What are the goals of Ongoing Professional Practice Evaluation. How is OPPE designed and implemented in healthcare organizations. What types of data are used in OPPE processes. How frequently should OPPE reviews be conducted. How is OPPE data used in decision-making processes.
Understanding Ongoing Professional Practice Evaluation (OPPE)
Ongoing Professional Practice Evaluation (OPPE) is a crucial component of medical staff peer review processes in healthcare organizations. This data-driven approach aims to continuously assess and improve the performance of healthcare practitioners. Let’s delve into the key aspects of OPPE and its implementation.
Goals of OPPE
The primary objectives of OPPE include:
- Identifying performance trends through qualitative and quantitative data analysis
- Implementing steps to improve performance when necessary, such as focused professional practice evaluations (FPPE)
- Establishing an objective foundation for re-privileging decisions
Designing an Effective OPPE Process
A well-designed OPPE process should include clearly defined elements such as:
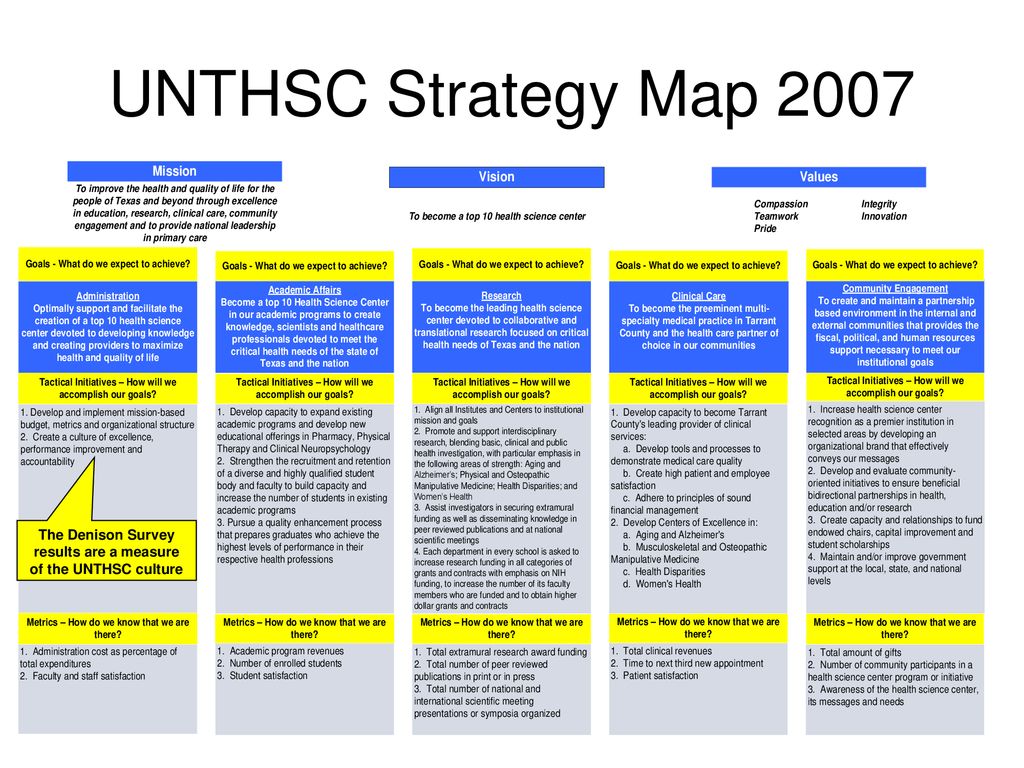
- Responsibilities for data review, which may involve:
- Department chairs or entire departments
- Credentialing committees
- Medical Executive Committees
- Special committees of the organized medical staff
- Frequency of review
- Process for using data in decision-making
- Decision-making procedures resulting from the review (e.g., continue, limit, or deny privileges)
Data Collection and Review Frequency in OPPE
The organized medical staff is responsible for defining the frequency of data collection for OPPE. This process may involve various types of data, including both qualitative and quantitative information.
Qualitative Data in OPPE
Qualitative data for OPPE may include:
- Description of procedures performed
- Periodic chart reviews, focusing on:
- Quality and accuracy of documentation
- Appropriateness of tests ordered and procedures performed
- Patient outcomes
- Types of patient complaints
- Code of conduct breaches
- Peer recommendations
- Discussions with other individuals involved in patient care
When reviewing qualitative data related to performance quality, it’s essential that someone with equivalent qualifications conducts the evaluation.

Quantitative Data in OPPE
Quantitative data often reflects specific quantities, amounts, or ranges, typically expressed as units of measure. It’s important to note that the manner of data capture can sometimes represent both qualitative and quantitative information.
Data Sources for OPPE
The data used in the OPPE process must include practitioner activities performed at the organization where privileges have been requested. This may encompass activities at any location under the organization’s single CMS Certification Number (CCN).
Multi-hospital Systems and OPPE
In multi-hospital systems where each hospital operates independently under separate CCNs, data from these entities may be used to supplement local data. However, it’s crucial to ensure that local data is still captured and evaluated.
Addressing Low-volume Practitioners
For practitioners with low or limited activity at the local level, supplemental data from another CMS-certified organization where the practitioner holds the same privileges may be used. However, this supplemental data should not replace the process of capturing local data.
Examples of situations where supplemental data might be appropriate include:
- Practitioners providing periodic on-call coverage for other physicians or groups
- Occasional consultations for a clinical specialty
Organizations using supplemental data should assess its relevance, timeliness, and accuracy.
Implementing OPPE in Non-inpatient Areas
OPPE applies to any privileges granted within the scope of the hospital survey, including inpatient, on-campus outpatient, off-campus clinics, and hospital-owned physician office practices. Privileges need to be granted to anyone providing a medical level of care, such as making medical diagnoses or treatment decisions.
Challenges in Non-inpatient OPPE
While the privileges for non-inpatient settings are often the same as those for inpatient care, collecting data may be more challenging if these settings do not have the same clinical record system or information technology. However, if the privileges are the same, the data collected should be consistent across all settings.

Utilizing OPPE Data in Decision-making Processes
The information gathered through OPPE needs to be used effectively in decision-making processes. This involves determining whether to continue, limit, or revoke existing privileges at the time the information is analyzed.
Potential Outcomes of OPPE Data Analysis
Based on the analysis of OPPE data, several possible actions may occur:
- Determining that the practitioner is performing well or within desired expectations, requiring no further action
- Identifying a performance issue that requires a focused evaluation (as per MS.08.01.01 EP 5)
- Revoking a privilege because it is no longer necessary or appropriate
Ensuring Compliance with OPPE Requirements
To ensure compliance with OPPE requirements, healthcare organizations should focus on several key areas:
Developing Clear Policies and Procedures
Organizations must develop comprehensive policies and procedures that outline:
- The process for data collection and review
- Responsibilities of various stakeholders in the OPPE process
- Guidelines for using supplemental data when necessary
- Procedures for addressing performance issues identified through OPPE
Training and Education
Providing adequate training and education to medical staff members and leadership is crucial for effective OPPE implementation. This may include:

- Workshops on OPPE best practices
- Training sessions on data analysis and interpretation
- Regular updates on changes to OPPE requirements and processes
Regular Audits and Quality Improvement
Conducting regular audits of the OPPE process can help identify areas for improvement and ensure ongoing compliance. This may involve:
- Reviewing the timeliness and completeness of OPPE data collection
- Assessing the effectiveness of decision-making processes based on OPPE data
- Identifying and addressing any gaps in the OPPE process
Addressing Challenges in OPPE Implementation
While OPPE is a valuable tool for ensuring quality patient care, its implementation can present several challenges. Let’s explore some common issues and potential solutions:
Data Collection and Management
One of the primary challenges in OPPE is collecting and managing large amounts of data from various sources. To address this:
- Implement robust electronic health record (EHR) systems that can easily capture and report relevant data
- Develop standardized data collection templates to ensure consistency across different departments and specialties
- Invest in data analytics tools to help process and interpret large datasets efficiently
Resistance from Medical Staff
Some practitioners may be resistant to the OPPE process, viewing it as an additional administrative burden. To overcome this:

- Communicate the benefits of OPPE for patient safety and quality improvement
- Involve medical staff in the development and refinement of OPPE processes
- Provide regular feedback and demonstrate how OPPE data is used to support professional development
Ensuring Fairness and Objectivity
Maintaining fairness and objectivity in the OPPE process is crucial. To achieve this:
- Develop clear, objective criteria for evaluating performance
- Use multiple data sources to provide a comprehensive view of practitioner performance
- Implement peer review processes that involve multiple reviewers to minimize bias
Future Trends in Medical Staff Peer Review and OPPE
As healthcare continues to evolve, so too will the processes for medical staff peer review and OPPE. Some potential future trends include:
Integration of Artificial Intelligence
AI and machine learning technologies may play an increasingly important role in OPPE processes, potentially:
- Analyzing large datasets to identify performance trends more quickly and accurately
- Predicting potential performance issues before they become significant problems
- Automating certain aspects of the data collection and analysis process
Focus on Patient-Reported Outcomes
There may be an increased emphasis on incorporating patient-reported outcomes and experiences into OPPE processes. This could involve:

- Developing more sophisticated patient feedback systems
- Incorporating patient-reported outcome measures (PROMs) into OPPE data collection
- Giving greater weight to patient satisfaction and experience metrics in performance evaluations
Expansion of Telemedicine Considerations
As telemedicine becomes more prevalent, OPPE processes may need to adapt to evaluate performance in virtual care settings. This might include:
- Developing specific criteria for assessing telemedicine consultations
- Implementing new tools for monitoring and evaluating virtual patient interactions
- Addressing unique challenges related to privacy and security in telemedicine practice
By staying abreast of these trends and continuously refining their OPPE processes, healthcare organizations can ensure they are well-positioned to maintain high standards of patient care and safety in an ever-changing healthcare landscape.
The Role of OPPE in Continuous Quality Improvement
OPPE plays a crucial role in the broader context of continuous quality improvement in healthcare organizations. Let’s explore how OPPE contributes to ongoing efforts to enhance patient care and safety:
Identifying Areas for Improvement
OPPE processes can help healthcare organizations pinpoint specific areas where individual practitioners or entire departments may need to improve. This might involve:
- Analyzing trends in patient outcomes across different specialties
- Identifying patterns in medication errors or adverse events
- Assessing compliance with best practice guidelines and protocols
Facilitating Targeted Interventions
Once areas for improvement are identified through OPPE, organizations can implement targeted interventions to address these issues. This may include:
- Providing additional training or education for specific practitioners or teams
- Revising protocols or procedures to address identified gaps
- Implementing new technologies or tools to support improved performance
Promoting a Culture of Excellence
By consistently monitoring and evaluating practitioner performance, OPPE helps to foster a culture of excellence within healthcare organizations. This can lead to:
- Increased awareness of quality and safety issues among medical staff
- Greater accountability for individual and team performance
- Ongoing dialogue about best practices and opportunities for improvement
In conclusion, Ongoing Professional Practice Evaluation (OPPE) is a vital component of medical staff peer review processes, contributing to improved patient care, safety, and overall healthcare quality. By implementing robust OPPE systems, addressing challenges, and staying attuned to future trends, healthcare organizations can ensure they are well-equipped to meet the evolving demands of the healthcare landscape while maintaining the highest standards of professional practice.
Ongoing Professional Practice Evaluation (OPPE) – Understanding the Requirements | Critical Access Hospital | Medical Staff MS
Goals
The goals include:
- A qualitative and quantitative data-driven process to identify performance trends that may require taking steps to improve performance (e.g. implementing an FPPE review).
- Establishing an objective, data-driven foundation for making re-privileging decisions.
Design
clearly-defined process that includes elements, such as:
- Responsibilities for data review, as defined by the medical staff that may include:
- Department chair or the department as a whole
- Credentialing committee
- Medical Executive Committee
- Special committee of the organized medical staff
- Frequency of review
- The process for using data for decision-making
- The decision process resulting from the review (continue/limit/deny privilege)
Frequency of Review
The organized medical staff defines the frequency for data collection. ) may include, but are not limited to:
) may include, but are not limited to:
• Description of procedures performed
• Periodic Chart Review
o quality/accuracy of documentation
o appropriateness of tests ordered / procedures performed
o patient outcomes
• Types of patient complaints
• Code of conduct breaches
• Peer recommendations
• Discussion with other individuals involved in the care of patient(s), e.g. consultants, surgical assistants, nursing, administration, etc.
When the data being collected is related to the quality of performance, e.g., appropriate management of a patient’s presenting condition, or the quality of the performance of a procedure, then the organized medical staff should determine that someone with essentially equal qualifications would review the data.
Quantitative Data
Quantitative data often reflects a certain quantity, amount or range and are generally expressed as a unit of measure. Note: The manner in which such data is captured could represent either – or both – qualitative and quantitative information.
Note: The manner in which such data is captured could represent either – or both – qualitative and quantitative information.
Data Sources
The data source used for the OPPE process must include practitioner activities performed at the organization where privileges have been requested. This may include activities performed at any location that falls under the organization’s single CMS Certification Number (CCN). For example, if an organization operates two hospitals that fall under the same CCN number, data from both hospital locations may be used.
Multi-hospital Systems
In multi-hospital systems where each hospital operates independently under separate CMS Certification Numbers (CCN), data from those entities may be used to supplement local data.
Low-volume Practitioners
When practitioner activity at the ‘local’ level is low or limited, supplemental data may be used from another CMS-certified organization where the practitioner holds the same privileges. The use of supplemental data may NOT be used in lieu of a process to capture local data. Organizations choosing to use supplemental data should assess and determine the supplemental data’s relevance, timeliness, and accuracy.
The use of supplemental data may NOT be used in lieu of a process to capture local data. Organizations choosing to use supplemental data should assess and determine the supplemental data’s relevance, timeliness, and accuracy.
Examples where supplemental data could be used may include, but are not limited to:
- activity is limited to periodic on-call coverage for other physicians or groups
- occasional consultations for a clinical specialty
Consistent with the “Medical Staff” chapter, the medical staff must develop policies and procedures which ensure oversight of local data and the use of supplemental data.
OPPE for non-inpatient areas
- Privileges need to be granted to anyone providing a medical level of care, i.e., making medical diagnoses or medical treatment decisions, in any setting that is included within the scope of the hospital survey. The settings can include inpatient, on-campus outpatient, off campus clinics, hospital owned physician office practices, etc.

- OPPE applies to any privileges granted to be exercised in any setting and/or location included within the scope of the hospital survey. The privileges are often the same as those for inpatient care, treatment, and services, therefore, separate privileges based on ‘location’ would not be required. If the non-inpatient settings do not have the same clinical record system or information technology, collecting data may be more difficult, but if the privileges are the same, the data collected should be the same.
Using the Data in Decision-making
The information resulting from the evaluation needs to be used to determine whether to continue, limit, or revoke any existing privilege(s) at the time the information is analyzed. Based on the analysis, several possible actions could occur, for example:
- determining that the practitioner is performing well or within desired expectations and that no further action is warranted
- determining that a performance issues exists and requires a focused evaluation – see MS.
 08.01.01 EP 5.
08.01.01 EP 5. - revoking the privilege because it is no longer required
- suspending the privilege, which suspends the data collection, and notifying the practitioner that if they wish to reactivate it, they must request a reactivation
Evidence of these determinations would need to be available at the time data is reviewed.
“,
“upvotecount”: 1,
“url”: “https://www.jointcommission.org/standards/standard-faqs/critical-access-hospital/medical-staff-ms/000001500/”,
“dateCreated”: “2022-02-4”,
“author”: {
“@type”: “Organization”,
“name”: “The Joint Commission Standards Interpretation Group”
}
}
}
}
Medical Staff Credentialing | Texas Children’s Hospital
Thank you for your interest in joining Texas Children’s Hospital and our mission of creating a healthier future for children and women. We are committed to ensuring quality patient care by applying verification practices in accordance to Texas Children’s Bylaws, Rules and Regulations, Joint Commission (JC) and National Committee for Quality Assurance (NCQA) during our Medical Staff appointment/reappointment process.
We are committed to ensuring quality patient care by applying verification practices in accordance to Texas Children’s Bylaws, Rules and Regulations, Joint Commission (JC) and National Committee for Quality Assurance (NCQA) during our Medical Staff appointment/reappointment process.
JP McGovern Bldg
2450 Holcombe Blvd, Ste. 34L
Houston, TX 77021
Phone: 832-824-2296
Fax: 832-825-0305
[email protected]
Texas Children’s Medical Staff is comprised of the following:
Physicians
Medical Staff – all physicians, dentists, psychologists and podiatrists who are privileged to admit and/or attend patients at the Hospital. Members of the Medical Staff with adjunct privileges are considered members of the Medical Staff; however, they do not have the rights afforded to other members of the Medical Staff set forth in Article IX and X of the Bylaws.
- Medical Doctors
- Doctor of Osteopathy
- Doctor of Dental Surgery
- Doctor of Dental Medicine
Advanced Practice Providers (APPs)
Advanced Practice Provider – practitioner affiliated with the Medical Staff for purposes of providing clinical services, consulting, teaching or other functions deemed necessary by the Medical Staff. Advanced Practice Providers must be sponsored by a member of the Medical Staff. Advanced Practice Providers may include individuals who practice independently within the scope of their licensure and are authorized to perform clinical service in a field allied to medicine but who do not hold a license to practice medicine, dentistry, psychology or podiatry. Advanced Practice Providers are governed by the Medical Staff Non-Physician Practitioner Credentialing Policy and Procedure.
Advanced Practice Providers must be sponsored by a member of the Medical Staff. Advanced Practice Providers may include individuals who practice independently within the scope of their licensure and are authorized to perform clinical service in a field allied to medicine but who do not hold a license to practice medicine, dentistry, psychology or podiatry. Advanced Practice Providers are governed by the Medical Staff Non-Physician Practitioner Credentialing Policy and Procedure.
- Acute Care Nurse Practitioner (ACNP)
- Advanced Practice Registered Nurse (APRN)
- Certified Family Nurse Practitioner (CFNP)
- Certified Registered Nurse Anesthetist (CRNA)
- Certified Neonatal Nurse Practitioner (CNNP)
- Certified Nurse Midwife (CNM)
- Family Nurse Practitioner (FNP)
- Licensed Professional Counselor (LPC)
- Physician Assistant Certified (PA-C)
Allied Health Professionals (AHP)
Allied Health Professional – (i) a dependent practitioner not employed by the Hospital, or (ii) a physician assistant employed by the Hospital, each of whom has been credentialed and approved to assist a member of the Medical Staff with the care and treatment of his/her patients. The AHP shall be under the supervision of a member of the Medical Staff who shall serve as the AHP’s sponsor and retain full responsibility for his/her acts. Dependent AHPs who are employed by the Hospital shall provide services in accordance with the policies of the Hospital, including the Human Resources Department.
The AHP shall be under the supervision of a member of the Medical Staff who shall serve as the AHP’s sponsor and retain full responsibility for his/her acts. Dependent AHPs who are employed by the Hospital shall provide services in accordance with the policies of the Hospital, including the Human Resources Department.
- Licensed Surgical Assistant (LSA)
- Registered Dental Assistant (RDA)
Application Process
To begin the credentialing process, please email your request for an application to [email protected] or call the Credentialing office at (832) 824-2296.
Please include the following information with your request:
- First Name
- Middle Name (if applicable)
- Last Name
- Credentials/License
- Date of Birth
- Specialty Privilege Requesting
- Personal Email Address
- Credentialing Contact’s Name, Phone Number, & Email address (must be different from practitioner)
Texas Children’s Credentialing Fees
Texas Children’s Hospital has an open medical staff except for certain services who have approved exclusivities. No individual is entitled to appointment to the Medical Staff and must be reviewed and approved in accordance to the Bylaws and Credentialing policy of Texas Children’s Hospital. Payment of Texas Children’s Credentialing Fees entitles you to access the general benefits offered to the medical staff, including health and well-being services.
No individual is entitled to appointment to the Medical Staff and must be reviewed and approved in accordance to the Bylaws and Credentialing policy of Texas Children’s Hospital. Payment of Texas Children’s Credentialing Fees entitles you to access the general benefits offered to the medical staff, including health and well-being services.
Review the Texas Children’s Credentialing Fee Schedule to identify the fee for your requested facility(ies).
Verifications
Hospital Privilege Verification
Verification Portal
This website represents current practitioner status information and is maintained by the Texas Children’s Hospital Medical Staff Office. All information contained in the database is secure and cannot be altered by outside parties.
When requesting information, you will be asked to enter your name and contact information as well as the Last Name and Birth Date of the provider. A list of providers matching the inserted criteria, including the provider’s specialty, will then be displayed. If there is more than one provider who matches these criteria, simply select the provider who has the matching specialty you are looking for.
If there is more than one provider who matches these criteria, simply select the provider who has the matching specialty you are looking for.
In response to this request for providers in ‘good standing’, a file quality letter will be displayed with the Name, Appointment Date, Reappointment Date, Department, Specialty, and Staff Status.
Residency/Fellowship Verification
Requests to verify a GME resident’s or fellow’s training at Texas Children’s Hospital are processed by the Medical Staff Services Office. Please contact the office directly with your verification inquiries to [email protected].
Open curatorial hour “Prevention of occupational infection of medical personnel”
course of this specialty, on the topic: “Prevention of occupational infection of medical personnel”, timed to coincide with the Day of the Medical Worker in Russia.
For the curatorial hour, a methodological development for the teacher was prepared. The lesson was accompanied by multimedia presentations, watching videos, which contributed to maintaining the attention and maintaining the interest of students during the entire class hour. In the process of preparing and holding the event, the general competencies were updated:
In the process of preparing and holding the event, the general competencies were updated:
OK 1. Understand the essence and social significance of your future profession, show a steady interest in it.
OK 4. Search and use the information necessary
for the effective performance of professional tasks, professional and personal development.
OK 5. Use information and communication technologies to improve professional activities.
OK 6. Work in a team and team, interact with management, colleagues and social partners.
OK 8. Independently determine the tasks of professional and personal development, engage in self-education, consciously plan advanced training.
curatorial hour contributed to the achievement of personal results:
HR1 Aware of himself as a citizen and defender of a great country;
HR 6 Focused on professional achievements, actively expressing cognitive interests, taking into account one’s abilities, educational and professional route, chosen qualification;
HR 7 Aware of the priority value of a person’s personality; respecting one’s own and others’ uniqueness in various situations, in all forms and activities.
This curatorial hour pursued the following goals and objectives:
- to motivate students to master general and professional competencies as a prerequisite for successful independent professional activity;
- to focus the attention of students on universal, moral and ethical values;
- to remind students of the main stages of prevention and diagnosis of infections transmitted by parenteral and sexual routes, to emphasize the importance of the profession of a laboratory technician, to promote respect and pride in the chosen specialty.
The presented material aroused great interest and emotional response among the students. The students were especially interested in showing a video about the real life of an HIV-infected patient who, thanks to all the recommendations for the treatment and prevention of infection, lives a normal life and was able to give birth to healthy children.
Summing up, the curator of the group Bozhko Yu. M. noted that a medical worker must comply with safety measures to prevent infection with parenteral infections, not only in their professional, but also in everyday life. Compassion, responsiveness, help – these are the main principles on which the activities of medical personnel are based. And only truly strong in spirit, patient, kind, sensitive, sympathetic remain in this profession.
M. noted that a medical worker must comply with safety measures to prevent infection with parenteral infections, not only in their professional, but also in everyday life. Compassion, responsiveness, help – these are the main principles on which the activities of medical personnel are based. And only truly strong in spirit, patient, kind, sensitive, sympathetic remain in this profession.
Students were actively involved in the preparation and holding of the event. All goals of the curatorial hour were achieved. At an open lesson, teachers of the college Medvedeva T.A., Isahakyan E.M., students of the specialty 31.02.03 Laboratory diagnostics and 33.02.01 Pharmacy.
Holding such open events allows developing general competencies and contributes to the achievement of the necessary personal results of future medical workers.
In the process of subsequent discussion, the experience of holding a curatorial hour was recognized as positive and worthy of dissemination among the teaching staff. 9Artemenko N.A.
9Artemenko N.A.
Russian schoolchildren were told about the medicine of the future /TASS/. Leading experts in the field of medicine and Internet technologies told schoolchildren about what medical specialties and technologies will be in demand in the near future at the fourth All-Russian open lesson of the Ministry of Education and Science of the Russian Federation and the Projectoria portal, which was held in Moscow on Thursday, the correspondent reports. TASS.
The organizers dedicated the lesson to the topic of cooperation between doctors and engineers for the development of medicine.
The cycle of All-Russian open lessons “Projection” started on February 8th. They were devoted to agriculture (“What do you know about food?”), urbanism, architecture and construction (“The house you want to live in”) and modern technologies (“Unreal reality”). Thanks to the online broadcast on the Projectoria portal and in the project groups on the social networks VKontakte and Odnoklassniki, schoolchildren, teachers and parents across the country can follow the studio where the lesson takes place. Previous lessons have already gained 10 million views and united 26.6 thousand schools.
Previous lessons have already gained 10 million views and united 26.6 thousand schools.
“In the near future, the professions of pathomorphologists and radiologists will be in demand and promising – instead of 1.8 thousand, there are about 1 thousand doctors, medical physicists – today in our country there are only 380 of them, with the required 1.1 thousand. There are not enough medical geneticists There are not enough radiologist operators, they are paramedical personnel, a very interesting specialty, there are still 300 of them, but 3,000 are needed. We are waiting for a new, young, smart and qualified replenishment, “the invited expert of the meeting, the general director of the Federal State Budgetary Institution, told TASS before the lesson “National Medical Research Center for Radiology” of the Ministry of Health of Russia, head of the Herzen Moscow Cancer Research Institute (MNIOI) Andrey Kaprin.
According to him, medical technology is developing at an extremely fast pace, so there will always be work for specialists in this field. “The problem of an overabundance of personnel will not threaten us for a long time. Qualified specialists will always be worth their weight in gold,” Kaprin is sure.
“The problem of an overabundance of personnel will not threaten us for a long time. Qualified specialists will always be worth their weight in gold,” Kaprin is sure.
The meeting was also attended by Rector of the National Research Nuclear University MEPhI (NRNU MEPhI) Mikhail Strikhanov, First Vice-Rector of Sechenov University Andrey Svistunov, and Advisor to the President of the Russian Federation on Internet Development German Klimenko.
Confidence in the future
The open lesson gave students the opportunity to make sure that they have chosen the right path in order to master the profession of their dreams in the future. “I really like biology, and I graduated from the 9th grade of the physical school. I wanted to become a bioengineer or a surgeon. It was very important for me to get confirmation that I was on the right path, I was achieving what would be useful to me later in life, would be necessary for my career,” Natalia Kraeva, a 10th grade student, told TASS after an open lesson.
“The lesson was very interesting, understandable and informative for me, since I choose the profile of chemistry-bio at the intersection of engineering and chemistry. I want to enter MISiS, because there are large serious laboratories where you can get a lot of practical knowledge, to use them in the future,” 8th grade student Daniil Zabarin shared his impressions with TASS.
Participation of parents
“It is very important that parents watch the lesson, because it is also important for parents to understand what fate awaits the child, the right choice of profession is important. Our children have the opportunity to touch new specialties that exist in every industry,” – said in a conversation with reporters the Minister of Education and Science of the Russian Federation Olga Vasilyeva, who became a special guest of the open lesson.
According to the minister, the cycle of open lessons will be continued, because during the four meetings the organizers managed to cover only a small part of the professions of the future.

 08.01.01 EP 5.
08.01.01 EP 5.