New Insights into Debeere and Debrer Diseases Causes Symptoms and TreatmentsNew Insights into Debeere and Debrer Diseases Causes Symptoms and Treatments
Understanding the Causes and Risk Factors of Debeere and Debrer
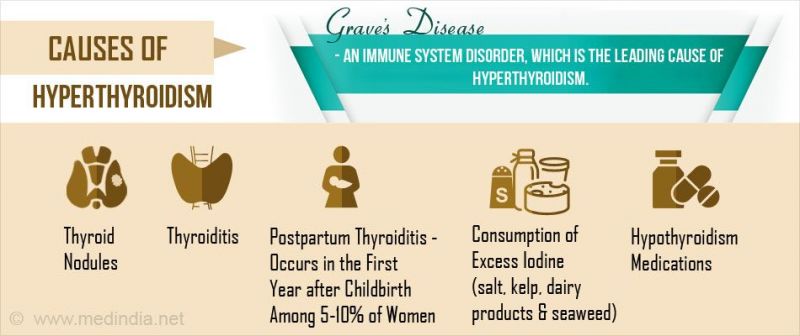
Debeere and debrer diseases have complex and multifactorial causes, but research over the years has uncovered some of the key contributing factors. Genetics play an important role, as people with a family history of either condition have a predisposition. Environmental triggers also come into play – exposure to certain toxins or pollutants may activate the disease pathway in those with a genetic vulnerability.
In terms of lifestyle, diet is one of the most significant risk factors. Diets high in processed foods, sugar, unhealthy fats, and low in fiber have been strongly associated with increased incidence of debeere and debrer. Obesity and being overweight are additional risk factors, as excess adipose tissue drives systemic inflammation. High stress levels and lack of exercise also correlate with greater risk. The immune system seems to be involved as well, as autoimmunity and imbalanced cytokine levels are often seen in debeere and debrer patients.
While more research is still needed, it’s clear that a combination of genetic, environmental, and lifestyle factors interact to determine someone’s susceptibility. By understanding and addressing modifiable risk factors like diet, activity levels, and stress, individuals may be able to reduce their chances of developing these conditions. Healthy eating, regular exercise, stress management, maintaining normal weight, and avoiding exposure to toxins are all recommended. Those with family history may consider genetic testing and take extra precautions. Increased awareness of risk factors empowers patients and physicians to make choices that can lower disease risk.
Distinguishing Key Differences Between Debeere and Debrer
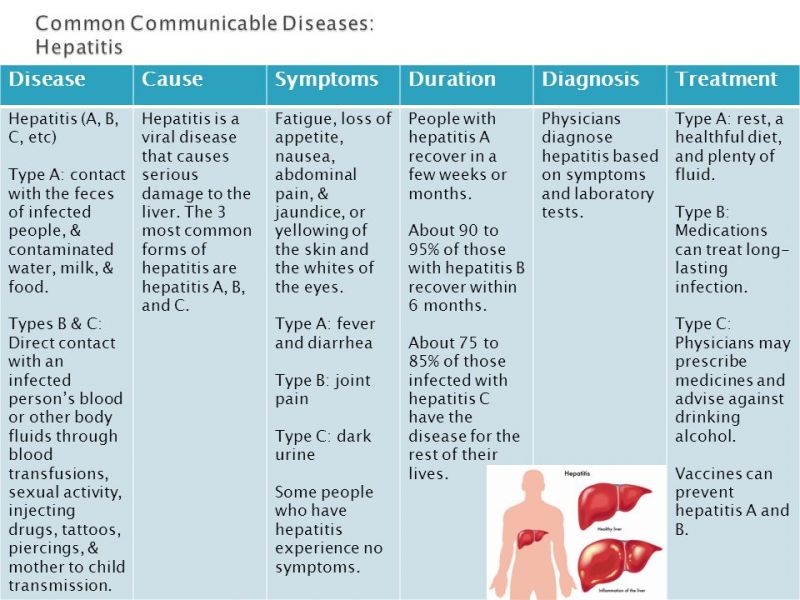
While debeere and debrer share some similar characteristics, there are important differences between the two conditions that are critical to understand. Debeere primarily affects the liver and gastrointestinal system, whereas debrer most severely impacts the kidneys and cardiovascular system. The pathophysiology differs as well – debeere is characterized by abnormal fat deposits in the liver leading to inflammation and scarring. In contrast, debrer involves dysfunction of the glomerular filtration system in the kidneys. Genetically, they have distinct gene associations, with debeere linked to variants in genes regulating lipid metabolism, and debrer associated with genes controlling blood pressure and kidney function.
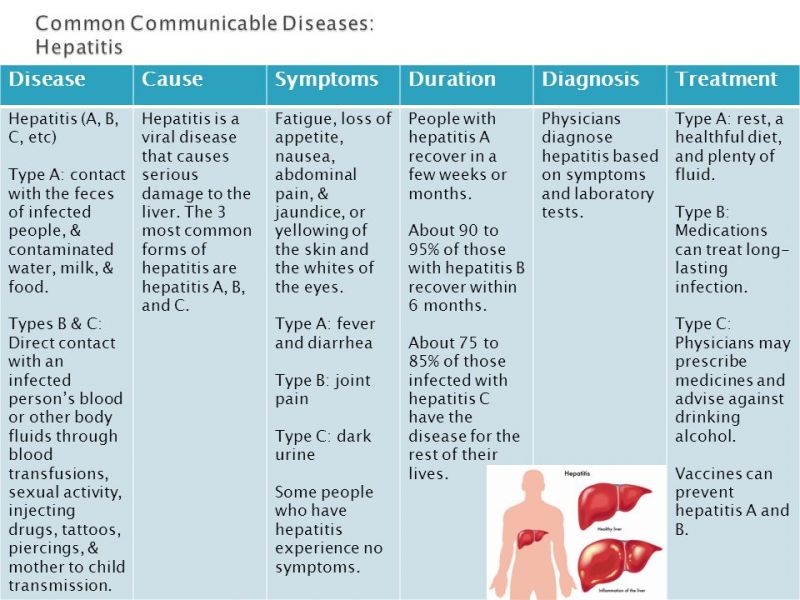
Clinically, the most prominent symptoms also diverge. Debeere often first presents with fatigue, abdominal discomfort, nausea, and jaundice. Debrer typically manifests with fluid retention, frequent urination, hypertension, and edema. While weight loss, appetite changes, and anemia can occur in both, the onset tends to be more rapid in debeere. In terms of diagnosis, debeere is identified via liver enzyme tests, imaging, and sometimes liver biopsy. Debrer is confirmed primarily through urine protein tests, eGFR, and kidney imaging studies.
Regarding treatment, the approaches differ significantly as well. Lifestyle changes involving diet, exercise, and abstinence from alcohol are cornerstones of treating debeere. Medications may include corticosteroids, immunosuppressants, or antivirals. Debrer management focuses on controlling hypertension and proteinuria through ACE inhibitors, ARBs, and diuretics. When kidney function declines severely in debrer, dialysis or transplantation may be required, whereas debeere progresses to cirrhosis and end-stage liver disease.
In summary, while both are serious chronic conditions, debeere and debrer have distinct mechanisms, symptoms, diagnostic criteria, and treatment protocols. Recognizing the key differences is vital for early and accurate diagnosis, so that patients can receive appropriate care based on the specific disease process involved.
Examining the Major Causes and Risk Factors of Debeere and Debrer
As complex conditions, debeere and debrer have a variety of genetic, lifestyle, and environmental factors that contribute to their development. Family history and genetic predisposition play a major causal role. Having a first-degree relative with either disease significantly raises one’s risk. Certain genetic variants, like those affecting lipid metabolism in debeere or blood pressure regulation in debrer, make individuals more susceptible.
Diet and nutrition status are also pivotal risk factors. Diets high in processed carbohydrates, added sugars, saturated fats, and sodium have been strongly linked to increased incidence of both diseases. These foods promote inflammation, insulin resistance, hypertension, and other effects that accelerate disease progression. Being overweight or obese also correlates to higher risk, as excess visceral fat causes metabolic dysfunction.
Environmental exposures can trigger these conditions as well. Toxins like pesticides, heavy metals, air pollution, and industrial chemicals are implicated in debeere and debrer. These compounds create oxidative stress, damage blood vessels, and disrupt normal cellular processes. Certain medications, like NSAIDs and chemotherapy drugs, can also lead to liver or kidney injury in sensitive individuals.
High stress levels, sedentary lifestyles, smoking, and excessive alcohol consumption further raise disease risk. Psychological stress activates inflammatory pathways and the sympathetic nervous system. Lack of exercise leads to insulin resistance, weight gain, and hypertension. Smoking and alcohol cause direct organ damage while depleting antioxidants.
In summary, while genes load the gun, lifestyle and environmental factors often pull the trigger when it comes to debeere and debrer. Addressing modifiable risk factors by adopting healthy diets, maintaining normal weight, exercising, limiting environmental exposures, and managing stress can help prevent these diseases despite genetic susceptibility.
Recognizing the Common Symptoms of Debeere and Debrer
In contrast, Debrer disease predominantly affects the kidneys and cardiovascular system. The primary pathological feature of Debrer is dysfunction of the glomerular filtration system in the kidneys. This leads to impaired kidney function, which can have far-reaching effects on overall health and well-being.
Genetic Factors in Debeere and Debrer Diseases
Genetic predisposition plays a crucial role in both Debeere and Debrer diseases. However, the specific genes involved differ between the two conditions:
- Debeere disease is associated with variants in genes regulating lipid metabolism
- Debrer disease is linked to genes controlling blood pressure and kidney function
Understanding these genetic differences is essential for developing targeted therapies and identifying individuals at higher risk for each disease.
Recognizing the Symptoms and Clinical Presentation
Early recognition of symptoms is crucial for timely diagnosis and treatment of both Debeere and Debrer diseases. The clinical presentation of these conditions can vary significantly, reflecting their distinct organ system involvement.

Debeere Disease Symptoms
Patients with Debeere disease often experience:
- Fatigue
- Abdominal discomfort
- Nausea
- Jaundice (yellowing of the skin and eyes)
- Weight loss
- Changes in appetite
Debrer Disease Symptoms
The typical presentation of Debrer disease includes:
- Fluid retention
- Frequent urination
- Hypertension (high blood pressure)
- Edema (swelling, especially in the legs and ankles)
- Anemia
- Fatigue
It’s important to note that while some symptoms may overlap, the onset and progression of these diseases can differ. Debeere disease often has a more rapid onset of symptoms compared to Debrer disease.
Diagnostic Approaches for Debeere and Debrer Diseases
Accurate diagnosis is crucial for effective management of Debeere and Debrer diseases. The diagnostic approaches for these conditions reflect their distinct pathophysiologies and organ system involvement.
Diagnosing Debeere Disease
To confirm a diagnosis of Debeere disease, healthcare providers typically employ the following methods:

- Liver enzyme tests
- Imaging studies (ultrasound, CT, or MRI of the liver)
- Liver biopsy (in some cases)
Diagnosing Debrer Disease
For Debrer disease, the diagnostic process often includes:
- Urine protein tests
- Estimated glomerular filtration rate (eGFR) measurement
- Kidney imaging studies (ultrasound or CT)
- Blood pressure monitoring
Why is early diagnosis important for Debeere and Debrer diseases? Early detection allows for prompt intervention, potentially slowing disease progression and improving long-term outcomes. It also enables healthcare providers to implement appropriate management strategies tailored to each condition.
Exploring Risk Factors and Prevention Strategies
Understanding the risk factors associated with Debeere and Debrer diseases is crucial for developing effective prevention strategies. While some risk factors are non-modifiable, such as genetic predisposition, many can be addressed through lifestyle changes and preventive measures.
Common Risk Factors
Several risk factors are shared between Debeere and Debrer diseases:

- Family history of the disease
- Obesity or overweight status
- Poor diet high in processed foods, sugar, and unhealthy fats
- Sedentary lifestyle
- Chronic stress
- Exposure to environmental toxins
Prevention Strategies
To reduce the risk of developing Debeere or Debrer disease, individuals can adopt the following preventive measures:
- Maintain a healthy weight through balanced diet and regular exercise
- Consume a diet rich in fruits, vegetables, whole grains, and lean proteins
- Limit intake of processed foods, added sugars, and saturated fats
- Engage in regular physical activity (at least 150 minutes of moderate-intensity exercise per week)
- Manage stress through relaxation techniques, mindfulness, or counseling
- Avoid exposure to environmental toxins and pollutants when possible
- If there’s a family history, consider genetic testing and take extra precautions
How effective are these prevention strategies? While no prevention method is 100% effective, adopting these lifestyle changes can significantly reduce the risk of developing Debeere and Debrer diseases. Moreover, these strategies promote overall health and well-being, offering benefits beyond disease prevention.

Innovative Treatment Approaches for Debeere Disease
Management of Debeere disease requires a multifaceted approach, combining lifestyle modifications with medical interventions. Recent advancements in treatment strategies have shown promising results in slowing disease progression and improving patient outcomes.
Lifestyle Modifications
The cornerstone of Debeere disease treatment involves significant lifestyle changes:
- Dietary modifications: Adopting a balanced, nutrient-rich diet low in processed foods and saturated fats
- Regular exercise: Engaging in moderate physical activity for at least 30 minutes daily
- Weight management: Achieving and maintaining a healthy body weight
- Alcohol abstinence: Completely avoiding alcohol consumption
Medical Interventions
Depending on the severity and progression of Debeere disease, various medical treatments may be prescribed:
- Corticosteroids: To reduce inflammation in the liver
- Immunosuppressants: To modulate the immune response and prevent further liver damage
- Antiviral medications: If viral hepatitis is a contributing factor
- Liver-protective agents: To support liver function and promote regeneration
In advanced cases of Debeere disease that progress to cirrhosis or end-stage liver disease, liver transplantation may be considered as a last resort.

Emerging Therapies
Ongoing research is exploring novel treatment approaches for Debeere disease:
- Targeted gene therapies to address specific genetic mutations
- Stem cell treatments to promote liver regeneration
- Microbiome modulation to improve gut-liver axis function
How do these innovative treatments impact patient outcomes? While still in various stages of development and clinical trials, these emerging therapies show promise in potentially reversing liver damage and improving long-term prognosis for Debeere disease patients.
Cutting-edge Management Strategies for Debrer Disease
The treatment of Debrer disease focuses on preserving kidney function, managing associated cardiovascular risks, and addressing symptoms. Recent advancements have led to more personalized and effective management strategies.
Blood Pressure Control
Managing hypertension is crucial in Debrer disease treatment. Commonly prescribed medications include:
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin receptor blockers (ARBs)
- Calcium channel blockers
- Diuretics
These medications not only control blood pressure but also help reduce proteinuria, a hallmark of Debrer disease.

Proteinuria Management
Reducing protein excretion in urine is essential for slowing kidney damage. Strategies include:
- Dietary protein restriction under medical supervision
- Use of ACE inhibitors or ARBs to reduce proteinuria
- Novel agents targeting specific pathways involved in protein leakage
Cardiovascular Risk Reduction
Patients with Debrer disease have an increased risk of cardiovascular complications. Management includes:
- Lipid-lowering medications (statins)
- Antiplatelet therapy when appropriate
- Lifestyle modifications to improve cardiovascular health
Renal Replacement Therapy
In advanced stages of Debrer disease, when kidney function declines severely, renal replacement therapy may be necessary:
- Hemodialysis
- Peritoneal dialysis
- Kidney transplantation
What factors influence the choice of renal replacement therapy? The decision depends on various factors including patient preference, overall health status, availability of donors, and the presence of comorbidities. Each option has its own benefits and considerations, and the choice is made in close consultation between the patient and their healthcare team.

The Role of Precision Medicine in Debeere and Debrer Diseases
Precision medicine is revolutionizing the approach to Debeere and Debrer diseases, offering tailored treatment strategies based on individual genetic, environmental, and lifestyle factors. This personalized approach holds the promise of more effective interventions and improved patient outcomes.
Genetic Profiling
Advances in genetic sequencing technologies have enabled more comprehensive genetic profiling of patients with Debeere and Debrer diseases. This allows for:
- Identification of specific genetic variants associated with disease risk or progression
- Prediction of treatment response based on genetic markers
- Development of targeted therapies addressing specific genetic abnormalities
Biomarker-guided Therapy
The use of biomarkers is becoming increasingly important in managing Debeere and Debrer diseases:
- Novel biomarkers for early disease detection and monitoring
- Predictive biomarkers to guide treatment selection
- Pharmacogenomic markers to optimize medication dosing and minimize side effects
Personalized Lifestyle Interventions
Precision medicine extends beyond genetic and molecular approaches to include personalized lifestyle recommendations:

- Tailored dietary plans based on individual metabolic profiles
- Customized exercise regimens accounting for genetic predispositions and physical limitations
- Targeted stress management strategies addressing individual psychological factors
How does precision medicine improve outcomes for Debeere and Debrer patients? By tailoring interventions to individual patient characteristics, precision medicine aims to enhance treatment efficacy, reduce adverse effects, and improve overall quality of life. This approach allows for more efficient use of healthcare resources and potentially slows disease progression more effectively than one-size-fits-all strategies.
Future Directions in Debeere and Debrer Disease Research
The landscape of Debeere and Debrer disease research is rapidly evolving, with several promising avenues of investigation that could lead to significant breakthroughs in understanding, diagnosing, and treating these conditions.
Advanced Imaging Techniques
Innovative imaging technologies are being developed to enhance early detection and monitoring of Debeere and Debrer diseases:

- High-resolution MRI techniques for detailed liver and kidney imaging
- Molecular imaging to visualize disease processes at the cellular level
- Artificial intelligence-assisted image analysis for more accurate diagnosis
Immunotherapy Approaches
Researchers are exploring the potential of immunotherapy in managing Debeere and Debrer diseases:
- Targeted immunomodulators to reduce inflammation and tissue damage
- Chimeric antigen receptor (CAR) T-cell therapy for advanced stages of disease
- Vaccine development to prevent disease onset in high-risk individuals
Regenerative Medicine
The field of regenerative medicine holds promise for repairing damaged tissues in Debeere and Debrer diseases:
- Stem cell therapies to promote liver and kidney regeneration
- Tissue engineering techniques to create functional organ replacements
- Gene editing technologies to correct disease-causing mutations
Microbiome Research
Growing evidence suggests that the gut microbiome plays a significant role in both Debeere and Debrer diseases:
![]()
- Studies on microbiome-based therapies to modulate disease progression
- Investigation of probiotic and prebiotic interventions
- Exploration of fecal microbiota transplantation as a potential treatment
What potential impact could these research directions have on patient care? These emerging areas of research hold the promise of more effective prevention strategies, earlier and more accurate diagnosis, and potentially curative treatments for Debeere and Debrer diseases. As our understanding of these complex conditions grows, we move closer to developing interventions that can significantly improve patient outcomes and quality of life.
The field of Debeere and Debrer disease research is dynamic and rapidly advancing. Continued investment in these areas of investigation is crucial for developing the next generation of diagnostic tools and therapeutic interventions. As we unravel the complexities of these diseases, we open new possibilities for improving the lives of millions affected by Debeere and Debrer worldwide.

Understanding the Causes and Risk Factors of Debeere and Debrer
Debeere and debrer diseases have complex and multifactorial causes, but research over the years has uncovered some of the key contributing factors. Genetics play an important role, as people with a family history of either condition have a predisposition. Environmental triggers also come into play – exposure to certain toxins or pollutants may activate the disease pathway in those with a genetic vulnerability.
In terms of lifestyle, diet is one of the most significant risk factors. Diets high in processed foods, sugar, unhealthy fats, and low in fiber have been strongly associated with increased incidence of debeere and debrer. Obesity and being overweight are additional risk factors, as excess adipose tissue drives systemic inflammation. High stress levels and lack of exercise also correlate with greater risk. The immune system seems to be involved as well, as autoimmunity and imbalanced cytokine levels are often seen in debeere and debrer patients.
While more research is still needed, it’s clear that a combination of genetic, environmental, and lifestyle factors interact to determine someone’s susceptibility. By understanding and addressing modifiable risk factors like diet, activity levels, and stress, individuals may be able to reduce their chances of developing these conditions. Healthy eating, regular exercise, stress management, maintaining normal weight, and avoiding exposure to toxins are all recommended. Those with family history may consider genetic testing and take extra precautions. Increased awareness of risk factors empowers patients and physicians to make choices that can lower disease risk.
Distinguishing Key Differences Between Debeere and Debrer
While debeere and debrer share some similar characteristics, there are important differences between the two conditions that are critical to understand. Debeere primarily affects the liver and gastrointestinal system, whereas debrer most severely impacts the kidneys and cardiovascular system. The pathophysiology differs as well – debeere is characterized by abnormal fat deposits in the liver leading to inflammation and scarring. In contrast, debrer involves dysfunction of the glomerular filtration system in the kidneys. Genetically, they have distinct gene associations, with debeere linked to variants in genes regulating lipid metabolism, and debrer associated with genes controlling blood pressure and kidney function.
Clinically, the most prominent symptoms also diverge. Debeere often first presents with fatigue, abdominal discomfort, nausea, and jaundice. Debrer typically manifests with fluid retention, frequent urination, hypertension, and edema. While weight loss, appetite changes, and anemia can occur in both, the onset tends to be more rapid in debeere. In terms of diagnosis, debeere is identified via liver enzyme tests, imaging, and sometimes liver biopsy. Debrer is confirmed primarily through urine protein tests, eGFR, and kidney imaging studies.
Regarding treatment, the approaches differ significantly as well. Lifestyle changes involving diet, exercise, and abstinence from alcohol are cornerstones of treating debeere. Medications may include corticosteroids, immunosuppressants, or antivirals. Debrer management focuses on controlling hypertension and proteinuria through ACE inhibitors, ARBs, and diuretics. When kidney function declines severely in debrer, dialysis or transplantation may be required, whereas debeere progresses to cirrhosis and end-stage liver disease.
In summary, while both are serious chronic conditions, debeere and debrer have distinct mechanisms, symptoms, diagnostic criteria, and treatment protocols. Recognizing the key differences is vital for early and accurate diagnosis, so that patients can receive appropriate care based on the specific disease process involved.
Examining the Major Causes and Risk Factors of Debeere and Debrer
As complex conditions, debeere and debrer have a variety of genetic, lifestyle, and environmental factors that contribute to their development. Family history and genetic predisposition play a major causal role. Having a first-degree relative with either disease significantly raises one’s risk. Certain genetic variants, like those affecting lipid metabolism in debeere or blood pressure regulation in debrer, make individuals more susceptible.
Diet and nutrition status are also pivotal risk factors. Diets high in processed carbohydrates, added sugars, saturated fats, and sodium have been strongly linked to increased incidence of both diseases. These foods promote inflammation, insulin resistance, hypertension, and other effects that accelerate disease progression. Being overweight or obese also correlates to higher risk, as excess visceral fat causes metabolic dysfunction.
Environmental exposures can trigger these conditions as well. Toxins like pesticides, heavy metals, air pollution, and industrial chemicals are implicated in debeere and debrer. These compounds create oxidative stress, damage blood vessels, and disrupt normal cellular processes. Certain medications, like NSAIDs and chemotherapy drugs, can also lead to liver or kidney injury in sensitive individuals.
High stress levels, sedentary lifestyles, smoking, and excessive alcohol consumption further raise disease risk. Psychological stress activates inflammatory pathways and the sympathetic nervous system. Lack of exercise leads to insulin resistance, weight gain, and hypertension. Smoking and alcohol cause direct organ damage while depleting antioxidants.
In summary, while genes load the gun, lifestyle and environmental factors often pull the trigger when it comes to debeere and debrer. Addressing modifiable risk factors by adopting healthy diets, maintaining normal weight, exercising, limiting environmental exposures, and managing stress can help prevent these diseases despite genetic susceptibility.
Recognizing the Common Symptoms of Debeere and Debrer
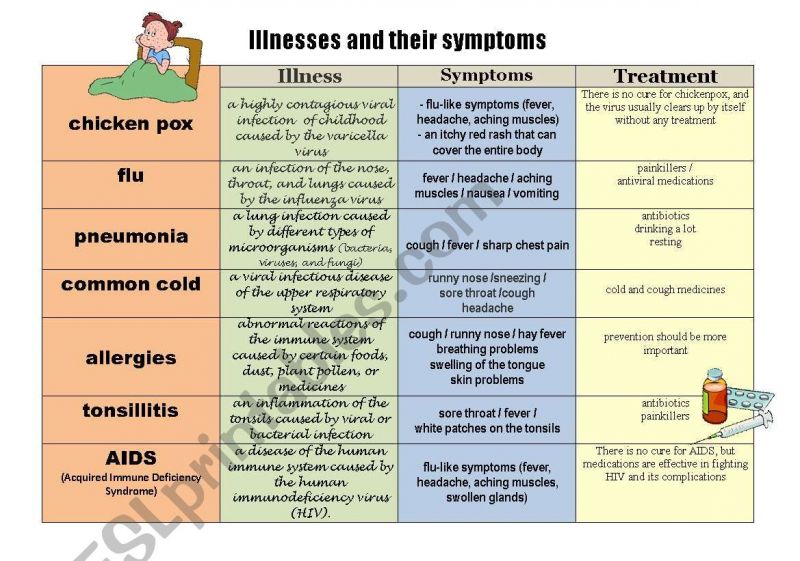
Being able to identify the characteristic symptoms of debeere and debrer is crucial for obtaining prompt diagnosis and treatment. While some generalized symptoms may overlap between the two diseases, there are also distinctive signs that set them apart.
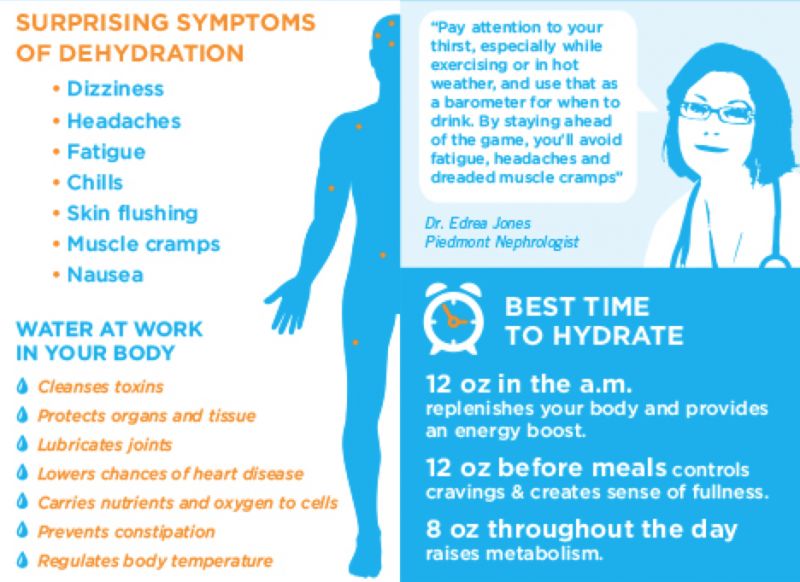
Fatigue and weakness are common early symptoms of both conditions. As liver or kidney function declines, the buildup of toxins and metabolic waste products leads to lack of energy. Weight loss or reduced appetite frequently occur as well, due to diminished nutrient absorption and metabolic disturbances. Abdominal swelling or discomfort may also be present.
People with debeere often develop a yellowing of the skin and eyes known as jaundice, indicating excess bilirubin from impaired liver function. Itching of the skin is also common. Patients may experience nausea, vomiting, or diarrhea due to gastrointestinal irritation. Dark urine and pale stool are other klassic signs.
Those with debrer frequently have puffy eyes and swelling in the hands and feet caused by fluid retention. Unexplained foamy or frothy urine is another peculiar symptom. High blood pressure often develops as kidney damage impairs sodium regulation. Shortness of breath can occur as fluid accumulates in the lungs.
While the earliest signs are often nonspecific, recognizing the unique manifestations of debeere versus debrer allows for more targeted diagnostic testing. Catching symptoms early and differentiating between the two diseases enables rapid treatment to halt progression and prevent complications. Public awareness of their distinct symptom profiles is essential.
Diagnostic Tests and Procedures for Debeere and Debrer

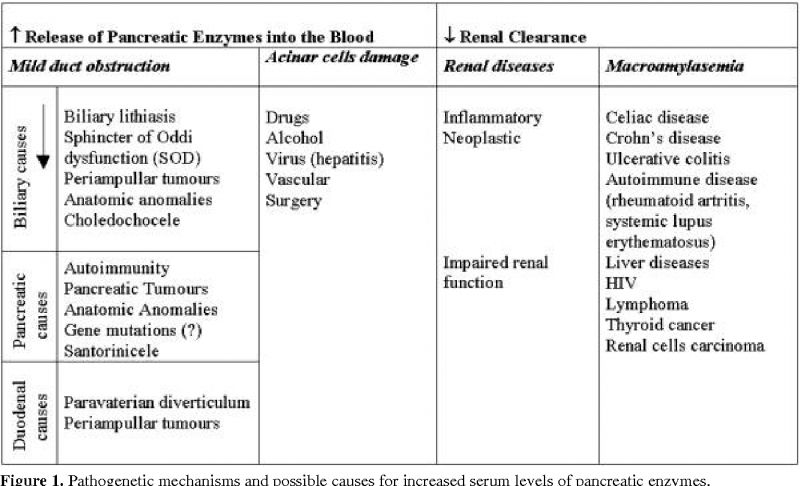
Getting an accurate diagnosis of debeere or debrer involves a combination of laboratory tests, imaging studies, and sometimes tissue biopsies. The different tests assess organ function, structure, and damage to pinpoint the specific disease.
Basic blood tests like complete blood count, metabolic panel, liver enzymes, and inflammatory markers provide important information in both diseases. Levels of bilirubin, albumin, ALT, AST, and ALP indicate liver function in debeere, while BUN, creatinine, and electrolytes reflect kidney status in debrer.
Imaging modalities like ultrasound, CT, and MRI scans give critical data on tissue structure. In debeere, they detect fat deposits, fibrosis, lesions, and cirrhosis in the liver. For debrer, imaging reveals kidney size, cysts, scarring, and other damage. Ultrasound with Doppler also evaluates blood flow.
Additional specialized tests offer more insights. Fibroscans use vibration waves to quantify liver stiffness from fibrosis in debeere. Biopsy of liver tissue is sometimes done to grade inflammation and staging. For debrer, urine is analyzed for levels of protein, blood, and sediment. Glomerular filtration rate is calculated from waste clearance kinetics.
No single test is definitive; diagnosis requires assessing multiple aspects of organ function and injury. With precise diagnostic criteria and testing protocols for debeere versus debrer, physicians can make accurate diagnoses even in complex cases. Advances in biomarkers and imaging will further improve sensitivity and specificity of diagnostic procedures in the future.
Conventional Treatment Options for Debeere and Debrer
Managing debeere and debrer involves a multifaceted approach addressing the underlying drivers of disease progression. Lifestyle modifications provide the foundation. Pharmaceuticals help control symptoms and complications. Regular medical monitoring is key for adjusting therapies.
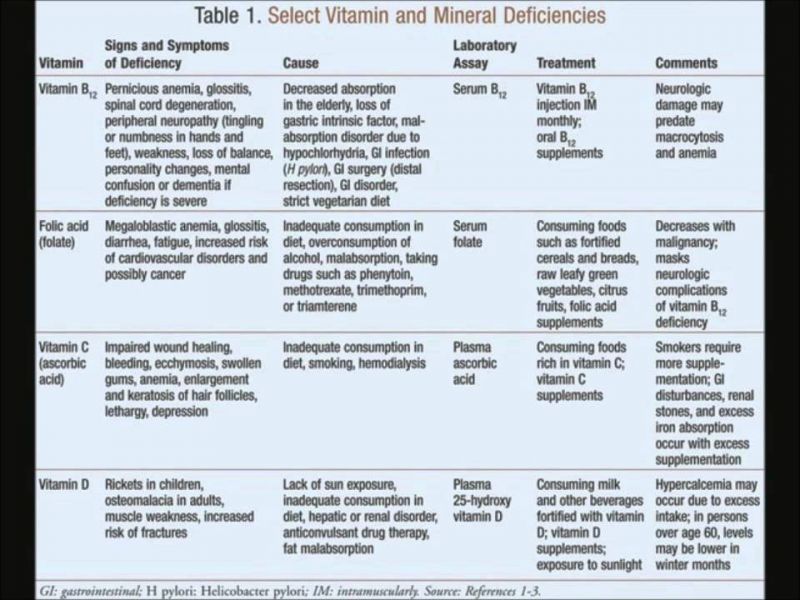
For debeere, abstaining from alcohol is imperative to limit further liver insult. Corticosteroids and immunosuppressants like prednisone, azathioprine, and cyclosporine reduce inflammation and autoimmune attack. Antiviral medications may be used if a hepatitis infection triggered liver injury. Vitamin supplements offset nutritional deficiencies common in debeere.
With debrer, the priority is preserving remaining kidney function. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) lower blood pressure while reducing protein in the urine. Diuretics manage fluid retention but must be used judiciously. Low protein diets are often recommended as well.
If kidneys fail completely in end-stage debrer, dialysis or transplantation are options. Peritoneal dialysis uses the abdomen to filter wastes. Hemodialysis relies on an external machine. Transplant swaps the diseased kidneys for a healthy donated organ. None fully replace normal kidney function but can sustain life.
For both diseases, regular checkups to monitor lab results, organ status, and medication side effects are essential. While current treatments cannot cure debeere or debrer, they can slow decline, manage complications, and extend life. Ongoing research strives to develop better tolerated and more effective therapies.
Latest Advances in Research for New Debeere and Debrer Therapies
Exciting progress is being made in understanding and treating debeere and debrer through cutting-edge scientific research. Novel medications, biologic agents, cell therapies, and nanotechnology are emerging from labs to clinical trials.
For debeere, new antifibrotic drugs slow or reverse scarring by targeting collagen production and matrix remodeling. Experimental drugs interrupt inflammatory pathways and apoptosis. Stem cell transplantation may enable liver regeneration. Nanoparticle delivery systems enhance bioavailability of medications.
In debrer, innovative immunosuppressants more selectively inhibit damaging immune processes while minimizing toxicity. Cell therapies utilizing mesenchymal stem cells show promise in reducing kidney inflammation. Gene therapies aim to correct aberrant DNA methylation underlying disease. Wearable or implantable biosensors allow real-time monitoring of kidney function.
Advanced filtration techniques are being engineered to improve dialysis efficiency and wearability for end-stage debrer. 3D bioprinting of kidney tissue may ultimately enable organ regeneration. Artificial intelligence is accelerating drug discovery and enabling personalized medicine approaches.
These emerging treatments target root causes of debeere and debrer with fewer side effects. While still early, such innovations offer hope for dramatically improving prognosis. With continued research, new therapeutic strategies transforming both the management and potential cure of these diseases are on the horizon.
Diet and Nutrition Recommendations for Debeere and Debrer
Diet and nutrition play a crucial role in managing debeere and debrer. The right foods can help control symptoms, support organ function, reduce complications, and slow disease progression. Nutrition should be a cornerstone of treatment.
For both conditions, limiting sodium, processed carbohydrates, and saturated fats is advised to reduce strain on the liver and kidneys. Lean proteins, complex grains, fruits, vegetables, and healthy fats nourish without promoting inflammation or obesity.
In debeere, restricting total calories can curb fat accumulation and weight gain. Limiting or avoiding alcohol prevents further liver toxicity. High fiber foods aid digestion to reduce GI symptoms. Supplements like milk thistle and vitamin D can help repair and protect liver tissue.
With debrer, reducing dietary potassium and phosphorus prevents abnormal mineral levels from damaged kidneys. Adequate protein intake maintains muscle mass but excess amounts accelerate kidney decline. Fluid restriction may be needed if output decreases.
Having a nutrition plan tailored to the specific condition allows patients to proactively optimize their diet. Registered dietitians can provide guidance on foods to emphasize or avoid. Supporting organ function through smart nutrition choices gives patients a sense of control in managing their disease.
Complications and Long-Term Effects of Debeere and Debrer
If left untreated or uncontrolled, debeere and debrer can lead to serious complications that negatively impact long-term health and quality of life. Being aware of these effects is important for seeking proper treatment.
In advanced debeere, extensive liver scarring culminates in cirrhosis and complete organ failure. This causes fluid retention, bleeding disorders, susceptibility to infections, and metabolic problems. Liver cancer risk also increases. If complications become life-threatening, liver transplant may be necessary.
With progressive debrer, chronic kidney disease leads to anemia, bone disease, malnutrition, and cardiovascular problems. Fluid overload strains the heart and lungs. Uremia results as wastes build up. Kidney failure requires lifelong dialysis or transplantation to sustain life.
Both diseases increase the risk of other conditions when organs are damaged. Debeere raises chances of diabetes, osteoporosis, and heart disease. Debrer is linked to hyperparathyroidism, gout, and hypertension. The emotional toll of serious illness can also negatively impact quality of life.
Prompt diagnosis and early management of debeere and debrer is imperative to halt progression before complications arise. Patients should be educated on potential long-term effects and work closely with their healthcare team to preserve health and prevent end-organ disease through vigilant monitoring and treatment.
Caring for Someone with Debeere or Debrer
Caring for a loved one with debeere or debrer poses challenges but also deepens relationships. As a caregiver, focus on educating yourself, providing emotional support, promoting treatment adherence, and maintaining your own self-care.
Learn all you can about your loved one’s disease – its symptoms, progression, treatment options, and needs. Accompany them to medical appointments to understand the care plan. Help keep track of medications, test results, and contact information for their healthcare providers.
Offer regular emotional support and encouragement through active listening and validating their feelings. Motivate them to stay positive and keep fighting the disease. Provide reassurance that you will be present through the ups and downs.
Gently remind them about proper diet, taking medications, exercise, and avoiding substances that could worsen their condition. Offer to assist with medical tasks like dressing changes, injections, or home dialysis. Help reduce sources of stress.
Don’t neglect your own self-care – maintain social connections, take time for activities you enjoy, and process your own emotions. Seek support through counseling or caregiver groups. Communicate honestly with your loved one about challenges. Caring for yourself enables you to be fully present as a caregiver.
With compassion, patience, education and teamwork, you can make the difficult journey with debeere or debrer more manageable for your loved one. Your support makes a meaningful difference.
Tips for Coping and Living Well with Debeere or Debrer
Receiving a diagnosis of debeere or debrer is life-altering. Adjusting mentally and emotionally while coping with symptoms can be very challenging. However, with the right strategies, many people learn to manage their disease and maintain a fulfilling quality of life.
Educate yourself fully about your condition through reliable sources, ask questions of your healthcare providers, and be actively involved in your treatment plan. Express your feelings and concerns to supportive loved ones and connect with others facing the same diagnosis.
Focus on the aspects of health you can control through diet, exercise, stress management, treatment adherence, and avoiding harmful substances. Set small, achievable goals you can work towards. Maintain a sense of purpose through hobbies, work, or volunteering if able.
Reduce stress through practices like meditation, yoga, nature walks, massage, or counseling. Get adequate rest and sleep. Seek ways to bring joy, humor, and laughter into each day. Join a support group to share wisdom and encouragement with others in a similar situation.
Remember there will be hard days physically and emotionally. Seek help from your support system on those days. Focus on progress and victories, rather than perceived setbacks. Be patient, kind and understanding with yourself. Don’t lose hope – many are now living long and fulfilling lives with debeere and debrer.
Support Groups and Resources for Debeere and Debrer Patients
Living with a chronic illness like debeere or debrer can feel isolating and overwhelming. Connecting with support groups and utilizing available resources can provide invaluable information, encouragement, and a sense of community.
Disease-specific nonprofits like the American Liver Foundation and American Kidney Foundation offer education, research updates, clinical trials, fundraising events, message boards, and local in-person support groups. These create meaningful opportunities to share experiences and advice.
Online communities through social media groups and forums enable connecting with others living with these diseases across geographical distances. Telehealth now also facilitates virtual support groups. Resources can be accessed 24/7 from home.
Support networks empower people to become advocates in their own care. Interacting with those further along in their diagnosis provides hope and wisdom to those newly diagnosed. Patients and loved ones gain perspective and realize they are not alone.
In addition to emotional support, practical resources include nutrition guides, financial aid, mental health services, transportation assistance, and more. Patients should be made aware of the range of services available locally and nationally. Support networks play a invaluable role in navigating life with chronic illness.
The Future Outlook for Debeere and Debrer Treatments
While debeere and debrer remain incurable diseases, the future outlook is encouraging thanks to expanding scientific knowledge and accelerated research on new therapies. There is hope that transformative treatments may emerge to dramatically improve prognosis.
Advanced medications, gene therapies, cell-based regenerative treatments, biomedical devices, and even organ bioengineering are progressing through clinical trials. Precision medicine approaches are enabling more tailored treatment based on the specific genetic and molecular characteristics of an individual’s disease.
Therapies in development aim to modify disease course by targeting underlying pathophysiologic mechanisms, rather than just managing complications. Some may be able to halt or reverse progression, potentially curing certain forms of debeere or debrer.
Artificial intelligence and advanced data analytics are rapidly enhancing diagnostic capabilities, treatment predictions, and acceleration of drug discovery. Biomarker research also holds promise for early disease detection and monitoring.
While realizing such advances takes years, exciting progress is underway. Patients should view debeere and debrer as manageable conditions given proper medical care and lifestyle changes. Maintaining optimism and hope allows positive outlooks despite current limitations in treatments.
Lowering Your Risk and Preventing Debeere and Debrer
While some risk factors for debeere and debrer like genetics cannot be changed, many evidence-based strategies can reduce your chances of developing these diseases.
Maintain a healthy body weight through diet and exercise. Follow a balanced eating pattern high in fruits, vegetables, whole grains, lean proteins and healthy fats. Limit sodium, added sugars, saturated fats, and processed foods. Stay well hydrated.
Be physically active on most days, incorporating both cardio and strength training. Get at least 7-9 hours of quality sleep per night. Manage stress levels through relaxation practices and social support.
Avoid or limit alcohol consumption, especially if you have a family history of liver disease. Don’t start smoking or quit if you currently smoke. Be vigilant about medications and supplements that could impact your liver or kidneys.
Take precautions around chemical or environmental exposures by using protective equipment at work, avoiding contact with toxins, and limiting pollution in your home. Stay up to date on vaccinations and see your provider for regular wellness visits.
Being proactive with lifestyle habits and regular medical care gives you the best chance at staying healthy and avoiding deveere and debrer. However, if diagnosed, early detection and treatment enables positive outcomes. Prevention plus vigilance provides peace of mind.