What is gait torque and why does it matter. How does gait torque affect stability and injury risk. How can optimizing gait torque reduce head wobble and fall risk. What are effective methods to improve gait torque. How does gait re-training and physical therapy help optimize gait torque. What other factors contribute to enhanced gait and fall risk reduction. How does gait analysis benefit performance and injury prevention.
Understanding Gait Torque and Its Importance
Gait torque is a crucial component of human locomotion that refers to the rotational forces exerted on the body during walking or running. These twisting forces play a vital role in maintaining balance, stability, and overall gait efficiency. But why is gait torque so important?
Proper gait torque is essential for:
- Maintaining balance and stability while in motion
- Reducing the risk of injuries during walking or running
- Optimizing overall performance in various physical activities
- Ensuring smooth and coordinated movement patterns
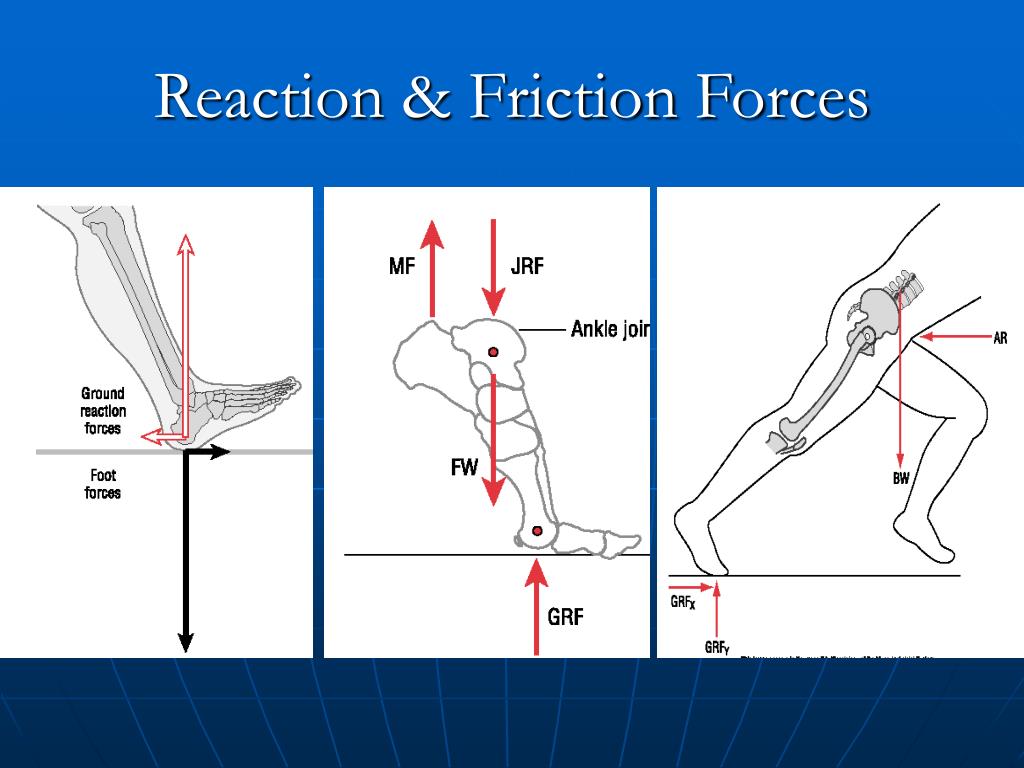
As we move, our legs and feet generate both linear forces that propel us forward and rotational forces that keep us balanced. These rotational forces constitute the torque component of our gait. The right amount of gait torque is crucial for efficient and safe movement, while too much or too little can lead to various problems.
The Impact of Gait Torque on Stability and Injury Risk
How does gait torque affect our stability and potential for injury? The relationship between torque, stability, and injury risk is complex and multifaceted.
Optimal Gait Torque
When gait torque is optimal, it contributes to:
- Maintaining a stable and upright posture during locomotion
- Preventing excessive side-to-side motion of the head and torso
- Smoothing out acceleration forces on joints and tissues
- Enhancing overall balance and coordination
Excessive Gait Torque
What happens when gait torque is too high? Excessive torque can lead to:
- Increased side-to-side wobbling of the head and torso
- Challenges to balance and coordination
- Greater stress on muscles, tendons, and ligaments
- Higher risk of injuries due to overcompensation
Insufficient Gait Torque
Conversely, insufficient gait torque can result in:
- Uncoordinated flailing of the torso and limbs
- Difficulty maintaining balance and smooth acceleration
- Increased risk of tissue injuries over time
- Reduced overall stability during movement
Reducing Head Wobble and Fall Risk Through Optimized Gait Torque
Can optimizing gait torque really make a difference in reducing head wobble and fall risk? The answer is a resounding yes. By fine-tuning gait torque, we can achieve numerous benefits:
- A smoother, more stable, and controlled gait pattern
- Reduction in excessive head bobbing or side-to-side wobbling
- Lower impact loading rates on joints and tissues
- Improved balance and coordination, especially crucial for older adults
- Decreased risk of falls due to enhanced stability
Research has shown a strong link between excessive head wobble during walking and an increased risk of falls, particularly in older populations. Therefore, optimizing gait torque and improving overall stability is a key strategy in fall prevention programs.
Effective Methods to Improve Gait Torque
If you’ve noticed excessive head and torso wobbling or balance challenges while walking, it may be time to focus on improving your gait torque. Here are some effective strategies to optimize your gait torque alignment:
- Seek a professional gait analysis to identify specific torque issues
- Practice hip hinging drills to enhance stability and control
- Engage in single-leg balance exercises to improve overall balance
- Strengthen your core and hip muscles to enhance control during movement
- Improve flexibility in key areas that affect gait
- Utilize biofeedback tools that provide cues for proper torque alignment
- Practice self-cueing techniques to smooth out your stride and minimize wobbling
- Consider the use of orthotics or shoe modifications to optimize torque alignment
Implementing these strategies can significantly improve your gait torque and overall stability. However, it’s important to remember that individual needs may vary, and consulting with a professional can help tailor these methods to your specific requirements.

The Role of Gait Re-Training and Physical Therapy in Optimizing Gait Torque
How can gait re-training and physical therapy contribute to improving gait torque? These specialized approaches offer targeted interventions to address underlying issues and optimize gait mechanics.
Benefits of Working with a Physical Therapist
- Identification and correction of muscle imbalances
- Addressing joint restrictions that may affect gait
- Correction of faulty movement patterns
- Customized gait re-training drills and exercises
- Long-term improvement in gait torque
Gait Re-Training Techniques
Physical therapists employ various techniques to improve gait torque, including:
- Walking practice with proper posture on lines or tiles
- Verbal cues to smooth out stride and optimize foot placement
- Use of mirrors for visual feedback on alignment
- Prescription of targeted strength and flexibility exercises
- Assessment for custom orthotics or assistive devices
These interventions provide a strong foundation for balanced and smooth walking, addressing the root causes of gait torque issues rather than just treating symptoms.
Comprehensive Approaches to Enhance Gait and Reduce Fall Risk
While optimizing gait torque is crucial, it’s just one piece of the puzzle when it comes to improving walking stability and reducing fall risk. What other factors should be considered in a comprehensive approach?
Additional Strategies for Gait Improvement and Fall Prevention
- Enhancing overall lower body strength and mobility
- Incorporating dual-tasking walking drills (e.g., walking while counting)
- Practicing challenging walking patterns like tandem or backward walking
- Addressing vision, inner ear, or neurological issues affecting balance
- Implementing environmental modifications to minimize fall hazards
- Regular cardiovascular exercise to improve overall fitness and endurance
- Nutrition interventions to support bone and muscle health
A comprehensive fall prevention program should address gait torque optimization alongside these other exercise, medical, and environmental factors that influence stability and fall risk. This holistic approach ensures that all aspects of gait and balance are addressed, providing the best possible outcomes for individuals at risk of falls.

Gait Analysis for Enhanced Performance and Injury Prevention
How can gait analysis benefit athletes and active individuals looking to improve performance and reduce injury risk? Sophisticated gait analysis techniques offer valuable insights for optimizing movement efficiency and preventing injuries.
Benefits of Advanced Gait Analysis
- Identification of torque imbalances that may hamper efficiency
- Detection of movement patterns that increase injury likelihood
- Customized recommendations for improving torque alignment
- Insights into power generation and transfer during movement
- Targeted interventions to enhance overall performance
High-level trainers and therapists utilize cutting-edge technology to conduct detailed gait analyses. These assessments can reveal subtle inefficiencies or imbalances that may not be apparent to the naked eye, allowing for precise interventions to optimize gait torque and overall movement mechanics.
Applications in Sports and Active Lifestyles
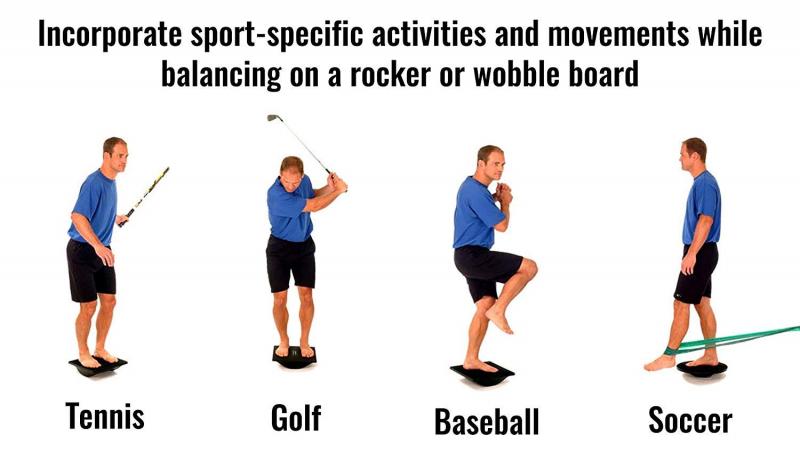
Gait analysis and torque optimization are particularly valuable for:
- Runners seeking to improve efficiency and reduce injury risk
- Team sport athletes looking to enhance agility and change of direction
- Endurance athletes aiming to optimize energy expenditure
- Individuals recovering from lower limb injuries
- Anyone engaged in activities requiring repetitive lower body movements
By identifying and addressing gait torque issues, athletes and active individuals can not only reduce their risk of injury but also potentially unlock new levels of performance in their chosen activities.
Implementing Gait Torque Optimization in Daily Life
How can individuals incorporate gait torque optimization into their daily routines? Integrating these principles doesn’t have to be complicated or time-consuming. Here are some practical tips:
- Practice mindful walking, focusing on smooth, controlled movements
- Incorporate balance exercises into your regular workout routine
- Use everyday activities as opportunities to challenge your balance (e.g., standing on one foot while brushing teeth)
- Regularly assess and replace worn-out footwear
- Maintain good posture throughout the day, not just during walking
- Stay active and engage in a variety of physical activities to challenge your body in different ways
By making these small changes and remaining conscious of your gait, you can gradually improve your gait torque and overall stability over time.

The Importance of Consistency and Patience
Improving gait torque and overall stability is not an overnight process. It requires consistent effort and patience. However, the benefits of improved balance, reduced fall risk, and enhanced performance make this investment in your movement health worthwhile.
Remember, progress may be gradual, but even small improvements can have significant impacts on your overall quality of life and ability to engage in physical activities safely and effectively.
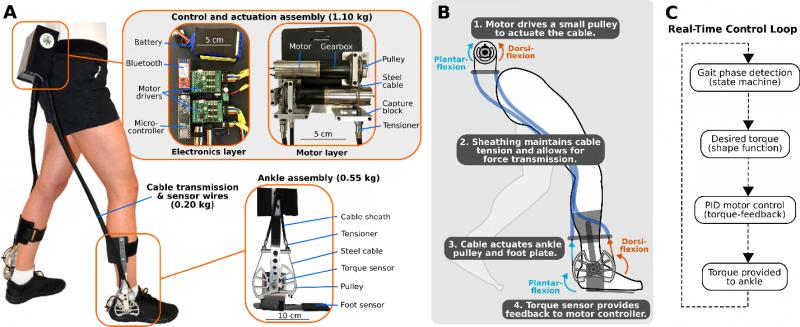
Technological Advancements in Gait Torque Assessment and Training
How is technology shaping the future of gait torque optimization? Recent advancements have opened up new possibilities for assessing and improving gait mechanics.
Innovative Tools for Gait Analysis
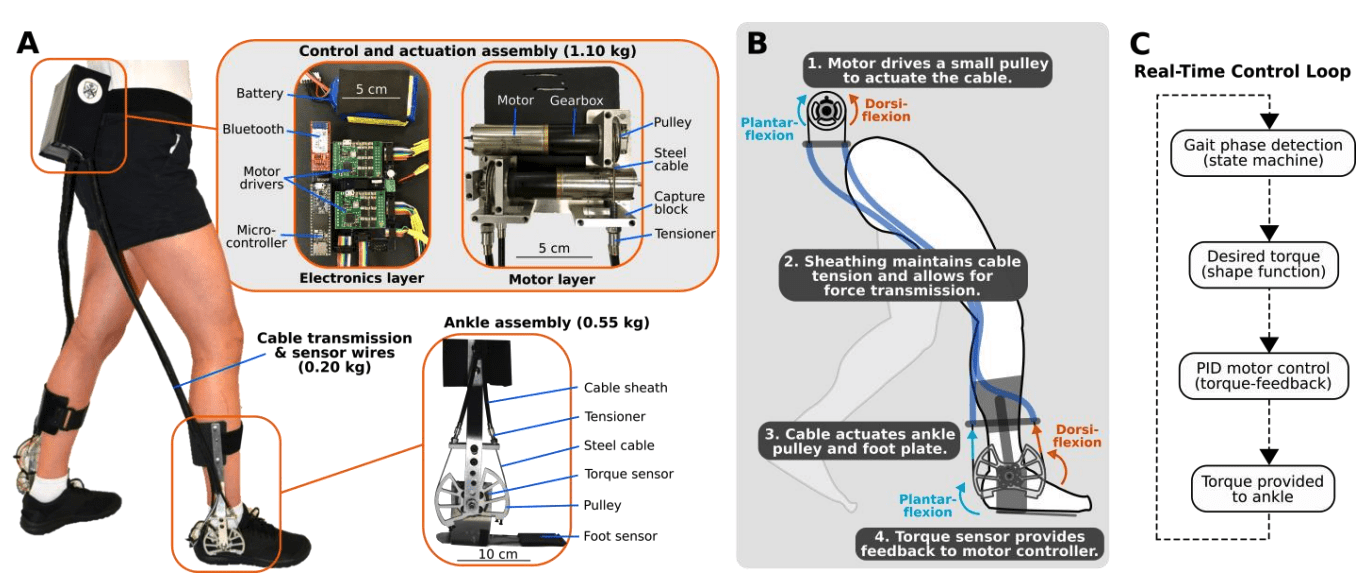
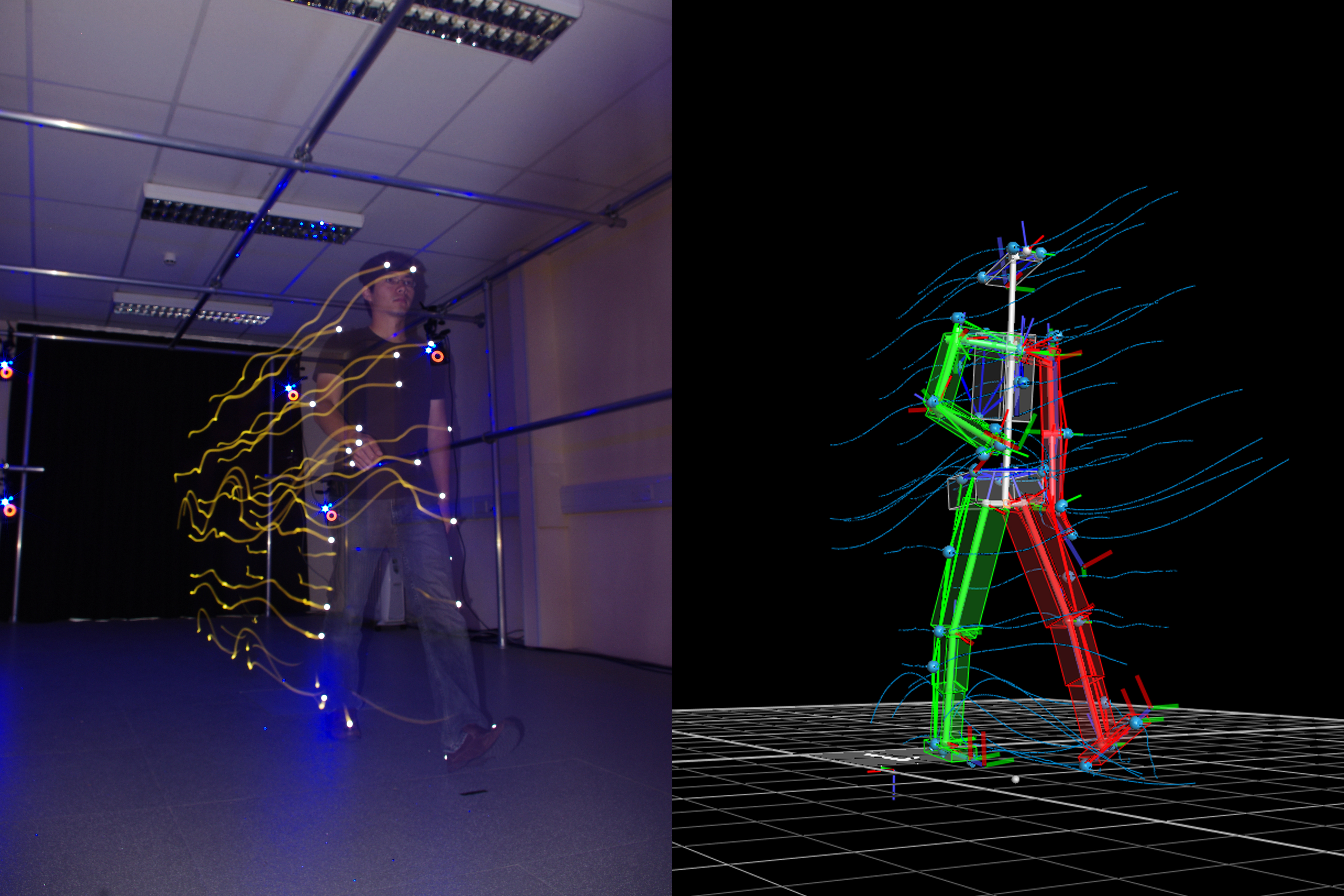
- Wearable sensors that provide real-time feedback on gait patterns
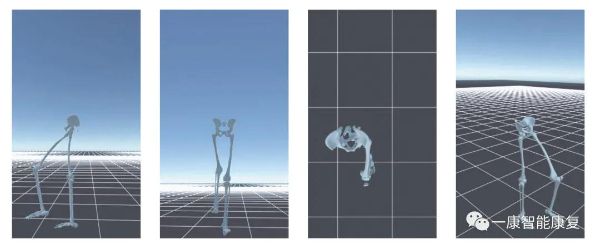
- 3D motion capture systems for detailed analysis of body movements
- Force plate treadmills that measure ground reaction forces during walking or running
- Smartphone apps that use built-in accelerometers to assess basic gait parameters
- Virtual reality systems for immersive gait training experiences
These technologies are making sophisticated gait analysis more accessible, allowing for more precise interventions and personalized training programs.
The Role of Artificial Intelligence in Gait Optimization
Artificial intelligence (AI) is playing an increasingly important role in gait analysis and optimization. AI algorithms can:
- Analyze vast amounts of gait data to identify subtle patterns and anomalies
- Predict potential injury risks based on gait characteristics
- Generate personalized training recommendations
- Adapt and evolve training programs based on individual progress
As these technologies continue to develop, we can expect even more precise and effective methods for optimizing gait torque and improving overall movement quality.
The Broader Impact of Gait Torque Optimization
Why does gait torque optimization matter beyond individual health and performance? The implications of improved gait mechanics extend to various aspects of society and healthcare.
Public Health Benefits
- Reduced healthcare costs associated with fall-related injuries
- Improved mobility and independence for aging populations
- Enhanced quality of life for individuals with movement disorders
- Potential reduction in chronic pain conditions related to poor gait mechanics
Implications for Occupational Health and Safety
Optimized gait torque can also have significant benefits in workplace settings, particularly in industries that require extensive walking or standing. Improved gait mechanics can lead to:
- Reduced risk of workplace injuries
- Improved productivity and efficiency
- Decreased absenteeism due to gait-related issues
- Enhanced overall employee well-being
By recognizing the broader impact of gait torque optimization, we can appreciate its potential to contribute to healthier, more active communities and workplaces.
Future Directions in Gait Torque Research and Application
What does the future hold for gait torque optimization? As our understanding of human movement continues to evolve, several exciting areas of research and application are emerging:
Emerging Research Areas
- Integration of neuroscience and biomechanics for deeper insights into gait control
- Exploration of the relationship between gait torque and cognitive function
- Development of more sophisticated predictive models for injury risk and performance
- Investigation of gait torque optimization in extreme environments (e.g., space exploration)
Potential Future Applications
The principles of gait torque optimization may find applications in diverse fields:
- Robotics and prosthetics design for more natural human-like movement
- Urban planning and architecture to create more movement-friendly environments
- Sports equipment design for enhanced performance and safety
- Rehabilitation protocols for neurological conditions affecting gait
As research in this field progresses, we can anticipate even more innovative approaches to understanding and optimizing human movement, with far-reaching implications for health, performance, and quality of life.
What Is Gait Torque And Why It Matters
Gait torque refers to the twisting or rotational forces exerted on the body during walking or running. Proper gait torque is important for maintaining balance and stability, reducing injury risk, and optimizing performance.
As we walk or run, our legs and feet exert both linear forces that propel us forward as well as rotational or twisting forces that keep us balanced. The rotational forces are the “torque” components of gait. Too much or too little gait torque can cause problems.
How Gait Torque Affects Stability and Injury Risk
Ideal gait torque helps keep the body stable and upright while walking and running. Proper torque prevents excessive side-to-side motion or wobbling of the head and torso during each step. It also smooths out acceleration forces on the joints and tissues.
However, if gait torque is too high or too low, it can lead to poor stability and increased injury risk. Excessive torque causes the head and torso to wobble more side-to-side with each step. This challenges balance and coordination. It also puts greater stress on the muscles, tendons, and ligaments to control these movements.
Insufficient gait torque allows the torso and limbs to flail about more freely in an uncoordinated manner. This makes maintaining balance and smooth acceleration much harder on the tissues. The end result is often injuries over time.
Optimizing Gait Torque Reduces Head Wobble and Fall Risk

By optimizing gait torque, we can achieve a smoother, more stable and controlled gait pattern. This reduces excessive head bobbing or wobbling side-to-side with each step. Proper gait torque alignment also lowers impact loading rates on the joints and tissues, reducing injury risk.
Additionally, smooth and controlled motion achieved through proper gait torque helps maintain balance and coordination. This is especially important in older adults who are at higher risk of falls. Excessive head wobble during walking is linked to increased risk of falls. Optimizing gait torque and stability is an important fall prevention strategy.
How to Improve Your Gait Torque
If you notice excessive head and torso wobbling or balance challenges when you walk, your gait torque may need improvement. Here are some tips to optimize gait torque alignment:
- Get a gait analysis to identify torque issues. Physical therapists can evaluate your gait and recommend specific exercises or drills.
- Practice hip hinging drills and single-leg balance exercises to improve stability.
- Work on core and hip strength and flexibility to enhance control.
- Use biofeedback tools that cue proper torque alignment during walking.
- Try cueing yourself to smooth out your stride and minimize wobbling.
- Consider orthotics or shoe modifications to optimize torque alignment.
Gait Re-Training and Physical Therapy
Working with a physical therapist to correct underlying muscle imbalances, joint restrictions, or movement pattern faults is key for improving gait torque long-term. They will guide you through proper gait re-training drills and exercises tailored to your needs.
For example, they may have you practice walking with proper posture on lines or tiles to optimize foot placement and torque alignment. Or they may use verbal cues during walking to smooth out your stride. Mirrors providing visual feedback on alignment can also help re-train optimal gait mechanics.
In addition, they will prescribe strength and flexibility exercises to improve control of your hips, core, and lower body. This gives you a strong foundation for balanced and smooth walking. They can also determine if custom orthotics or other assistive devices could improve your gait torque.
Other Ways to Enhance Gait and Reduce Fall Risk
Optimizing gait torque alignment is one important piece of improving walking stability and injury resilience. But there are other aspects of gait and fall risk reduction to consider as well, including:
- Improving overall lower body strength and mobility
- Working on dual-tasking walking drills (e.g. walking while counting)
- Practicing tandem or backward walking
- Addressing vision, inner ear or neurological issues affecting balance
- Making environmental modifications to minimize fall hazards
A comprehensive fall prevention program would address gait torque optimization as well as these other exercise, medical, and environmental factors that affect stability and fall risk.
Gait Analysis for Performance and Injury Prevention
Finally, gait torque evaluation and training is also crucial for athletes and active individuals looking to enhance performance and reduce injury risk. Excessive torque or torque imbalances can hamper efficiency and raise injury likelihood.
High-level trainers and therapists use sophisticated gait analysis to identify opportunities to improve torque alignment, power generation, and smooth acceleration in runners and other athletes. Fine-tuning gait torque is key for achieving excellence in sport as well.
So whether you are an older adult concerned about falls, a weekend warrior trying to avoid injuries, or an elite athlete pursuing that extra competitive edge, understanding and optimizing your gait torque is essential. A focused training program tailored to your needs by a physical therapist or trainer can help unlock safer, stronger, and higher performing movement patterns.
Measuring Gait Torque To Identify Imbalances
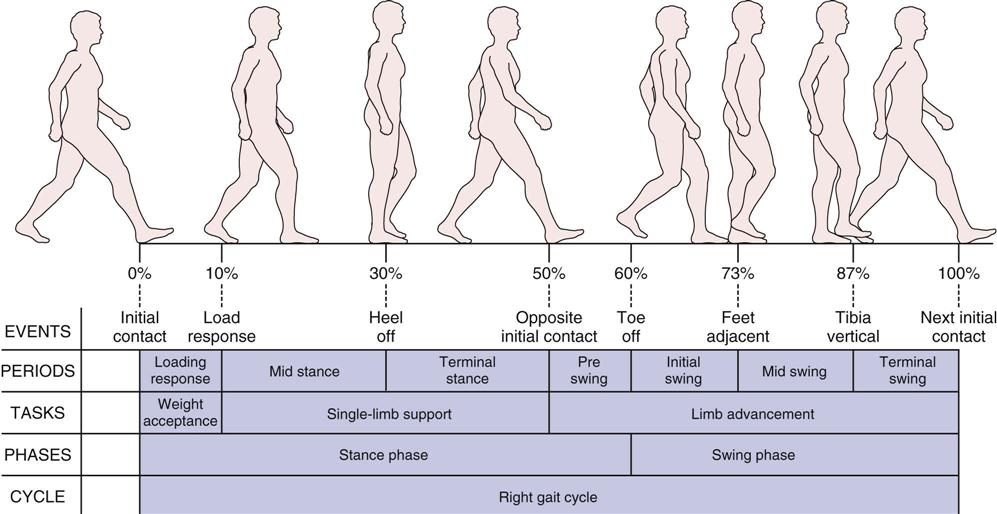
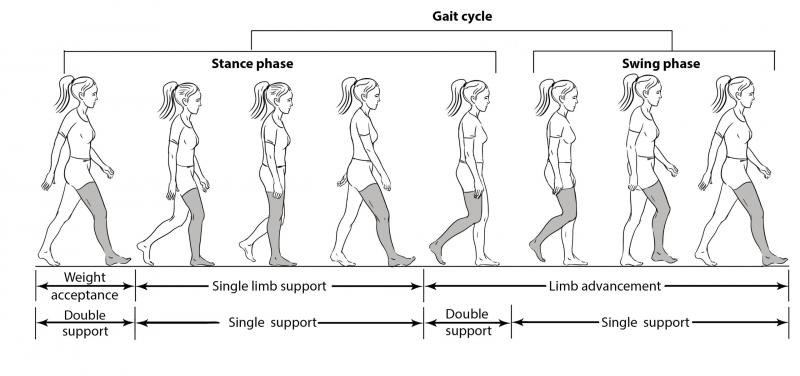
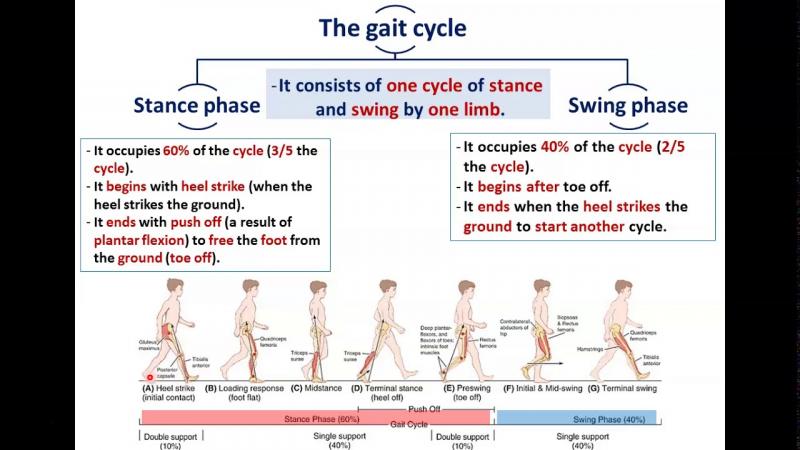
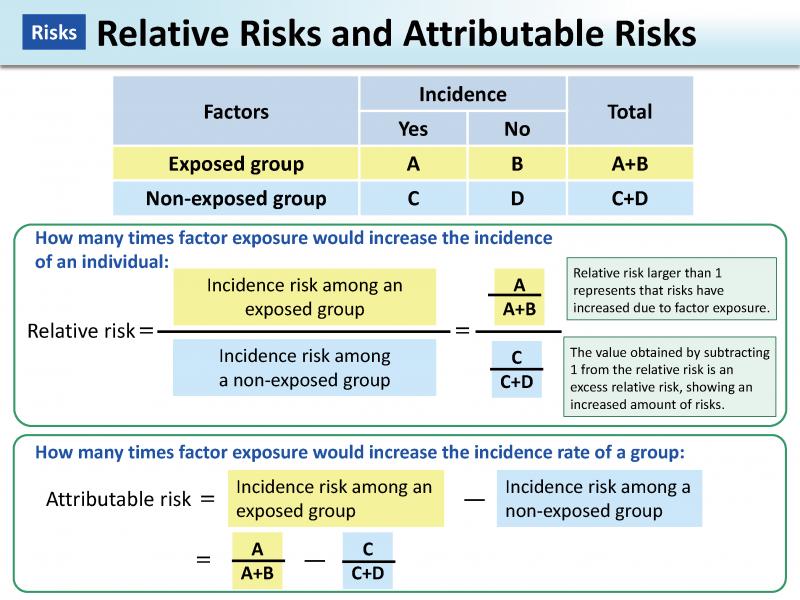
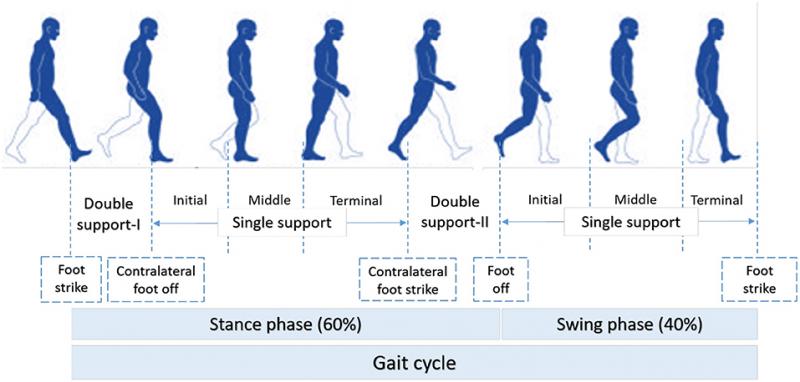
Walking seems like such a simple task, but it actually requires intricate coordination between multiple muscle groups to propel the body forward. With each step, the leg must rotate with enough power to provide forward momentum while also maintaining stability. This rotation generates torque – a rotational force that can be measured to gain insight into muscle activation patterns and detect potential imbalances. Understanding gait torque has important implications for identifying injury risks, monitoring rehabilitation progress, and optimizing sports performance.
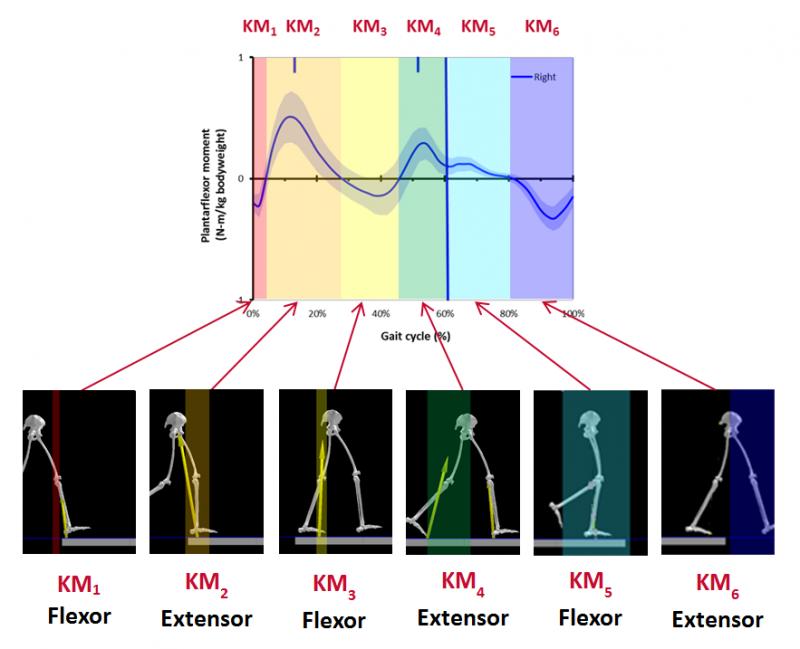
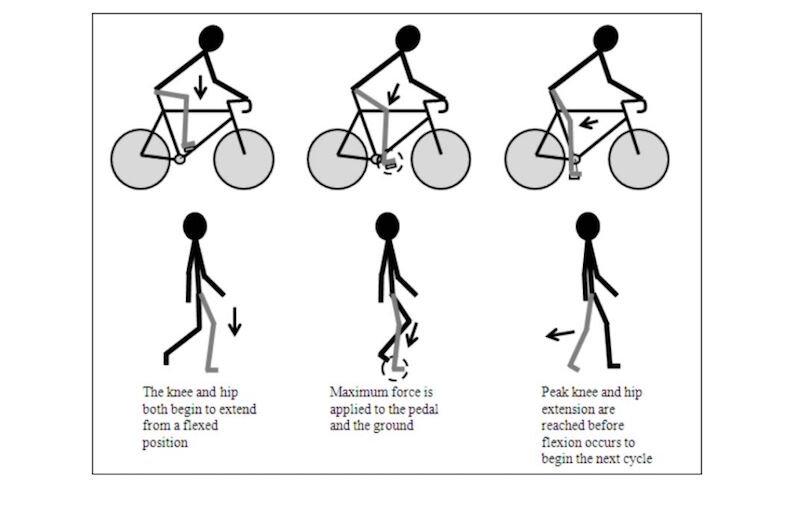
Gait analysis focuses on measuring biomechanical factors during walking, including joint angles, ground reaction forces, muscle activity, and torque. Torque refers to the twisting force generated when muscles contract to rotate a joint. Measuring torque provides direct insight into the intensity of muscle contractions during gait. For example, higher torque at the hip and knee joints indicates stronger activation of gluteal and quadriceps muscles to propel the leg forward.
Torque measurements can reveal left/right muscle activation imbalances that may increase injury risk. For example, if one leg generates significantly lower hip torque, it suggests weakened gluteal muscles that could lead to knee or hip pain. Rehabilitation specialists use gait torque analysis to identify specific deficiencies and target strengthening exercises. Monitoring torque over time also helps track progress in regaining symmetrical muscle activation patterns.
Beyond injury screening, gait torque has important applications in sports training. Torque profiling can detect muscle firing inconsistencies between legs that may hamper performance. Trainers utilize this data to develop drills that enhance symmetrical power generation. Optimizing torque output allows athletes to maximize speed and efficiency.
Measuring gait torque requires specialized equipment to track joint motion and forces. Treadmills with embedded force plates are commonly used along with 3D motion capture systems. Small sensors are placed on the legs to track joint angles while walking. Force plates record ground reaction forces generated with each step. Computer processing combines this data to calculate net torque around each joint.
Wearable sensor technology now allows torque analysis outside the lab. Compact inertial measurement units with accelerometers and gyroscopes can track limb and joint kinematics. Combined with machine learning algorithms, these sensors can estimate torque measures and asymmetry. This makes continuous gait monitoring possible in real-world settings.
However, some limitations remain in gait torque testing. Soft tissue motion can introduce error in joint angle measures, affecting torque calculations. It also provides only a snapshot of straight-line walking and may not reveal issues with multi-directional movements. Therefore, torque measures should be considered alongside other aspects of gait analysis for the most complete picture.
Improve Your Gait: How Adjusting Torque Reduces Head Wobble And Fall Risk

As we age, changes in our walking pattern often lead to increased upper body movement, or ‘head wobble’. Excessive side-to-side head motion while walking not only looks unstable but can indicate impairments that raise fall risk. The underlying cause typically involves reduced torque, or rotational force, generated in the lower limbs. Understanding the relationship between gait torque deficiencies and increased head oscillation provides key insights for improving stability.
Healthy smooth gait relies on optimal coordination between multiple muscle groups to efficiently propel the body forward. The gluteal and quadriceps muscles generate forward torque around the hip and knee joints, controlling acceleration of the leg into swing phase. Weakness in these muscles reduces torque, disrupting the normal walking rhythm.
With low propulsion torques, the center of mass rises and falls with each step instead of following a steady trajectory. The trunk and upper body must work harder to counteract these excessive vertical movements. This often leads to increased rotation of the head and unstable side-to-side wobbling.
Studies show that aging adults who display greater head oscillation during gait tend to have decreased torque around the hip and knee. This link persists even when controlling for walking speed, indicating the specific role of torque deficits. The resulting unsteadiness significantly increases risk of falls and resulting injuries.
Fortunately, targeted exercises to improve torque generation can help reestablish efficient gait patterns and reduce head wobble. Training protocols focus on strengthening the gluteal and quadriceps muscles using resistance bands, free weights, or body weight. Monitoring head acceleration and torque measures provides objective feedback on progress.
Assistive walking devices can also help compensate for muscle weakness. Nordic poles enhance stability during gait by increasing ground force application. Other aids like braces or prosthetics are engineered to optimize torque generation. Maximizing torque reduces destabilizing vertical movements, translating to smoother walking.
In summary, age-related gait instabilities often arise from reduced torque output in the lower limbs. This results in excessive upper body motion, seen as increased head wobble. Corrective interventions aimed at improving propulsion torques can reestablish efficient gait patterns and improve stability. Analyzing torque generation provides insights for targeted rehabilitation to reduce fall risk.
How Excessive Torque Causes Head Instability
During walking, the body must coordinate numerous muscles to smoothly accelerate the limbs and propel the body forward. Proper control of torque, the rotational force generated by muscles, is crucial for maintaining head stability. However, impaired neuromuscular activation can lead to excessive torque production, resulting in increased head wobble and oscillations. Understanding this relationship has important implications for improving balance and reducing fall risk.
Healthy gait relies on optimized torque patterns to ensure a steady trajectory of the head and trunk. As the leg swings forward, the hip flexors and quadriceps generate torque to accelerate the limb. At the same time, the gluteal muscles produce torque to extend the hip, providing forward propulsion. Coordinated contractions finely control the torque, minimizing disruptive forces.
Some neurologic conditions impair this coordination, leading to abnormal torque production. For example, Parkinson’s disease is characterized by insufficient hip flexor torque when initiating swing phase. Conversely, hemiplegia after stroke can involve excessive torque from hip hiking compensations.
Uncontrolled torque destabilizes the upper body by causing excessive rotation and displacement of the center of mass. With each step, the head and trunk must work harder to counteract abnormal angular momentum, resulting in greater oscillations. This is seen as increased wobbling of the head, which appears unstable and increases exertion.
Research quantifying head acceleration shows higher peak angular velocities in Parkinson’s disease patients, indicating more rapid twisting. Stroke survivors also display greater range of head motion compared to healthy controls. These instability patterns directly relate to underlying torque irregularities in the lower limbs.
Excessive head oscillations significantly increase fall risk since it becomes difficult to maintain visual focus and orient the body relative to the environment. Not surprisingly, greater head acceleration correlates strongly with impaired balance control during gait tasks. Reducing torque abnormalities is therefore a key target for rehabilitation.
Physical therapy exercises focus on strengthening muscles to improve torque control. Rhythmic auditory cueing helps establish coordinated motor patterns. Assistive walking devices provide external stabilization of the trunk and optimize torque generation through the hips and knees.
Wearable sensors that track head movements now enable real-time biofeedback during gait retraining. Monitoring progress in reducing torque-related oscillations helps fine tune interventions and maximize improvements in stability.
In summary, precise coordination of muscular torque is required for steady head motion during gait. Certain conditions impair this control, leading to excessive torque production and destabilizing head wobble. Targeted rehabilitation aims to improve torque regulation and minimize disruptive oscillations that elevate fall risk.
Improve Your Gait: How Adjusting Torque Reduces Head Wobble And Fall Risk
As we age, changes in our walking pattern often lead to increased upper body movement, or ‘head wobble’. Excessive side-to-side head motion while walking not only looks unstable but can indicate impairments that raise fall risk. The underlying cause typically involves reduced torque, or rotational force, generated in the lower limbs. Understanding the relationship between gait torque deficiencies and increased head oscillation provides key insights for improving stability.
Healthy smooth gait relies on optimal coordination between multiple muscle groups to efficiently propel the body forward. The gluteal and quadriceps muscles generate forward torque around the hip and knee joints, controlling acceleration of the leg into swing phase. Weakness in these muscles reduces torque, disrupting the normal walking rhythm.
With low propulsion torques, the center of mass rises and falls with each step instead of following a steady trajectory. The trunk and upper body must work harder to counteract these excessive vertical movements. This often leads to increased rotation of the head and unstable side-to-side wobbling.
Studies show that aging adults who display greater head oscillation during gait tend to have decreased torque around the hip and knee. This link persists even when controlling for walking speed, indicating the specific role of torque deficits. The resulting unsteadiness significantly increases risk of falls and resulting injuries.
Fortunately, targeted exercises to improve torque generation can help reestablish efficient gait patterns and reduce head wobble. Training protocols focus on strengthening the gluteal and quadriceps muscles using resistance bands, free weights, or body weight. Monitoring head acceleration and torque measures provides objective feedback on progress.
Assistive walking devices can also help compensate for muscle weakness. Nordic poles enhance stability during gait by increasing ground force application. Other aids like braces or prosthetics are engineered to optimize torque generation. Maximizing torque reduces destabilizing vertical movements, translating to smoother walking.
In summary, age-related gait instabilities often arise from reduced torque output in the lower limbs. This results in excessive upper body motion, seen as increased head wobble. Corrective interventions aimed at improving propulsion torques can reestablish efficient gait patterns and improve stability. Analyzing torque generation provides insights for targeted rehabilitation to reduce fall risk.
Reducing Torque Smooths Out Your Walking Motion
Walking is a complex task that requires coordinated muscle activations to propel the body forward. The forces generated by muscles during gait produce torque, or rotational force, around the joints. Excessive torque can lead to unstable movements and increase injury risk. That’s why controlling and reducing torque is key for smoothing out your natural walking motion.
Healthy smooth gait relies on the right amount of torque at the right time. As you shift your weight to one leg, the hip abductors on the stance side fire to stabilize the pelvis. Meanwhile, hip flexors and quadriceps muscles generate torque to accelerate the swinging leg. Well-timed contractions finely control torque for optimal forward momentum.
Sometimes muscle weakness or improper firing reduces torque generation, causing an unsteady gait. The legs seem to waver side-to-side, and maintaining balance becomes difficult. This not only feels unstable but can lead to falls or joint pain over time.
On the other hand, excessive muscular torque has a similarly destabilizing effect. Conditions like spasticity or dystonia cause muscles to contract too forcefully, creating excessive torque. This disrupts the normal rhythmic patterns of gait, causing abrupt accelerations and decelerations.
Uncontrolled torque throws off the smooth up-and-down motion of the center of mass. The upper body is forced to work harder to dampen these irregular movements. This often translates into a lurching gait that lacks fluidity.
Thankfully, several strategies can help regulate torque and establish smoother walking mechanics. Targeted strengthening exercises improve neuromuscular control, allowing muscles to generate just the right amount of torque when needed. Stretching increases range of motion and flexibility for better torque modulation.
Assistive devices like braces or walking aids provide external support to guide the leg’s swing path and trajectory. This enhances stability while reducing excessive torque from underlying muscle issues. Some emerging exoskeleton technologies even use robotic motors to augment human joint torque as needed.
Physical therapy taps into the nervous system’s innate plasticity. Sensorimotor feedback training helps reestablish optimal patterns of muscular torque generation. With improved coordination, gait becomes steadier and more fluid.
Analgesics and muscle relaxants can temporarily reduce abnormal muscle torque output. However, addressing the root neuromuscular imbalance is key for lasting improvements in gait quality.
In summary, optimizing torque production is essential for smoothing out natural walking mechanics. When muscles generate coordinated torque patterns, it allows for efficient acceleration and deceleration of the legs. Regulating torque enhances stability and fluidity, reducing pain and injury risk.
Improve Your Gait: How Adjusting Torque Reduces Head Wobble And Fall Risk

As we age, changes in our walking pattern often lead to increased upper body movement, or ‘head wobble’. Excessive side-to-side head motion while walking not only looks unstable but can indicate impairments that raise fall risk. The underlying cause typically involves reduced torque, or rotational force, generated in the lower limbs. Understanding the relationship between gait torque deficiencies and increased head oscillation provides key insights for improving stability.
Healthy smooth gait relies on optimal coordination between multiple muscle groups to efficiently propel the body forward. The gluteal and quadriceps muscles generate forward torque around the hip and knee joints, controlling acceleration of the leg into swing phase. Weakness in these muscles reduces torque, disrupting the normal walking rhythm.
With low propulsion torques, the center of mass rises and falls with each step instead of following a steady trajectory. The trunk and upper body must work harder to counteract these excessive vertical movements. This often leads to increased rotation of the head and unstable side-to-side wobbling.
Studies show that aging adults who display greater head oscillation during gait tend to have decreased torque around the hip and knee. This link persists even when controlling for walking speed, indicating the specific role of torque deficits. The resulting unsteadiness significantly increases risk of falls and resulting injuries.
Fortunately, targeted exercises to improve torque generation can help reestablish efficient gait patterns and reduce head wobble. Training protocols focus on strengthening the gluteal and quadriceps muscles using resistance bands, free weights, or body weight. Monitoring head acceleration and torque measures provides objective feedback on progress.
Assistive walking devices can also help compensate for muscle weakness. Nordic poles enhance stability during gait by increasing ground force application. Other aids like braces or prosthetics are engineered to optimize torque generation. Maximizing torque reduces destabilizing vertical movements, translating to smoother walking.
In summary, age-related gait instabilities often arise from reduced torque output in the lower limbs. This results in excessive upper body motion, seen as increased head wobble. Corrective interventions aimed at improving propulsion torques can reestablish efficient gait patterns and improve stability. Analyzing torque generation provides insights for targeted rehabilitation to reduce fall risk.
Proper Torque Alignment Prevents Fatigue And Pain
Walking is a complex coordinated activity, but it’s easy to take for granted until something goes wrong. Improper torque patterns during gait can lead to inefficient movement, early fatigue, and joint pain. By understanding optimal torque alignment and making targeted adjustments, you can unlock fluid walking mechanics and prevent unnecessary wear and tear.
Torque refers to the rotational force generated by muscles contracting across a joint. Proper torque activation sequences are crucial for efficient gait. As you shift your weight forward, hip extensor and ankle plantarflexor muscles produce torque to propel and support the body.
Meanwhile, hip flexors and knee extensors on the swinging leg generate torque to accelerate it forward. Well-timed contractions control torque for smooth heel-strike to toe-off transitions. This alignment of torques minimizes wobbling from side to side.
However, muscle weakness or activation issues can disrupt optimal torque patterns. For example, weak hip abductors may provide inadequate stabilization torque on the stance leg. This causes the pelvis to dip to the unsupported side, called a Trendelenburg gait.
Not only does this feel unstable, but it alters joint alignment and increases forces through the hip joint. Over time, this abnormal torque pattern leads to accelerated wear and tear. Strengthening the hip abductors helps realign torque and prevent joint degeneration.
Prolonged walking with suboptimal torque activation tends to cause a feeling of tiredness or fatigue. The muscles have to work overtime to compensate for deficiencies, draining energy reserves. Proper alignment of torques minimizes wasted effort, allowing you to walk farther without getting worn out.
Physical therapy aims to identify and correct the root torque deficiencies contributing to pain or fatigue. Targeted exercises strengthen muscle groups to optimize torque capacity and coordination. Stretching also helps ensure joints can move through the required range of motion.
Gait training on various surfaces retrains proper torque firing patterns. Biofeedback provides objective measures of torque alignment progress. Assistive devices like orthotics optimize torque angles to offload painful joints.
While surgery may still be required for severe joint damage, conservative care focused on torque optimization often reduces pain and avoids invasive procedures. With proper torque mechanics, the forces through the joints stay in healthy ranges.
In summary, the coordinated application of muscle torque is essential for efficient and comfortable gait. Therapeutic interventions to align torques minimize fatigue, pain, and joint wear and tear. Optimizing torque allows you to walk smoothly and pain-free.
Improve Your Gait: How Adjusting Torque Reduces Head Wobble And Fall Risk
As we age, changes in our walking pattern often lead to increased upper body movement, or ‘head wobble’. Excessive side-to-side head motion while walking not only looks unstable but can indicate impairments that raise fall risk. The underlying cause typically involves reduced torque, or rotational force, generated in the lower limbs. Understanding the relationship between gait torque deficiencies and increased head oscillation provides key insights for improving stability.
Healthy smooth gait relies on optimal coordination between multiple muscle groups to efficiently propel the body forward. The gluteal and quadriceps muscles generate forward torque around the hip and knee joints, controlling acceleration of the leg into swing phase. Weakness in these muscles reduces torque, disrupting the normal walking rhythm.
With low propulsion torques, the center of mass rises and falls with each step instead of following a steady trajectory. The trunk and upper body must work harder to counteract these excessive vertical movements. This often leads to increased rotation of the head and unstable side-to-side wobbling.
Studies show that aging adults who display greater head oscillation during gait tend to have decreased torque around the hip and knee. This link persists even when controlling for walking speed, indicating the specific role of torque deficits. The resulting unsteadiness significantly increases risk of falls and resulting injuries.
Fortunately, targeted exercises to improve torque generation can help reestablish efficient gait patterns and reduce head wobble. Training protocols focus on strengthening the gluteal and quadriceps muscles using resistance bands, free weights, or body weight. Monitoring head acceleration and torque measures provides objective feedback on progress.
Assistive walking devices can also help compensate for muscle weakness. Nordic poles enhance stability during gait by increasing ground force application. Other aids like braces or prosthetics are engineered to optimize torque generation. Maximizing torque reduces destabilizing vertical movements, translating to smoother walking.
In summary, age-related gait instabilities often arise from reduced torque output in the lower limbs. This results in excessive upper body motion, seen as increased head wobble. Corrective interventions aimed at improving propulsion torques can reestablish efficient gait patterns and improve stability. Analyzing torque generation provides insights for targeted rehabilitation to reduce fall risk.
Optimizing Torque Improves Overall Gait Efficiency
Walking is something most of us do without thinking, but it requires complex coordination of muscle activity. The contraction of muscles generates torque, or rotational force, across joints to propel the body forward. Optimizing these torque patterns is key for maximizing gait efficiency and avoiding wasted effort.
Healthy walking relies on properly sequenced torque generation through the legs and hips. As you transfer weight to one leg, the hip abductors and ankle everters produce torque to stabilize the pelvis and ankle. Meanwhile, hip flexors and knee extensors generate forward swing torque.
Well-timed muscle activations ensure torque is applied in the right direction at the right time. This aligns the ground reaction forces through the joints, providing smooth acceleration. Optimized torque allows you to walk farther with less fatigue.
However, impairments in strength, flexibility, or motor control can disrupt optimal torque patterns. Weak hip extensors may inadequately accelerate the leg into swing phase. Tight hip flexors can inhibit proper hip extension torque.
Abnormal torque activation squanders metabolic energy. Additional muscle groups have to compensate and work harder to maintain forward progress. This leads to a feeling of inefficiency and tiring out more quickly.
Physical therapy aims to identify and correct suboptimal torque contributors to improve gait economy. Targeted strengthening builds muscle endurance for sustaining proper torque over time. Stretching increases range of motion for better torque generation.
Gait retraining provides cues to activate key muscle groups, facilitating ideal timing of torque application. Assistive devices like braces or canes can help optimize torque angles. Reducing excessive or poorly timed torque minimizes wasted effort.
Wearable sensors enable real-time feedback on torque patterns during walking. This data helps fine-tune muscle engagement to enhance forward propulsion and stability torque. Achieving ideal alignment reduces accessory motions and unnecessary energy expenditure.
Maximizing gait efficiency has many advantages beyond just saving energy. It reduces joint loads and delays fatigue onset in the muscles. This helps prevent overuse injuries. Optimized torque also smooths out gait irregularities that can lead to falls in older adults.
In summary, proper torque coordination is crucial for efficient walking mechanics. Targeted rehabilitation and gait retraining helps optimize torque generation sequences. This aligns joint forces, reduces wasted motion, and maximizes stride propulsion. The result is tiring less quickly and walking comfortably farther.
Improve Your Gait: How Adjusting Torque Reduces Head Wobble And Fall Risk
As we age, changes in our walking pattern often lead to increased upper body movement, or ‘head wobble’. Excessive side-to-side head motion while walking not only looks unstable but can indicate impairments that raise fall risk. The underlying cause typically involves reduced torque, or rotational force, generated in the lower limbs. Understanding the relationship between gait torque deficiencies and increased head oscillation provides key insights for improving stability.
Healthy smooth gait relies on optimal coordination between multiple muscle groups to efficiently propel the body forward. The gluteal and quadriceps muscles generate forward torque around the hip and knee joints, controlling acceleration of the leg into swing phase. Weakness in these muscles reduces torque, disrupting the normal walking rhythm.
With low propulsion torques, the center of mass rises and falls with each step instead of following a steady trajectory. The trunk and upper body must work harder to counteract these excessive vertical movements. This often leads to increased rotation of the head and unstable side-to-side wobbling.
Studies show that aging adults who display greater head oscillation during gait tend to have decreased torque around the hip and knee. This link persists even when controlling for walking speed, indicating the specific role of torque deficits. The resulting unsteadiness significantly increases risk of falls and resulting injuries.
Fortunately, targeted exercises to improve torque generation can help reestablish efficient gait patterns and reduce head wobble. Training protocols focus on strengthening the gluteal and quadriceps muscles using resistance bands, free weights, or body weight. Monitoring head acceleration and torque measures provides objective feedback on progress.
Assistive walking devices can also help compensate for muscle weakness. Nordic poles enhance stability during gait by increasing ground force application. Other aids like braces or prosthetics are engineered to optimize torque generation. Maximizing torque reduces destabilizing vertical movements, translating to smoother walking.
In summary, age-related gait instabilities often arise from reduced torque output in the lower limbs. This results in excessive upper body motion, seen as increased head wobble. Corrective interventions aimed at improving propulsion torques can reestablish efficient gait patterns and improve stability. Analyzing torque generation provides insights for targeted rehabilitation to reduce fall risk.
Simple Exercises To Improve Gait Torque At Home
Having a smooth, efficient gait is important for balance, mobility, and fall risk reduction. Gait torque – the twisting force produced when we walk – is a key element in stride mechanics. High torque levels at the hip, knee and ankle are linked to forceful, stable steps. As we age, gait torque naturally declines, contributing to unsteady walking patterns. The good news is that targeted exercises can improve torque and enhance your overall gait.
Gait torque is created by the contraction of muscles that laterally rotate and abduct the hip, flex the knee, and plantarflex the ankle as we walk. This torque enables powerful propulsion with each step. Insufficient torque leads to reduced stride length, slow velocity, excessive vertical oscillations of the head, and greater vulnerability to falls.
Here are 5 simple at-home exercises to boost gait torque:
1. Side-Stepping with Resistance Band
This exercise strengthens your hip abductors – key muscles for producing torque during gait. Place a looped resistance band around your thighs, just above the knees. Stand with feet hip-width apart. Keeping toes facing forward, step sideways with one leg, then bring the other leg in to meet it. Repeat for 10-15 steps each direction. Perform 2-3 sets.
2. Hip Hiking
This move directly works the hip hiking motion used in gait. Stand sideways near a wall for support. Slowly lift one hip up towards the ceiling, then lower it down. Switch sides. Repeat 10 times on each leg. Do 2 sets. For a greater challenge, perform without the wall support.
3. Seated Knee Extensions
Sit upright in a chair. Lift one leg and fully straighten the knee, tightening the quadriceps. Hold for 5 seconds. Lower back down, keeping foot flexed. Repeat 10 times, then switch legs. Complete 2-3 sets per side. Strong quads are vital for gait knee torque.
4. Calf Raises
Stand with feet hip-width apart. Raise up onto your toes, lifting heels as high as possible. Pause briefly, then lower back down. Repeat for 10-12 reps. For added difficulty, perform single-leg calf raises. Do 2-3 sets. This strengthens the calf muscles responsible for gait ankle torque.
5. Sit-to-Stand
Sit tall near the front of a chair. Lean forward slightly and stand up (with hands on chair if needed). Slowly lower back into the seat. Repeat 10 times. Work up to not using your hands. This builds lower-body power for gait torque generation.
Aim to perform these gait torque exercises 2-3 times per week, along with aerobic activity like walking to improve endurance. Monitor your progress by checking stride length and head sway. As torque improves, your steps should become more powerful and controlled, with less vertical head movement.
Other tips for optimizing torque at home include:
- Wear supportive, well-fitted shoes to enhance force transfer.
- Walk on softer surfaces like grass or dirt to increase muscle activation.
- Have home safety modifications like ramps, railings and good lighting.
- Ask your physical therapist about assistive devices if needed.
Enhancing your gait now pays dividends later by preserving mobility, balance and independence. Simple home exercises that increase hip, knee and ankle torque are an easy way to strengthen key muscles for walking power, stability and fall prevention.
How Physical Therapists Assess And Treat Gait Torque
When we walk, our body exerts forces against the ground to propel us forward. The ground pushes back against these forces to keep us upright. This interaction of opposing forces is called torque. Optimizing torque generation and absorption during gait is key for stability and preventing falls.
Physical therapists are experts at evaluating and correcting dysfunctional gait torque. By assessing joint motions and muscle activity patterns, they can identify impairments in a patient’s ability to produce or attenuate forces. They then design customized treatment programs to restore optimal torque control.
The Role of Torque in Walking
During gait, the lead leg exerts a forward propulsive force against the ground while the trailing leg pushes backward to propel the body. The ground pushes back with equal force to keep us upright. This interaction generates torque around each leg joint.
The hip, knee and ankle all play roles in producing and absorbing torque during walking. For example, the hip extensors like the gluteus maximus produce hip extension torque to propel the leg backward. Meanwhile, the knee extensors like the quadriceps produce knee extension torque to straighten the knee. The ankle plantarflexors like the calf muscles exert torque to propel the body forward.
Torque must be properly coordinated across all leg joints for efficient gait. The muscles work synergistically to optimize torque generation and absorption. This prevents excessive or inadequate joint motions that can lead to instability.
How Physical Therapists Assess Gait Torque
Physical therapists use various methods to evaluate a patient’s gait torque patterns:
- Observing joint motions and alignment during walking to detect abnormalities.
- Analyzing muscle activity on EMG to identify impaired firing patterns.
- Measuring joint kinetics using force plates or special equipment.
- Assessing strength and flexibility to identify torque limitations.
- Reviewing past injuries and surgeries that could impact torque capacity.
This information helps pinpoint where torque production or absorption is dysfunctional. For example, reduced firing of the hip abductors could limit hip extension torque on that side. Or weak ankle plantarflexors may limit propulsive torque.
Treatment Strategies to Improve Gait Torque
Once dysfunctional gait torque patterns are identified, physical therapists implement customized treatments. Some key strategies include:
- Strengthening exercises – Target weakened muscles to increase torque capacity.
- Neuromuscular re-education – Retrain appropriate muscle firing patterns during gait.
- Mobility and flexibility training – Optimize joint range of motion for torque generation.
- Orthotics or braces – Use external support to improve alignment and torque mechanics.
- Balance and perturbation training – Enhance ability to absorb and react to torque during gait.
The goal is to restore efficient coordination of torque production and absorption across the hip, knee and ankle. This improves stability, propulsion, shock absorption and overall gait biomechanics.
Benefits of Optimizing Gait Torque
Correcting gait torque deficits provides many benefits for patients including:
- Reduced wobbling and deviations while walking
- Decreased risk of instability, tripping or falls
- Improved ability to start and stop smoothly
- Increased walking speed and endurance
- Lower risk of joint degeneration from improper mechanics
- Enhanced shock absorption and impact reduction
By evaluating and treating dysfunctional torque patterns, physical therapists can help patients achieve a smoother, steadier and safer gait. This reduces fall risk and improves mobility, independence and quality of life.
Medical Conditions That Disrupt Healthy Gait Torque
Our ability to walk depends on properly generating and controlling torque – the rotational forces produced by our muscles and joints. Certain medical conditions can disrupt normal gait torque patterns, leading to an unstable and unsafe walking pattern.
Physical therapists are experts at assessing how diseases and injuries impact gait torque production. By identifying impaired torque mechanisms, they can implement customized treatment to restore efficient walking ability.
Neurological Conditions
Neurological diseases often affect the nervous system’s ability to coordinate muscle activity and joint motions needed for proper gait torque:
- Stroke – Weakness or paralysis on one side limits torque capacity.
- Parkinson’s disease – Rigidity and tremors lead to poor torque control.
- Multiple sclerosis – Nerve damage causes torque generation problems.
- Spinal cord injury – Interruption of signals to the muscles disrupts torque patterns.
Physical therapy focuses on strengthening weak muscles, improving flexibility, and retraining more normal movement and torque production.
Orthopedic Conditions
Damage to the muscles, bones, and joints involved in walking can alter gait torque mechanics:
- Arthritis – Pain and stiffness affect torque generation capacity.
- Tendonitis – Inflamed tendons reduce torque from calf and foot.
- Knee or hip osteoarthritis – Loss of cartilage leads to painful, limited torque.
- Lower limb fractures – Healing bones impact torque absorption.
Treatment focuses on pain relief, incrementally increasing torque capacity, and optimizing joint alignment with braces or aids.
Other Diseases
Some other conditions causing gait torque problems include:
- Peripheral neuropathy – Nerve damage leads to poor torque control.
- Vestibular disorders – Impaired balance limits ability to react to torque.
- Charcot foot – Causes collapse of arch structure needed for propulsion.
- Diabetes – High blood sugar can affect joint mobility and torque capacity.
Therapy involves gait training, strength work, and techniques to enhance sensory awareness and feedback.
Customized Treatment
While various conditions disrupt gait torque patterns through different mechanisms, physical therapists can thoroughly assess each patient and design specialized programs to correct deficiencies. The goal is to restore efficient torque production and shock absorption so patients can walk safely and independently.
Torque-Modifying Footwear And Assistive Devices
Generating the right amount of torque or rotational force is key for efficient and stable walking. Some people with gait abnormalities benefit from footwear, braces, or mobility aids designed to improve torque production and absorption.
Physical therapists often recommend and fit patients with these torque-modifying devices. By restoring proper torque patterns, they can significantly improve gait, balance, and safety.
Orthotic Shoes and Inserts
Specially designed orthotic footwear and inserts can optimize gait torque patterns in several ways:
- Cushioning absorbs shock and impact torques during foot strike.
- Arch supports improve propulsive torque from the feet and ankles.
- Heel lifts and wedges change alignment and torque angles.
- Motion control shoes prevent excessive joint and torque motions.
These modifications enhance stability, reduce pain, and restore normal torque mechanics at each step.
Ankle-Foot Orthoses
Custom ankle-foot orthoses (AFOs) are external braces that control ankle position and motion during gait. Benefits include:
- Preventing foot drop which disrupts propulsive torque.
- Improving alignment to optimize torque angles.
- Providing leverage for torque generation from calf muscles.
- Immobilizing joint to eliminate unhealthy torque forces.
AFOs enhance stability, reduce strain, and normalize torque patterns.
Knee Braces
Specialized knee braces can also improve gait torque issues by:
- Supporting and aligning the joint for proper torque absorption.
- Reducing painful motions that impair smooth torque generation.
- Providing leverage for quadriceps and hamstrings to produce torque.
- Immobilizing partially to eliminate unhealthy torque forces.
Knee braces tailor torque mechanics to enhance stability and function.
Canes, Crutches, and Walkers
Assistive devices like canes, crutches, and walkers redistribute body weight to optimize gait torque patterns:
- Improve balance to allow stronger torque generation.
- Absorb impact torques through the arms rather than lower joints.
- Enhance base of support for more controlled torque absorption.
- Reduce load on painful joints to enable smoother torque production.
The devices provide leverage, support, and stability to normalize gait torque mechanics.
With their expertise in biomechanics, physical therapists can match patients to the ideal torque-modifying devices for safer walking and daily function.
The Importance Of Gait Analysis And Torque Measurement
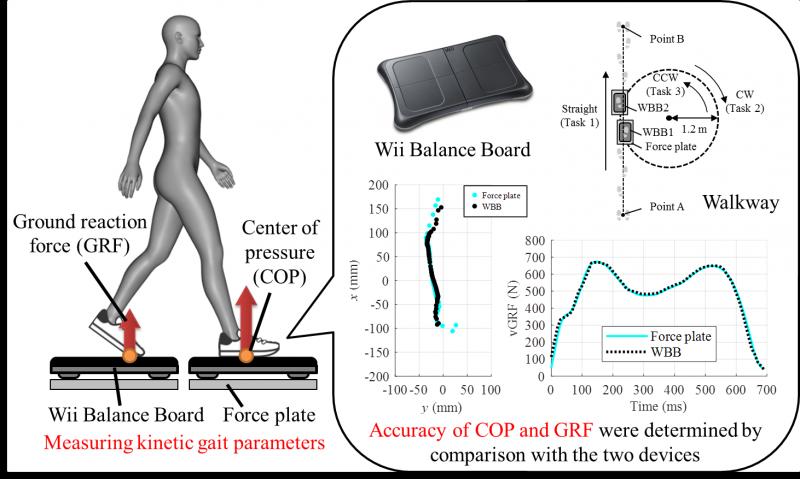
Understanding normal and abnormal gait patterns is key for physical therapists treating mobility impairments. Advanced gait analysis using force plates, motion capture and EMG provides objective data on joint motions, muscle activity, and ground reaction forces during walking.
One vital parameter quantified during gait analysis is torque – the rotational forces exerted by muscles across joints. Measuring torque production and absorption provides invaluable insight into gait abnormalities.
Measuring Gait Kinetics
Kinetic analysis using embedded force plates as patients walk examines ground reaction forces and the torques they generate on the body. Key parameters include:
- Joint torque – rotations caused by muscle contractions and ground forces.
- Joint power – the rate at which muscles do work by producing torque.
- Center of pressure – distribution of torque on the foot soles.
This data precisely quantifies torque patterns at the hip, knee and ankle during gait phases like heel strike, push off, and swing through.
Identifying Torque Abnormalities
Analyzing joint torque metrics enables physical therapists to pinpoint specific gait deficits like:
- Reduced hip extension torque due to weak glutes.
- Excessive knee torque from quadriceps imbalance.
- Inadequate push off torque from weakened calf muscles.
- High impact torque at heel strike indicating poor shock absorption.
Torque data reveals dysfunctional muscle activity required to walk efficiently.
Guiding Treatment Plans
Quantifying gait torque deficits helps physical therapists design targeted treatment programs including:
- Strengthening specific muscles to increase torque capacity.
- Retraining walking patterns to normalize torque coordination.
- Orthoses to improve alignment and torque angles.
- Reducing torque loads on unstable joints.
Follow-up gait analysis verifies if torque abnormalities are corrected and gait is improved after interventions.
Optimizing Mobility and Stability
Analyzing and correcting dysfunctional torque patterns is crucial for enhancing gait efficiency, balance, propulsion, shock absorption and stability. The detailed insights from gait torque measurement guide physical therapists in treating mobility impairments for safer walking.
Adjusting Torque Helps Prevent Falls In The Elderly
As we age, gait and balance impairments increase the risk of debilitating falls. A major factor is reduced ability to effectively produce and control rotational forces or torque during walking. With training, elderly adults can optimize gait torque patterns and prevent dangerous stumbles.
Physical therapists are experts in gait analysis and fall risk assessments. By identifying torque deficiencies, they implement customized programs to enhance stability in seniors.
Why The Elderly Fall
Age-related physical declines negatively impact gait stability:
- Weakened muscles reduce torque generation capacity.
- Stiff joints limit ability to absorb forces and torque.
- Declining vision disrupts torque control and reactions.
- Medications can cause dizziness and alter torque patterns.
Without adequate torque from muscles, elderly adults cannot recover balance when tripped or bumped. This leads to devastating fall injuries.
Assessing Gait and Torque
Physical therapists conduct thorough evaluations including:
- Observing walking pattern to detect instability.
- Testing joint flexibility needed for torque motions.
- Measuring muscle strength for generating torque.
- Quantifying torque production and absorption with gait analysis.
This identifies specific torque limitations impacting balance and mobility.
Customized Treatment Programs
Physical therapists design interventions to enhance elderly gait torque:
- Targeted strengthening exercises increase torque capacity.
- Perturbation and balance training hone reactive torque skills.
- Assistive devices improve torque generation leverage.
- Orthotics optimize torque angles at joints.
Multifactorial programs aim to improve torque production, absorption, and control during walking.
Preventing Falls with Proper Torque
Optimizing gait torque patterns provides elderly adults with:
- Improved balance and stability.
- Enhanced ability to respond to trips or slips.
- Smoother, steadier walking pattern.
- Increased confidence in mobility and independence.
Physical therapy can help seniors safely remain active and reduce fall risk by addressing age-related torque deficiencies.
Targeted Stretching To Improve Gait Torque Imbalances
Generating proper rotational force or torque across joints is key for efficient walking. Limited flexibility in specific muscle groups can throw off optimal gait torque patterns. Targeted stretching is an effective way to address torque imbalances.
Physical therapists are experts in identifying restrictions that disrupt normal torque mechanics during gait. They design customized stretching programs to improve range of motion and walking stability.
How Stiffness Alters Torque
Limited flexibility in areas like the calves, hamstrings, hips and lower back can negatively impact gait torque:
- Short calf muscles reduce push off torque from the ankle.
- Tight hamstrings limit torque generation at the knee.
- Stiff hips restrict powerful glute torque needed for propulsion.
- Low back tightness prevents proper trunk rotation and torque absorption.
These restrictions throw off coordinated torque patterns, reduce shock absorption, and disrupt stability.
Targeting Specific Muscle Groups
Physical therapists identify problem areas through range of motion assessments and gait analysis. Targeted stretches improve flexibility:
- Calf stretches – Increase ankle mobility for propulsive torque.
- Hamstring stretches – Enable greater knee torque during swing through.
- Hip flexor and glute stretches – Allow more hip extension torque.
- Low back stretches – Improve trunk rotation for torque absorption.
Programs are tailored to individual needs and gait deficits.
Restoring Optimal Torque Patterns
Dedicated stretching to increase range and reduce imbalances provides several gait benefits:
- Allows muscles to generate torque through full range of motion.
- Improves shock absorption as joints have greater flexion for torque attenuation.
- Reduces compensations and substitution patterns that disrupt torque coordination.
- Normalizes torque angles and directions at each joint.
Targeted stretching can restore optimal gait torque patterns for enhanced stability, speed, endurance and balance.
Flexible Muscles Produce Better Torque
Physical therapists leverage stretching techniques to improve flexibility issues that alter gait torque mechanics. Opening tight areas allows muscles to generate and control torque during walking for efficient stability.
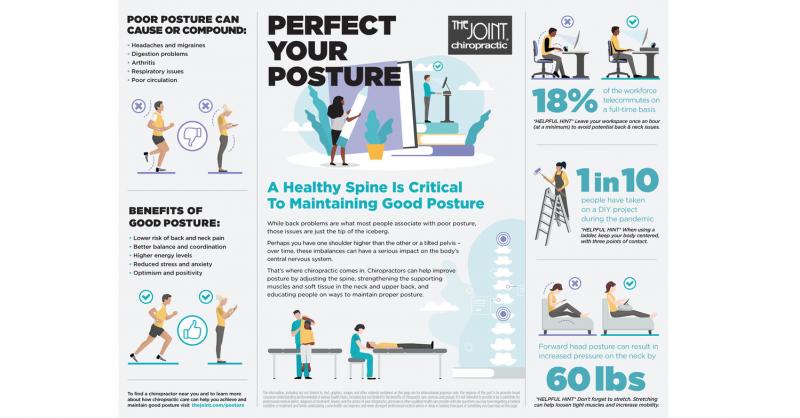
Lifestyle And Postural Changes For Better Gait Torque
Generating adequate rotational force or torque when walking depends on proper alignment and coordinated muscle patterns. Lifestyle factors like posture, activity levels, and footwear choices can enhance or disrupt gait torque.
Physical therapists identify lifestyle issues negatively impacting torque. They provide personalized recommendations to improve walking biomechanics.
How Lifestyle Impacts Torque
Certain lifestyle factors influence gait torque production and absorption:
- Poor posture misaligns joints and alters optimal torque angles.
- Lack of activity weakens muscles needed to generate torque.
- Excess weight increases torque demands on the joints.
- Improper footwear reduces stability for controlling torque.
By optimizing these areas, people can improve gait torque patterns.
Postural Modifications
Physical therapists identify postural issues negatively impacting gait torque like:
- Rounded shoulders limiting arm swing and torso rotation torque.
- Forward head position disrupting visual feedback for torque reactions.
- Excessive arch or flat feet altering optimal propulsive torque angles.
Postural retraining, cueing, and bracing can reinforce better alignment for gait torque generation.
Increasing Physical Activity
Lack of exercise leads to weak muscles unable to produce adequate torque. Physical therapists recommend targeted strength training to enhance gait torque capacity and control.
Proper Footwear
Supportive shoes with cushioning, stability features, and orthotics can optimize torque absorption and propulsion. Ill-fitting footwear contributes to torque problems.
Improving Torque Through Lifestyle Factors
By correcting poor posture, increasing activity, and wearing appropriate footwear, people can facilitate correct gait torque patterns. This provides better stability, mobility and reduced injury risk.
Achieving Optimal Gait Through Torque Balance And Control
Walking efficiently depends on muscles properly generating and absorbing rotational forces or torque across joints. With training, people can optimize torque patterns for smooth, stable gait.
Physical therapists are experts in gait analysis and torque deficiencies. They design comprehensive programs focused on restoring torque balance and control.
Characteristics of Ideal Torque
Normal gait requires coordinated torque production and attenuation across the hips, knees and ankles. Key elements include:
- Adequate torque generation from major muscle groups.
- Smooth acceleration and deceleration of joint torque motions.
- Symmetric torque patterns between left and right legs.
- Proper shock absorption as joints flex to absorb torque.
- Ideal torque directions and angles at each joint.
This optimizes walking efficiency, speed, stability and impact reduction.
Identifying Torque Dysfunction
Physical therapists use gait analysis and assessments to pinpoint problematic torque patterns like:
- Low push off torque from weak ankle muscles.
- Excessive torque from overly tight hip flexors.
- Asymmetric knee torque due to joint injury.
- Poor shock absorption and impact torque at heel strike.
Accurately identifying torque deficiencies and imbalances is key.
Restoring Ideal Torque Control
Treatments target identified issues to improve torque balance and coordination:
- Strengthen weak muscles to increase torque capacity.
- Stretch tight musculature to optimize torque angles.
- Retrain coordinated motion patterns during gait.
- Use bracing and orthotics to improve torque alignment.
This comprehensive approach achieves smoother, safer walking by optimizing all aspects of gait torque generation and control.

