lukewarm water.
- Store the thermometer in its protective case when not in use.
- Keep the thermometer away from extreme temperatures and direct sunlight.
- Check the battery regularly and replace when necessary.
- Calibrate your thermometer annually or as recommended by the manufacturer.
How long can you expect a digital thermometer to last? With proper care, most quality digital thermometers can last for several years. However, if you notice inconsistent readings or other signs of malfunction, it’s time to replace the device.
Signs Your Thermometer Needs Replacement
- Inconsistent or clearly inaccurate readings
- Slow response time
- Difficulty turning on or off
- Faded or malfunctioning display
- Visible damage to the probe or body of the thermometer
By following these care guidelines and staying alert to signs of wear and tear, you can ensure your digital thermometer remains a reliable tool in your home health kit for years to come.
Small digital thermometers have become increasingly popular in recent years due to their convenience and ease of use. But how exactly do these little devices work, and what are the best practices for taking accurate temperature readings with them? Let’s take a closer look.
How Small Digital Thermometers Work
Small digital thermometers use a thermistor to measure temperature. A thermistor is a type of resistor that changes its resistance with temperature. Within the thermometer is a tiny circuit board that applies a voltage across the thermistor and measures the resulting current flow. Based on the resistance of the thermistor, the microchip in the thermometer can determine the temperature.
Most small digital thermometers are designed for oral, rectal, or underarm use. When placed properly in one of these bodily locations, the thermistor at the tip of the thermometer senses the surrounding temperature and relays the information back to the digital display.
Types of Small Thermometers

In addition to traditional oral and rectal models, small digital thermometers are now available with special features and for different body locations:
- Forehead thermometers use an infrared scanner to measure the temperature of the temporal artery.
- Ear thermometers have an infrared sensor that reads the tympanic membrane temperature.
- Pacifier thermometers take temperature from a baby’s mouth.
- Armpit thermometers work best under the arm.
- Finger thermometers measure temperature from the fingertip.
Benefits of Using a Small Thermometer
Compared to old-fashioned glass thermometers with mercury, small digital thermometers offer many benefits:
- Results in seconds – no waiting for minutes.
- Easy to read digital display.
- Silent operation.
- Small and compact size.
- Safety – no glass or mercury.
- Can store past temperature readings.
- Some are flexible or “bendable”.
When to Use a Small Thermometer

Small digital thermometers are useful for monitoring potential fever and illness. It’s recommended to take temperature readings when:
- Feeling warm, flushed, chilled, or sweaty
- Sore throat or coughing
- Aches, chills, and other flu symptoms
- After a seizure
- Monitoring a chronic condition
- A baby seems fussy or sick
Routine temperature taking can give early warning of infection or other issues.
How to Properly Take a Temperature
For the most accurate reading, proper technique is important when using a small digital thermometer:
- Read the instructions for proper use of your thermometer model.
- Clean the thermometer tip before and after each use.
- Wait 15-20 minutes after eating or drinking before taking an oral temperature.
- Place correctly under tongue towards the back for oral use.
- Keep still with mouth closed while thermometer is sensing.
- Wait for the beep or other signal that reading is complete.
- Record your temperature reading with date/time for reference.
Normal Temperature Ranges
Normal oral temperature is approximately 98.6°F (37°C). However normal can vary by person, time of day, and measurement method. Here are general guidelines:
- Oral: 97.8°F – 99°F (36.5°C – 37.2°C)
- Underarm: 97.5°F – 99°F (36.4°C – 37.2°C)
- Rectal: 99.6°F – 100.4°F (37.5°C – 38°C)
- Ear: 97.5°F – 99.5°F (36.4°C – 37.5°C)
Signs of a Fever
A fever is generally defined as a temperature over 100.4°F (38°C). Some key signs of a fever include:
- Feeling excessively warm or chilled
- Flushed skin
- Sweating
- Shivering
- Warm, dry skin
- Lack of energy and appetite
- Aches and pains
See a doctor for any fever over 104°F, or that lasts more than a few days.
How Accurate Are Small Thermometers?
Most quality small digital thermometers are accurate to within ±0.2°F (±0.1°C) with proper technique. However, many factors can affect accuracy:
- Placement – Oral and rectal readings are more accurate than ear or forehead.
- Consistency – Take multiple readings for confirmation.
- User error – Not following instructions.
- Environment – Ambient temperature can impact readings.
- Calibration – Accuracy declines over time.
Tips for Getting an Accurate Reading

Follow these tips for the most precise temperature measurement:
- Use oral mode for highest accuracy.
- Take 3 readings spaced apart and average.
- Use disposable probe covers if available.
- Allow proper time under the tongue or in other location.
- Compare to “old-fashioned” glass thermometer periodically.
- Replace battery regularly.
Checking a Baby or Child’s Temperature
It can be challenging to take an accurate temperature reading on a squirming, fussy child. Here are some pointers:
- Distract with toys, books, or singing.
- Add a little petroleum jelly to aid probe slippage.
- Do rectal temperature for infants – gently insert only 1/4 to 1/2 inch.
- Pacifier thermometers work well when a baby is sucking.
- Underarm is OK if child is staying still.
- Use forehead mode if child resists other methods.
Taking Your Temperature Orally

For adults and older children, oral temperature is generally most accurate. Follow these steps:
- Wait 15-20 minutes after eating or drinking.
- Turn on thermometer and place probe under tongue towards back of mouth.
- Close mouth and breathe through nose.
- Hold in place until thermometer beeps – usually 10 seconds.
- Remove and read display.
- Clean probe before and after use.
Taking a Forehead Temperature
Forehead thermometers are convenient but less precise. Use this method:
- Brush hair off forehead and wipe away any sweat.
- Turn on thermometer and hold 1 inch from center of forehead.
- Press button and slowly scan across forehead.
- Release button and check reading.
- Repeat 2-3 times and average temperatures.
Taking an Underarm Temperature
For underarm use:
- Wipe underarm with towel to dry.
- Turn on thermometer and place tip pointing up under arm snugly.
- Hold arm against body to keep thermometer tip in place.
- Leave until thermometer signals done – about 25 seconds.
- Add 1 degree to reading for estimate of oral temperature.
Taking an Ear Temperature
Ear thermometers can be very convenient but technique matters. Follow these guidelines:
- Gently pull ear back to straighten ear canal.
- Insert probe snugly aiming towards the jawbone.
- Press button and leave in place until beep, about 2 seconds.
- For infants under 1, gently pull down on ear.
- Repeat on other ear and use highest reading.
Caring for and Cleaning a Small Thermometer
Be sure to care for your thermometer properly so it stays accurate and avoids spreading germs:
- Replace disposable probe covers between each use.
- Clean with rubbing alcohol between each use if no covers.
- Store in protective case when not in use.
- Replace batteries regularly.
- Don’t immerse digital thermometer in water.
- Don’t bite probe – use care when chewing.
Small digital thermometers provide a convenient way to monitor body temperature. By following proper technique and care, you can gain the most accurate readings and detect any concerning fever or illness early.
When it comes to taking temperature, small digital thermometers offer convenience and speed over traditional glass mercury thermometers. But with the variety of options available, how do you choose the right one? The type of small thermometer you use can impact the accuracy and ease of getting a reading.
Types of Small Thermometers (Ear, Forehead, etc.)

Small digital thermometers come in several styles suited for different applications:
- Ear thermometers use an infrared scanner to measure the infrared heat signatures radiating from the eardrum. They provide quick readings but proper placement is key.
- Forehead thermometers also employ an infrared scanner to read the temperature of the temporal artery in the forehead. Convenient but less precise.
- Oral thermometers are placed under the tongue and use a thermistor to measure core body temperature. Considered most accurate but can be uncomfortable.
- Rectal thermometers with a short, blunted probe can deliver excellent accuracy for small children when used carefully.
- Underarm thermometers work best when held snugly in the armpit and allowed time to read temperature through the skin.
- Pacifier thermometers contain a sensor that reads baby’s temperature from the mouth while sucking.
Other options like temporal artery thermometers and skin strip thermometers are also available. Choosing the right variety comes down to factors like invasiveness, convenience, patient age, and need for maximum accuracy.
Benefits of Using a Small Thermometer

Transitioning from bulky glass thermometers to small digital models offers some useful advantages:
- Digital readings eliminate guesswork and squinting at tiny lines.
- Very fast results – seconds rather than minutes.
- No risk of breakage like glass thermometers.
- Simplicity of one-button operation.
- Compact size for portability and storage.
- Silent so no disruptive shaking sound.
- Some models store past temperature data for tracking.
- Flexible “bendable” designs for ease of use.
For home health care or those monitoring chronic conditions, small digital thermometers provide convenience and speed over older analog versions.
When to Use a Small Thermometer
Knowing when to take someone’s temperature is key to proper thermometer usage. Suggested times to measure body temperature include:
- At the first signs of illness – feeling flushed, achy, chilled, etc.
- When a sore throat, cough, or headache develops.
- If a child seems particularly fussy or irritable.
- With symptoms of potential flu or virus.
- Ongoing monitoring of a chronic health condition.
- After a seizure or fainting episode.
- When caring for infants for whom fever could be dangerous.
Routine temperature checks can provide early notification of infection and prompt medical care if needed.
How to Properly Take a Temperature
While small thermometers are convenient, proper technique is vital for obtaining the most accurate reading:
- Read and follow the instructions for your specific thermometer model.
- Allow sufficient time for the thermometer to register the temperature.
- Take multiple back-to-back readings for consistency.
- Record readings along with date/time for comparison.
- Use probe covers if available to prevent spreading germs.
- Clean the thermometer probe carefully after each use.
- Replace batteries regularly to maintain performance.
With practice, proper placement and usage of your particular thermometer will become second nature.
Normal Temperature Ranges
Contrary to the 98.6°F benchmark, normal body temperature can vary depending on many factors. Here are general normal ranges:
- Oral: 97.8°F – 99°F
- Rectal: 99.6°F – 100.4°F
- Ear: 97.5°F – 99.5°F
- Forehead: 97.5°F – 99.5°F
- Underarm: 96.6°F – 98.1°F
Time of day, age, activity level, and other elements can all impact an individual’s average normal temperature. Tracking readings over time allows you to determine your personal range.
Benefits of Using a Small Thermometer

Have you ever reached for a thermometer when feeling under the weather, only to realize the one you have takes forever to get a reading? Those old-school mercury thermometers we grew up with could easily take 3-5 minutes to register an accurate body temperature. But who has time for that these days?
Enter the age of the small digital thermometer. These convenient little devices can give you a temperature reading in just seconds. No more waiting around with a clunky thermometer under your tongue! Small digital thermometers are affordable, easy to use, and can make monitoring temperatures a breeze. Here are some of the biggest benefits of using a small digital thermometer:
Quick Readings
As mentioned, the main advantage of using a small digital thermometer is the speed at which you can get an accurate temperature reading. Within seconds of placing the thermometer probe under your tongue or against your forehead, the display will show your current temperature. This is much faster than mercury or alcohol thermometers that need a few minutes to equilibrate.
Precise Measurements

Small digital thermometers use advanced electronics and algorithms to deliver precise temperature measurements, usually to within 0.1°F/0.1°C. This level of accuracy is better than traditional glass thermometers and allows you to closely monitor fever levels or subtle temperature changes.
Easy to Read Display
Who hasn’t struggled to read the little markings on those old mercury thermometers? The crisp digital displays on small thermometers eliminate this problem. Most use large numerical readouts that are easy to read, even in low light conditions. Some also have backlit displays for reading in the dark.
Compact Size
As the name suggests, small digital thermometers are petite, portable, and take up hardly any space. Just pop one in your medicine cabinet or first aid kit so it’s always within reach. Some are even small enough to attach to a keychain for on-the-go temperature checks.
Silent Operation
Trying to take a sleeping child’s temperature with a beeping thermometer usually ends with the child wide awake! Small digital thermometers don’t make noise during measurement, allowing you to check temps without disturbing sleeping patients.
Durable Construction
Small digital thermometers are well-constructed from durable plastic and metal. Unlike glass mercury thermometers, you don’t have to worry about breaking these if dropped. Many are waterproof too, so you can safely use them in bathwater.
Hygienic
Sharing thermometers can spread germs. But with most small digital thermometers, you only share the probe cover. This plastic sheath keeps the thermometer probe protected and hygienic between uses. Some thermometers even come with disposable probe covers.
Memory Feature
Many small thermometers can store your last several temperature readings in memory. This lets you track temperature trends over time. Especially helpful for monitoring sick children or the elderly!
Fever Alarm
Some premium models have a fever alarm that beeps when temperatures go above 100°F/38°C. This can alert caregivers that prompt medical attention may be needed for the high fever.
Forehead or Ear Use
While most small digital thermometers take oral or rectal readings, specialized models can take forehead or ear readings too. Forehead strips are quick and easy for babies or children. Ear thermometers, while more expensive, only need a second to get a reading!
Flexible Tip
A flexible probe tip enables you to comfortably take armpit temperatures. This avoids the discomfort of keeping your mouth closed on a hard probe for minutes.
Automatic Shutoff
Forgetful about turning devices off? Small digital thermometers automatically power down after use to conserve batteries. No more dead batteries from accidentally leaving it on!
As you can see, small digital thermometers offer many advantages over traditional glass thermometers. From ultra-quick readings to memory recall to fever alarms, these devices pack helpful features in a compact package. And with low prices under $10, everyone can enjoy the speed, precision, and convenience of small digital thermometers.
The next time you need to take a temperature, grab one of these useful gadgets. Just place the sensor, press a button, and your temperature will be displayed in seconds. Small digital thermometers give you time-saving performance without sacrificing accuracy. Give one a try for your health toolkit or as a gift for loved ones!
When to Use a Small Thermometer

Feeling a little under the weather lately? One of the first things you may reach for is a thermometer to check if you have a fever. But how do you know when it’s really time to grab that handy little device? Small digital thermometers make temperature taking a cinch – when used at the right times.
Monitoring your body temperature can provide vital health insights. But taking your temperature too often can lead to unnecessary anxiety. So when should you whip out a small thermometer to take your temp?
When You Feel Feverish
Feeling feverish is one of the most common reasons to take your temperature. Symptoms like chills, body aches, headache, and fatigue often accompany a fever. If you have these symptoms, take your temperature to see if it is elevated. A reading over 100°F (37.8°C) confirms a fever.
Knowing you have a fever can help guide treatment. Doctors may recommend fever reducers, increased fluids, and rest. Fevers may also indicate when medical evaluation is needed, especially with high fevers over 103°F (39.4°C).
When You’re Ill
Certain illnesses like flu, COVID-19, tonsillitis, pneumonia, ear infections, and UTIs can cause fevers. Taking your temperature when sick helps monitor the course of the illness and effectiveness of treatment.
For example, if you start an antibiotic for an infection and your fever comes down, it suggests the medication is working. Check with your doctor on what temperature readings warrant a call to the office when ill.
Infant or Child is Fussy
Infants and small children can’t verbalize when they feel ill. Fussiness, reduced appetite, and sleepiness may indicate sickness. Taking a baby’s temperature when they seem uncomfortable can detect an unseen fever.
New parents should have an easy-to-use small thermometer on hand to frequently check baby’s temp when unwell. fevers in infants warrant prompt medical attention.
After Vaccinations
It’s common for babies to develop a mild fever after getting vaccinations. Taking their temperature a few times in the hours after shots helps identify this expected side effect.
Monitoring temperatures can also assure parents that the fever resolves within a day or so. Call the doctor if fever lasts over 24 hours after vaccinations.
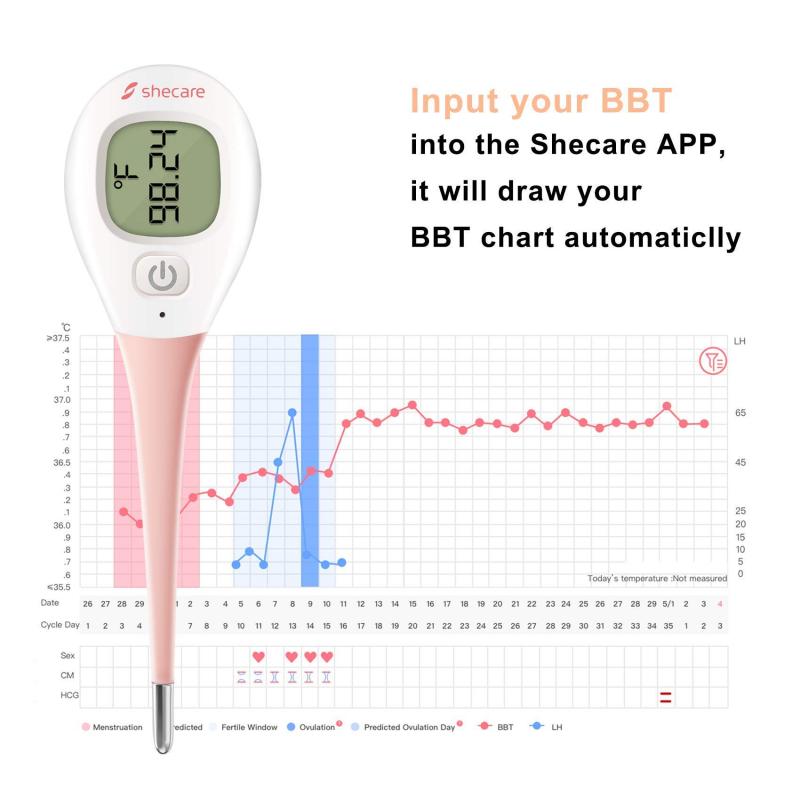
When Tracking Ovulation
Some women notice a slight temperature increase of around half a degree when ovulating. Taking your basal body temperature with a small thermometer each morning can help identify when you’re ovulating.
This can aid couples who are trying to conceive in timing intercourse optimally. Look for this basal temperature spike on days 10-15 of your menstrual cycle.
If You Feel Hot or Chilled
Feeling unusually hot or chilled can also prompt a temperature check. Chills may indicate the onset of an illness or fever.
On the other hand, feeling hot and flushed may reflect menopausal hot flashes, overheating from exercise, or even anxiety. A temperature reading can help discern the cause.
When Monitoring a Medical Condition
Those with chronic medical conditions may need to routinely monitor temperatures. Conditions like diabetes, recurrent UTIs, inflammatory bowel disease, and immune disorders can involve temperature instability.
Checking your temp when you feel unwell provides data for your doctor to assess disease control. But also take it when feeling well to establish your normal baseline.
Before Bed
Taking your temperature before bedtime can serve as a baseline. You can then compare it to overnight or morning temperatures to see if it becomes elevated, indicating illness.
Having this evening baseline temperature improves interpretation of later readings. Mark down each reading to identify temperature trends.
When Caring for an Elderly Person
Frail elderly individuals may not notice or communicate symptoms of illness. Regular temperature screening by caregivers can identify medical issues like infections needing attention.
Note any temperature over 100°F (37.8°C) or 2+ degrees over the person’s baseline. Report these to a doctor to determine if treatment is appropriate.
During or After Surgery
Doctors routinely monitor patient temperatures after surgical procedures to watch for post-operative infection. Temperature spikes after surgery usually require further evaluation and treatment.
At-home monitoring with a small thermometer after discharge provides data to inform follow-up care. Avoid confusion by noting the time of day with each reading.
When You Just Feel “Off”
Sometimes you may just feel generally crummy without specific fever symptoms. Taking your temperature when you feel “off” can reveal an elevated reading warranting medical care.
Trust your instincts and reach for the thermometer when your body gives vague indications that something may be amiss. Better safe than sorry if a fever is brewing.
During illness or any condition causing temperature instability, take readings multiple times a day to establish trends. Keep a temperature log to provide your physician complete information.
Having a compact, easy-to-use small digital thermometer makes frequent temperature checks simple and fast. Keep one handy in your medicine cabinet, so it’s available whenever feeling under the weather strikes. Monitoring your temperature provides valuable health insights to discuss with your doctor.
How to Properly Take a Temperature
Taking someone’s temperature is a simple and common way to check for signs of illness or infection. However, there are some important tips to follow to ensure you get an accurate reading. With a few basic steps, you can become a pro at taking temperatures.
Choosing the Right Thermometer

The first step is selecting the proper thermometer. Here are the most common options:
- Digital thermometers – These electronic thermometers provide a quick digital readout. They are inexpensive, easy to use, and accurate. Just be sure to clean the tip before and after each use.
- Ear or forehead thermometers – These use an infrared scanner to take the temperature. They are very fast but tend to be less reliable. Only use them if you’ve verified their accuracy.
- Rectal thermometers – Considered the most accurate method, but invasive. Only use for infants or when maximum accuracy is critical.
- Oral thermometers – The traditional choice, but can be less sanitary. Be sure to clean thoroughly and avoid biting down.
For routine temperature taking, a digital thermometer is recommended. They provide the best combination of speed, accuracy, and convenience.
Preparing the Person
Proper set up will help ensure you get an accurate reading:
- Wait at least 15-20 minutes after eating, drinking, exercise, or bathing since this can impact temperature.
- Have them sit comfortably in a chair or laying down. Movement right before taking temperature can alter results.
- Remain calm and relaxed. Stress and anxiety can temporarily increase temperature.
- Take temperature in a draft-free room. Air currents from fans, open windows, or air conditioning can lead to erroneous readings.
Taking a Proper Oral Temperature
When using an oral thermometer, follow these steps:
- Make sure the thermometer is clean by washing it with soap and water or disinfecting with alcohol.
- Turn on the thermometer and make sure it is reset to its lowest temperature.
- Place the thermometer tip under the tongue toward the back of the mouth. Ask the person to close their lips tightly around it.
- Have them breathe through their nose – no talking!
- Hold the thermometer in place for the required amount of time – usually 30-60 seconds until it beeps or displays the reading.
- Read and record the temperature, then clean the thermometer.
Key tips: Don’t let them bite down and don’t take temperature right after drinking a hot or cold liquid.
Taking a Temperature Rectally
For babies or when maximum accuracy is needed, a rectal temperature is best. To take:
- Lubricate the tip with a water-soluble jelly for easier insertion.
- Lay the baby belly-down across your lap or have an older child kneel and bend forward.
- Gently insert the thermometer about 1 inch into the anus.
- Hold it still for the required time until it signals – usually 30-60 seconds.
- Remove thermometer and clean thoroughly with soap and water.
Rectal temperatures run about 1 degree higher than oral readings. Only use rectal method for children under 5 years old.
Reading and Resetting
Once done taking the temperature:
- Read the number and write it down along with the time and date.
- Reset the thermometer back to its lowest temperature setting.
- Disinfect the thermometer probe before storing.
Normal temperature is generally considered 98.6°F (37°C) but can range from 97.5–99.5°F (36.4-37.5°C). Keep track of temperatures over time and call a doctor if someone has a temperature over 100.4°F (38°C) or if elevated temperatures last for more than 2-3 days.
What to Avoid
Some common thermometer mistakes include:
- Not cleaning the probe between uses
- Not waiting long enough for an accurate reading
- Letting the probe touch tongue, cheek, teeth or gums
- Not tightly closing lips around oral thermometer
- Not properly inserting rectal thermometer
- Not noting the time and date with each reading
With a quality thermometer and proper technique, temperature taking doesn’t need to be complicated. Just remember the preparation, proper placement, and avoidance of mixing foods or drinks during the process. With practice, taking accurate temperatures will become second nature.
Normal Temperature Ranges

Understanding normal body temperature ranges is important for monitoring health. While 98.6°F (37°C) is the benchmark, a person’s temperature can vary throughout the day and still be considered normal.
Oral Temperature Range
For oral temperature, which is taken by mouth using a thermometer, the standard normal is 98.6°F or 37°C. However, this is more of an average than a hard rule. The typical normal oral temperature range is:
- 97.8–99.1°F (36.5–37.3°C) for adults and children over age 5
- 97.9–100.4°F (36.6–38°C) for children aged 1-5 years
- 97.5–100°F (36.4-37.8°C) for babies under 1 year
Temperatures on the lower end are normal and do not necessarily indicate a problem. Oral readings up to 100.4°F (38°C) may still be considered normal, especially later in the day. Higher temperatures in the evening are common.
Rectal Temperature Range
Rectal temperatures, taken with a thermometer inserted shallowly into the anus, run about 1 degree higher than oral readings. Normal rectal temperature ranges are:
- 99–100.6°F (37.2–38.1°C) for adults and children over age 5
- 99–101°F (37.2–38.3°C) for children aged 1-5 years
- 99–100.9°F (37.2-38.3°C) for babies under 1 year
Rectal temperature is considered the most accurate method but is used primarily for infants or when maximum precision is needed.
Ear Temperature Normal Range

Ear or tympanic temperature is taken electronically by scanning the eardrum with an infrared thermometer. Normal ranges are:
- 97.5–99.5°F (36.4–37.5°C) for infants, children and adults
Ear temperatures tend to be close to rectal readings. However, ear thermometers are less reliable and accurate than other methods.
Forehead Temperature Normal Range
Forehead or temporal artery thermometers use an infrared scanner across the forehead. Normal is:
- 97.5–99.5°F (36.4–37.5°C)
Like ear temperature, forehead readings have more variability than oral or rectal methods.
Factors Affecting Normal Temperature
Many factors can alter body temperature throughout the day. Normal fluctuations can occur due to:
- Time of day – Temperatures tend to peak in the evenings
- Age – Infants and elder adults run lower temperatures
- Activity level – Exercise and metabolism increase heat
- External conditions – Hot or cold environments affect body temperature
- Hormones – Ovulation and menstruation cause variances
- Medications – Some drugs influence thermoregulation
What matters most is the pattern and any variations from an individual’s normal baseline temperature range. Sudden high spikes, low temperatures, or fluctuations can signify an underlying problem.
When a Temperature Is Considered a Fever
In general, a fever is technically defined as a body temperature over 100.4°F (38°C). However, lower temperatures can still be considered a fever if much higher than normal for a given individual. Other fever guidelines include:
- Oral temperature over 100.4°F (38°C)
- Rectal or ear temperature over 101°F (38.3°C)
- Forehead temperature over 100.4°F (38°C)
Fevers are commonly a key sign of infection or illness. If a fever lasts more than 2-3 days, be sure to contact a doctor. Pay attention to any sudden spikes in temperature as well.
Tracking Changes Over Time
To best assess normal body temperature, measure and track it regularly. Note the time of day, method used, and any factors that may have influenced the reading. Watch for variations outside of normal daily fluctuations or your personal baseline ranges.
Understand the typical normal temperature ranges based on site and method used. This provides context for monitoring any given individual. Consistency in timing and technique is key. Contact a physician for guidance on any concerning readings or prolonged abnormalities.
Signs of a Fever

A fever indicates an elevated body temperature, usually due to an underlying illness or infection. But how do you know if someone has a fever without taking their temperature? There are some key signs to watch out for.
Flushed Skin
One of the most common physical signs of a fever is flushed or reddened skin on the face, neck, or body. This occurs as blood vessels dilate to allow more heat release from the skin’s surface. The higher the fever, the more flushed the skin appears.
In light-skinned individuals, the flushed areas may appear pink or red. In darker complexions, the skin may look more flushed than usual. Heat rash can also develop, causing red bumps or patches on the skin that feels hot to the touch.
Sweating
Fever often triggers sweating as the body tries to cool itself down. Any sweating occurring without exertion or high temperatures may be indicative of an elevated internal body temperature.
Sweating is especially common with fever at night, which can cause someone to wake up drenched in sweat. The sweating may be most pronounced on the chest, face, neck, back, and palms of the hands and feet.
Chills, Shivering & Body Aches

Someone with a higher than normal temperature may feel chilled, shiver, and have flu-like body aches. The chills are caused by rapid muscle contraction and relaxation as the body tries to generate more heat through involuntary shivering.
Alternating chills with excessive sweating is particularly telling. The muscle aches seem flu-like, often occurring in the back, arms, and legs. Headaches and general malaise are also common.
Lack of Appetite
Low appetite and nausea frequently accompany a fever. The body is diverting energy toward mounting an immune response, decreasing digestive function in the process. Food may be unappealing or even make someone feel sick to their stomach.
In babies and younger children, refusing to eat or drink as normal is often one of the first fever symptoms noticed. Dehydration is a potential complication.
Irritability & Lethargy
Fever, chills, body aches, and nausea make a person feel unwell, which leads to mood changes like irritability, crying, and lack of interest in normal activities. The fever is sapping the body’s energy.
Lethargy, drowsiness, and lack of energy are common fever symptoms. Someone may sleep or rest more than usual. With an elevated temperature, any movement or activity takes more effort and feels exhausting.
Confusion & Disorientation
A very high fever can cause confusion, delirium, hallucinations, and trouble thinking clearly. This is a medical emergency, as temperature over 104° F (40° C) can lead to seizures, brain damage, or death.
In children, look for any strange behavior that seems out of character. Adults may act confused about their location or identity, be unable to follow simple instructions, or have garbled speech.
Measuring Temperature
The most definitive way to identify a fever is to take someone’s temperature. Oral thermometers are recommended for routine temperature taking. Ear, forehead and temporal artery thermometers are faster but less reliable alternatives.
Any temperature over 100.4° F (38° C) indicates a significant fever, especially if over 102° F (39° C). However, even a lower grade temperature can be considered fever if elevated for that particular person.
Duration of Fever Symptoms
Pay attention to how long fever symptoms persist. A common cold may cause a low-grade fever for a day or two. The flu brings on a higher fever lasting around 3-4 days.
Any fever lasting longer than a week requires medical attention. The same applies to infants under 3 months with a rectal temperature over 100.4° F (38° C). Be alert for any other worrying symptoms accompanying the fever.
Call the Doctor If…

Contact your doctor if:
- Fever over 102° F (39° C) in adults, over 101° F (38.3° C) in children
- Fever lasts longer than 3 days in adults, 2 days in children
- Recurrent fevers keep returning
- Fever accompanied by severe headache, neck stiffness, mental changes, difficulty breathing, or rash.
Trust your instincts. Even low-grade sustained fever or any unusual fever symptoms warrant a doctor visit. Fever often provides an important early warning of underlying illness.
How Accurate Are Small Thermometers?
Small digital thermometers have become a popular choice for temperature taking at home due to their affordability, ease of use, and fast results. But how reliable are these mini thermometers? Here’s an overview of their accuracy.
Overall Accuracy
In general, modern digital stick thermometers provide accurate temperature measurements falling within +/- 0.1-0.2 degrees Fahrenheit of a reading taken simultaneously using a standard oral or rectal mercury thermometer.
Clinical studies evaluating various models of digital thermometers compared to glass mercury versions show that the small digital options reliably produce results well within the acceptable range for accuracy.
Advantages Over Mercury

The precision of digital sticks actually exceeds old-fashioned mercury thermometers in several ways:
- Quick precise readout rather than estimating where the mercury line falls.
- No risk of broken glass and mercury exposure.
- Measures in 10 seconds versus 3+ minutes for mercury.
- Can take many back-to-back readings quickly.
- Stores previous temperature readings.
- Some models beep when finished.
For these reasons, trusted health organizations including the Mayo Clinic recommend switching to digital thermometers over mercury ones.
Oral vs. Rectal Readings
One accuracy consideration is that digital stick thermometers provide more precise oral temperature readings than rectal.
Rectal thermometers are shaped specifically to insert shallowly into the anus for maximum accuracy. Oral digital models are not ideal for rectal use. However, for oral temperature taking, digital stick thermometers perform very well.
Proper Technique
To ensure optimum accuracy with a digital oral thermometer:
- Wait 15-20 minutes after eating, drinking, or exercise.
- Place carefully under the tongue toward the back of mouth.
- Ensure lips seal tightly around thermometer probe.
- Avoid biting down or touching teeth/tongue.
- Hold in place until it beeps – usually 10 seconds.
Proper measurement technique is key for any thermometer. Digital options provide more room for user error than mercury since they measure so rapidly.
Regular Calibration
Like any thermometer, digital sticks lose calibration over time with heavy use. Replace your thermometer annually or any time results seem inaccurate compared to how you normally feel.
Some models let you manually recalibrate by pressing a button. Compare against a known accurate thermometer like recently calibrated mercury one from your doctor’s office.
Look for Quality Models
Here are signs of a high-quality digital thermometer for optimal accuracy:
- Meets ISO accuracy standards
- Has been clinically tested for precision
- Recommended by medical experts and organizations
- Trusted brand with good reputation
- Good owner reviews and feedback
- Long battery life and warranty from manufacturer
There are many inferior products out there, so choose carefully. Spending a little more upfront ensures you get precise consistent results.
Know the Limitations
While generally reliable for typical temperature taking, oral digital thermometers may be less accurate in certain circumstances:
- Very high or very low body temperatures at extremes.
- Rectal versus oral route usage.
- Old thermometers in need of recalibration.
- Poor measurement technique.
- Comparing single time measurement versus tracking temperature continuously.
- Severe hypothermia or hyperthermia life-threatening states.
For serious illness or emergencies, doctors have more sophisticated thermometer options. But for daily use, a quality digital stick thermometer provides accurate results you can rely on.
Tips for Getting an Accurate Reading
Taking an accurate body temperature is vital for assessing health. However, many factors can impact the reading. Here are tips to help get a precise temperature measurement.
Choose the Right Thermometer
Opt for an oral digital thermometer. These offer the best balance of affordability, ease of use, speed, and accuracy for home temperature taking. Make sure to replace it annually.
Use Proper Placement

For oral readings, place the thermometer tip under the tongue toward the back of the mouth. Close lips tightly around it. Avoid biting down or letting it touch the tongue, teeth or inner cheeks which can alter the results.
Take the Time
Leave the thermometer in place until it signals completion (usually 10 seconds for digital). Removing early can lower the reading. For rectal use in infants, insert only 1 cm and hold for up to 60 seconds for an accurate core body temperature.
Get in the Habit
Take temperature at the same time daily as body temperature varies throughout the day. Consistency gives the best sense of an individual’s normal.
Note the Conditions
Record details like time taken, temperature method, recent medicines, activity level, and environment. These details provide context affecting temperature.
Avoid Eating and Drinking Before
Wait at least 15-20 minutes after eating or having cold/hot beverages as food and drink impact oral temperature. Also avoid taking right after exercise or a bath which can briefly alter readings.
Mean Multiple Readings
For best accuracy, take 2-3 back-to-back readings and use the average. Repeated measurements minimize normal fluctuations.
Try Different Methods
If concerned about accuracy, compare your digital oral stick to a rectal or ear reading. Rectal thermometers are considered the gold standard, especially for infants.
Ensure Proper Conditions
Take temperature in a draft-free room without air currents from fans, open windows, or air conditioning which can distort results. Stay relaxed as stress affects temperature.
Disinfect Between Uses
Always clean the thermometer tip with soap and water or rubbing alcohol between readings to prevent transmitting bacteria.
Know Your Baseline
Track your regular temperature readings over time to determine personal average, fluctuations and any abnormalities for you individually.
Replace Batteries
Make sure your digital thermometer has fresh batteries. Weak batteries lead to inaccurate low readings. Most last approximately 2000 readings before needing replacement.
Recalibrate Annually

Check calibration periodically against a known accurate thermometer. Recalibrate if readings are off. Replace oral digital models annually for best performance.
Following these tips helps minimize normal variability in temperature taking. Be systematic in technique, conditions, timing, and recording details to get the most accurate reading possible.
Checking a Baby or Child’s Temperature
It’s important to know how to properly take a baby or child’s temperature. Young children can’t communicate how they feel, so checking for fever is key. Here are tips for getting an accurate reading.
Choose the Right Thermometer
For babies under 3 months, a rectal thermometer is recommended. Older babies and toddlers need a digital thermometer designed specifically for oral/rectal/armpit use with a flexible tip.
Look for digital sticks offering accurate readings in only 10 seconds to keep squirmy kids still. An appealing color helps too!
Rectal Readings for Under 3 Months

Rectal temperature is the gold standard for accuracy in infants. To take:
- Lay baby tummy-down across lap or have an older child kneel and bend forward.
- Gently insert the tip only 1 cm into the anus.
- Hold for up to 60 seconds until thermometer beeps.
- Remove and clean thoroughly with soap and water.
Rectal runs about 1 degree higher than oral. 100.4°F (38°C) rectal is considered fever in babies under 3 months.
Oral Readings for Older Babies & Toddlers
For ages 4 months to 3 years, carefully take an oral temperature by:
- Insert tip under tongue near back of mouth.
- Have child close lips around thermometer.
- Gently hold it there until the 10 second beep.
- Distract child by stroking their cheek or Singing.
Oral readings are lower than rectal. For ages 1-5 years, over 100°F (37.8°C) oral indicates fever.
Armpit Readings
If oral temperature taking is challenging, place the flexible tip in baby’s armpit instead. Hold arm down for an accurate reading.
Axillary temperatures run about 1 degree lower than oral. A fever threshold here would be 99°F (37.2°C).
Ear Thermometers
Infrared ear thermometers can provide quick readings. However, accuracy depends on proper technique and they tend to be less reliable in young children. Use as a secondary temperature method only.
Forehead Strips
Disposable thermometer strips or stickers that adhere to the forehead are convenient but not recommended. They are highly variable and inaccurate for assessing fever in babies and children.
Timing Matters
Take temperature when symptoms seem worst, usually late afternoon or evening as fevers tend to rise throughout the day. Record time taken with the reading.
Be Consistent
Always take temperature in the same location each time (oral, rectal, armpit, ear) for consistency. Compare apples to apples when looking for fever.
Learn Normal Range
Know your child’s usual temperature range when well. Any reading above their norm could indicate fever, even below the standard fever thresholds.
Note Other Symptoms
Fever often coincides with flushed skin, sweating, chills, reduced appetite, and irritability in children. Look for associated symptoms.
When to Call the Doctor

Consult your pediatrician if baby under 3 months has a rectal temperature over 100.4°F (38°C) or for any fever concerns in a young infant. For older babies and children, call for fevers over 102°F (39°C) or any fever lasting over 2 days without explanation.
Knowing the proper thermometer type and method for checking your baby or child’s temperature helps ensure you get an accurate reading to assess for fever or illness.
Taking Your Temperature Orally
One of the most common ways to check your body temperature is by taking it orally using a thermometer. Here are tips for properly taking an oral temperature reading at home.
Choose the Right Thermometer
Digital thermometers are recommended over mercury for home use. Seek out a digital stick thermometer that’s affordable, easy to use, provides fast (10 second) readings, and specifically designed for oral use.
Prepare Properly
Avoid eating, drinking, exercising, or bathing for 15-20 minutes beforehand as this affects oral temperature. Also pick a draft-free room without air currents from fans, AC, or open windows.
Clean the Thermometer
Always clean the thermometer tip before and after use with soap and water or rubbing alcohol to prevent spreading germs.
Turn Thermometer On
Digital thermometers need to be turned on first and reset to the default lowest reading (usually around 94°F or 34°C). Make sure fresh batteries are installed.
Place Under Tongue
Gently place the thermometer tip as far back under your tongue as comfortable, near but not touching the bottom of your mouth.
Close Lips Tightly
Completely close lips to seal around the thermometer. Don’t bite down on it. Keep lips sealed until it beeps.
Hold Steady
Hold the thermometer in place under your tongue without moving, talking, or disturbing it until the reading is complete, about 10-20 seconds. Breath through your nose.
Note the Reading
When it beeps, remove thermometer and note the temperature reading along with time and date. Normal oral temperature is 97.6-99.6°F (36.4-37.6°C).
Take 2-3 Times
For best accuracy, take your temperature 2-3 times in a row at the same session and use the average. This minimizes normal fluctuations.
Try Other Methods
If concerned about oral reading accuracy, also take a rectal or ear temperature for comparison. Rectal is considered the most precise.
Clean After Use
Always sanitize the tip with soap/water or alcohol wipe after each use to kill germs before storage or reuse.
Note Any Abnormalities
Record any symptoms along with temperature and monitor patterns over time. Consult your doctor if any readings cause concern.
With the proper technique, taking your temperature orally can provide quick and accurate insight into possible fever or illness. Make it part of your health self-monitoring routine.
Taking a Forehead Temperature
Measuring temperature using a forehead thermometer is a quick, non-invasive method. Here are tips on how to properly take someone’s temperature at the forehead or temporal artery.
Choose a Forehead Thermometer

Use an electronic thermometer designed specifically for the forehead. Look for an adjustable tip to fit all ages. Seek a model with a silent mode and large digital readout.
Read the Instructions
Read the manufacturer directions for proper use of your particular forehead thermometer model. Specific techniques can vary.
Clean the Thermometer
Before first use and between readings, clean the thermometer tip with an alcohol wipe or soap and water to prevent spreading germs.
Remove Hair, Sweat, Dirt
Gently brush away any hair, sweat or dirt from the center of the forehead to ensure good skin contact for accuracy.
Position Correctly
Have the person sit upright and bring the thermometer probe in contact with the center of the forehead, about an inch above eyebrows.
Press and Hold in Place
Press and hold the thermometer flush against the forehead skin for the required time, usually 10-15 seconds until it beeps.
Take 2-3 Readings
For best results, take 2-3 consecutive forehead temperature readings at the same session and use the highest measurement.
Note the Temperature
The digital display will show the temperature reading. Normal forehead temperature is 97.5-99.5°F (36.4-37.5°C).
Add Context
Note time of day, concurrent symptoms, recent medicines or activity that could impact the temperature.
Clean After Use
Disinfect the thermometer probe with an alcohol wipe after each use before storing it.
Minimize Error
Avoid taking forehead temperature after exercising, bathing, or being in direct sunlight which alter readings. Stay in draft-free room.
With practice, a forehead thermometer can provide a relatively quick and convenient way to assess for fever. Just be sure to use proper technique for most accurate readings.
Taking an Underarm Temperature
Measuring temperature under the arm (axillary) can be an alternative to oral readings. Here are some tips on properly taking underarm temperature.
Choose Underarm Thermometer
Use a digital thermometer designed for axillary use with a thin, flexible tip that can easily slip into the armpit.
Clean Thermometer Tip
Carefully clean the thermometer probe before each use with soap/water or alcohol wipe to prevent spreading germs.
Apply Some Powder
Lightly sprinkle some baby powder or cornstarch on the armpit. This allows smooth thermometer gliding and absorption of sweat.
Place in Armpit
Lift arm and insert the tip of the thermometer as far back into armpit as possible, adjacent to the body.
Lower Arm
Keep arm pressed tightly against the body and apply pressure against the body to keep thermometer firmly in place.
Hold In Place
Hold thermometer snugly in armpit for the required time until it beeps – usually 10 seconds for digital.
Read Temperature
Note the digital reading after it beeps. Normal underarm temperature is 97.5-99.1°F (36.4-37.2°C)
Repeat 2-3 Times
For accuracy, repeat the underarm process 2-3 times in a row and use the highest reading.
Both Underarms
Consider taking temperature in both underarms and comparing to account for any asymmetry.
Use Oral Too
For confirmation, also take oral temperature since underarm readings run about 1°F (0.6°C) lower than oral.
Disinfect After Use
Clean thermometer probe thoroughly with soap/alcohol to disinfect after each use before storage.
With practice, taking underarm temperature can be an easier option than oral, especially for young children. Just be sure to use proper technique.
Taking an Ear Temperature
Using an ear (tympanic) thermometer is a quick, non-invasive way to take someone’s temperature. Here are some tips for properly taking temperature through the ear canal.
Choose an Ear Thermometer
Use a thermometer designed specifically for the ear canal. Seek out a trusted brand with a reputation for accuracy and reliability.
Read the Instructions

Read the manufacturer’s directions for your particular model. Proper technique can vary between ear thermometer brands.
Clean Tip Before Use
Always clean thermometer tip with alcohol wipe or soap/water before first use and between readings to prevent spreading germs.
Insert Properly
Gently pull ear back to straighten canal. Insert tip snugly into ear aiming toward the membrane of eardrum.
Press Button to Take Reading
With tip aimed at eardrum, press button to take reading. Measurement occurs very quickly, usually within 1-2 seconds.
Read Digital Temperature
The digital display will show the temperature reading. Normal ear temperature is 97.5-100.4°F (36.4-38°C).
Take 2-3 Times
For accuracy, repeat the ear temperature process 2-3 times per ear and use the highest reading.
Use Other Methods Too
Consider also taking oral or rectal temperature to confirm ear readings which can have more variability.
Note Time and Symptoms
Record date, time, symptoms, recent medicines or activities that could impact temperature.
Clean After Each Use
Disinfect thermometer probe with alcohol wipe after each reading before storage to prevent germ spread.
Watch for Problems
Avoid taking temperature after bathing, swimming, or lying down. Look for ear wax blockage, discharge, or infection prior to use.
With proper placement and technique, an ear thermometer can give fast temperature readings. Just be sure to use it correctly for optimal accuracy.
Caring for and Cleaning a Small Thermometer
Proper maintenance and hygiene are key to ensuring your small digital thermometer performs accurately. Here are tips for cleaning and caring for a digital stick thermometer.
Disinfect Between Uses
Always disinfect the thermometer probe before and after each use. Wash with soap and warm water or wipe with rubbing alcohol to prevent transmitting germs.
Store in Protective Case
Keep your thermometer in the provided protective case or storage sleeve when not in use. This prevents damage to the digital display and probe.
Avoid Extreme Temperatures
Don’t store the thermometer long-term in very hot or very cold environments like a car in summer or winter. Follow storage temperature guidelines.
Remove Batteries if Storing Long-Term
If storing for an extended period of time, remove batteries prior to storage. Batteries can corrode over several months if left in place.
Replace Batteries Annually
For optimal performance, replace batteries once a year even if the low battery light isn’t on yet. Weak batteries lead to inaccurate readings.
Don’t Immerse Fully in Liquids
Take care not to fully submerge or soak the entire thermometer in cleaning liquids or water, just the probe. Damage can occur.
Don’t Use Abrasive Cleaners
Avoid abrasive scouring pads or cleaners when cleaning probe tip. Gently wash with soap and water or disinfectant wipes.
Check for Damage

Inspect for cracks or damage to the digital display, buttons, or probe. Replace if any issues are noted with functionality or accuracy.
Calibrate Annually
Check calibration about once per year against a known accurate thermometer from your doctor’s office to ensure precision.
Replace Every 2-3 Years
Consider replacing your oral digital thermometer every 2-3 years with heavy use for most accurate readings.
With careful handling, storage, cleaning and maintenance your digital stick thermometer can provide reliable temperature readings for years of use.

