How long should an athlete rest after a concussion. What are the laws governing concussion management in youth sports. When is it safe for an athlete to return to play after experiencing a concussion. How do multiple concussions affect an athlete’s ability to return to sports.
Understanding Concussions in Sports
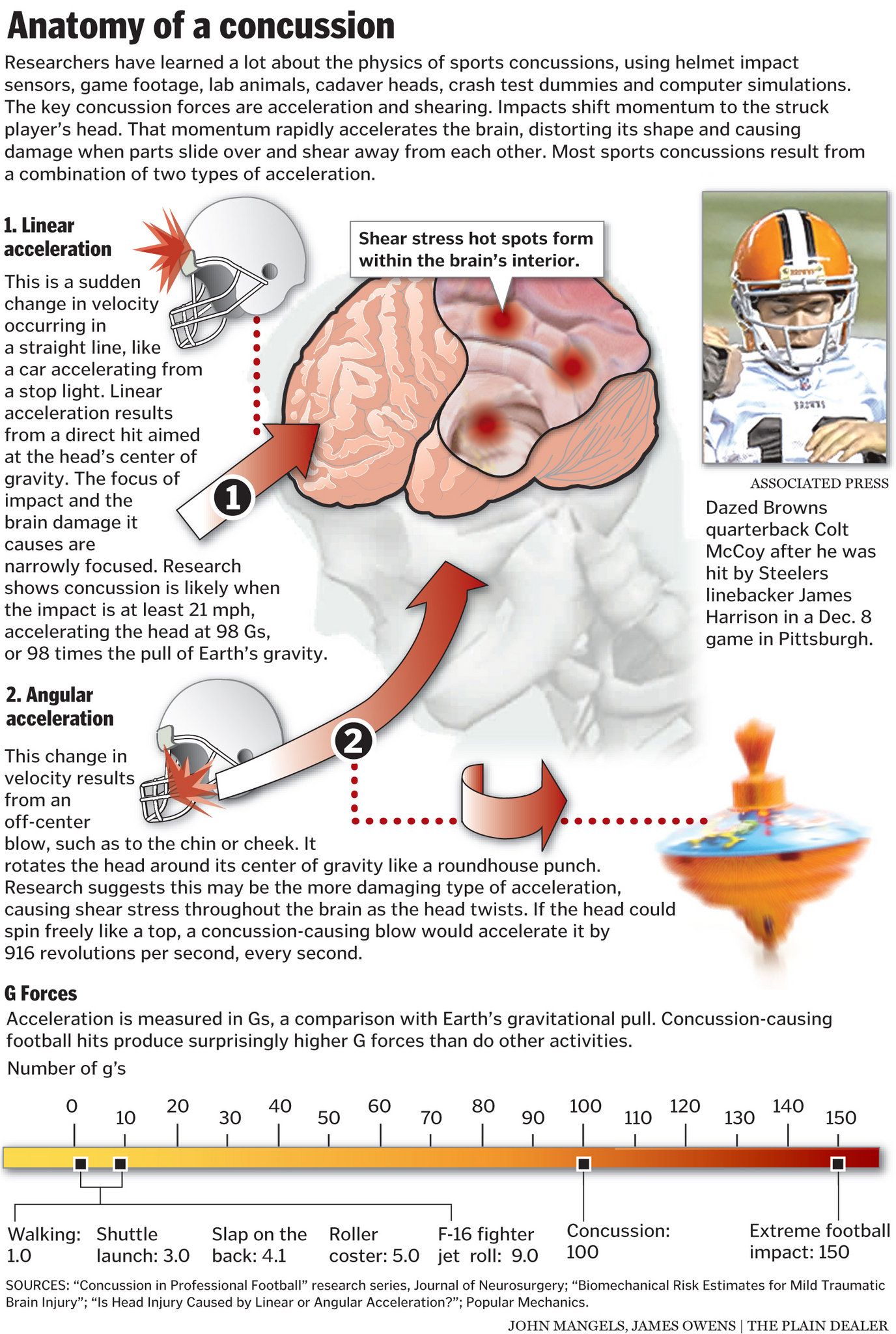
A concussion is a mild traumatic brain injury caused by a forceful blow or jolt to the head or body. It disrupts normal brain function and does not necessarily involve loss of consciousness. For young athletes participating in contact sports like football, soccer, or lacrosse, understanding the implications of concussions is crucial.
Is it safe for a young athlete to return to sports after experiencing a concussion? This question concerns many parents and coaches. The answer lies in seeking guidance from a healthcare provider trained in concussion management. They can assess the athlete’s condition and provide recommendations for a safe return to play.

The Critical Importance of Proper Concussion Recovery
Why is it essential for athletes to refrain from sports activities during concussion recovery? There are several compelling reasons:
- Faster recovery: Research shows that high school athletes removed from play immediately after a concussion recovered twice as fast as those who continued to participate.
- Symptom management: Engaging in strenuous activity soon after a concussion can exacerbate symptoms.
- Risk reduction: A second head injury during recovery can increase the risk of complications, potentially leading to worsening symptoms and prolonged recovery time.
While catastrophic brain injuries resulting in death or permanent neurological damage are extremely rare in youth sports, awareness of their possibility is crucial for immediate identification and appropriate management.
Legal Framework for Concussion Management in Youth Sports
Are there laws governing concussion management in youth sports? Yes, many states have implemented legislation to protect young athletes. In Colorado, for example, the Jake Snakenberg Youth Concussion Act took effect in 2012, establishing safety measures for athletes aged 11 to 18 participating in organized sports.

Key provisions of this law include:
- Mandatory annual concussion recognition training for coaches
- Immediate removal of athletes with suspected concussions from play
- Parental notification of suspected concussions
- Requirement for healthcare provider clearance before return to play
The Impact of Multiple Concussions on Return to Play
How do multiple concussions affect an athlete’s ability to return to sports? While most concussion symptoms typically resolve within a few days to weeks without long-term problems, the situation becomes more complex for athletes who have sustained multiple concussions.
Factors considered in determining return to play after multiple concussions include:
- Number and timing of concussions
- Duration of recovery and required treatment
- Presence of complications or incomplete recovery
- Injury threshold and risk of desired activity
- Athlete and family priorities
In cases of multiple concussions, consulting with a concussion specialist is highly recommended to weigh these factors and make an informed decision.

Debunking the Myth of Second Impact Syndrome
Is there scientific evidence supporting the concept of “second impact syndrome”? This term refers to the belief that two closely spaced concussions result in devastating brain injury. However, recent research has called this phenomenon into question, as studies have not found a direct causal link between back-to-back concussions and severe brain injury.
While catastrophic outcomes can occur after sport-related head injuries, it’s important to note that such incidents are extremely rare. In fact, they occur less frequently than injuries from everyday activities like riding in motor vehicles or cycling.
Assessing Readiness for Return to Play
How can healthcare providers determine if an athlete is ready to return to play after a concussion? There is no single definitive test to make this determination. Instead, a comprehensive approach is necessary, considering various factors:
- Complete resolution of symptoms both at rest and with physical exertion
- Normal neurological examination
- Return to baseline performance on neurocognitive testing
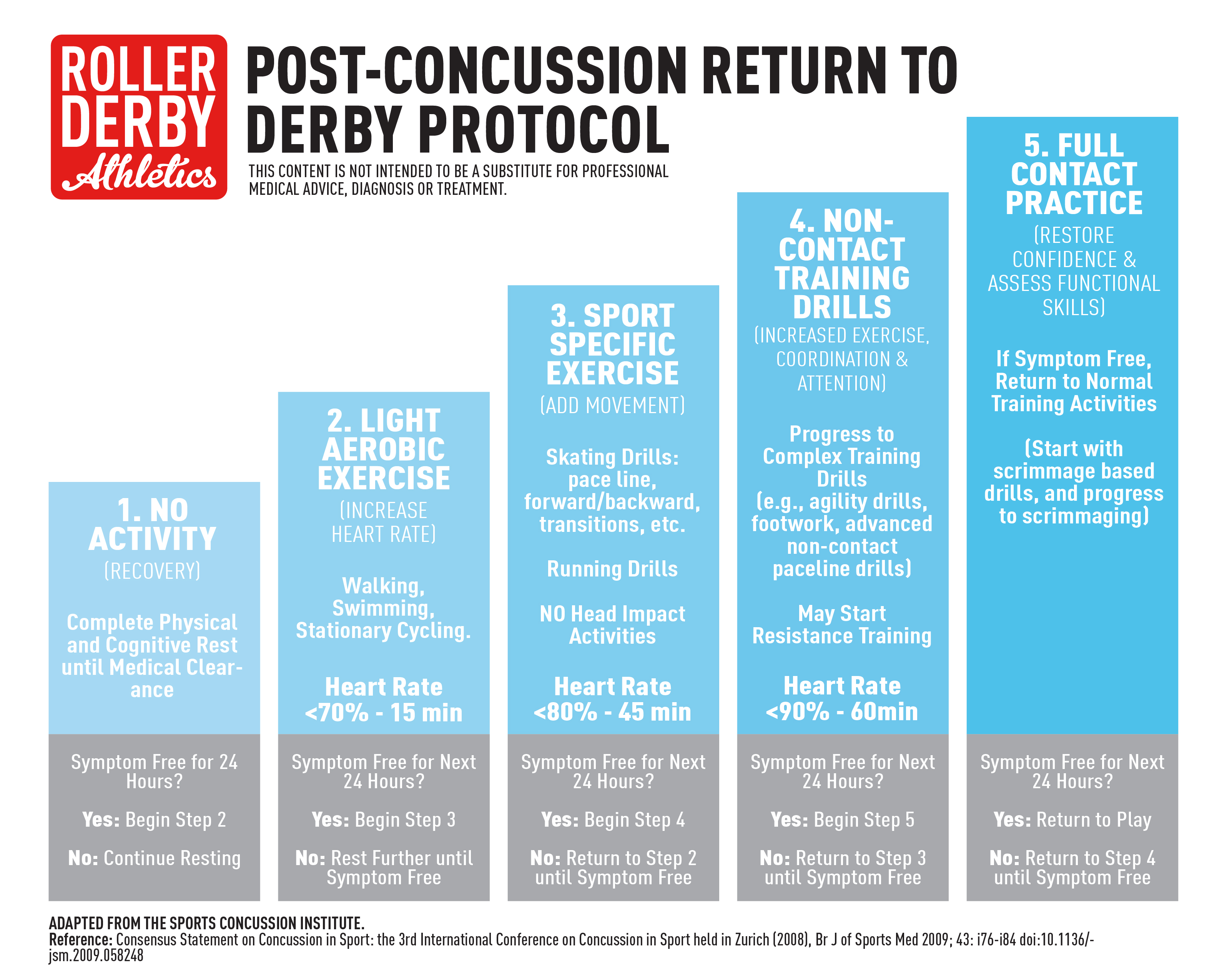
- Successful completion of a graduated return-to-play protocol
The graduated return-to-play protocol typically involves a step-wise progression of activities, starting with light aerobic exercise and advancing to sport-specific training, non-contact drills, full-contact practice, and finally, return to competition.

The Role of Neurocognitive Testing in Concussion Management
What is the significance of neurocognitive testing in managing sports-related concussions? Neurocognitive tests assess various aspects of brain function, including memory, processing speed, and reaction time. These tests can provide valuable information about an athlete’s cognitive recovery following a concussion.
Many sports programs now use computerized neurocognitive testing as part of their concussion management protocol. Athletes typically undergo baseline testing before the season starts, which can then be compared to post-injury test results to help determine when cognitive function has returned to normal.
Types of Neurocognitive Tests
Several computerized neurocognitive tests are commonly used in sports concussion management:
- ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing)
- CogSport
- ANAM (Automated Neuropsychological Assessment Metrics)
- CNS Vital Signs
While these tests provide valuable information, it’s important to note that they should not be used as the sole determinant for return-to-play decisions. A comprehensive approach considering multiple factors is always recommended.

Long-Term Consequences of Concussions in Youth Sports
Are there potential long-term effects of concussions in young athletes? While most athletes recover fully from concussions without lasting effects, there is growing concern about the potential long-term consequences of repetitive head impacts, particularly in contact sports.
Some areas of concern include:
- Chronic Traumatic Encephalopathy (CTE): A progressive degenerative brain disease associated with repetitive head trauma
- Cognitive impairment: Potential difficulties with memory, attention, and executive function
- Mental health issues: Increased risk of depression and anxiety
- Neurodegenerative diseases: Possible increased risk of conditions like Alzheimer’s and Parkinson’s disease
It’s important to note that research in this area is ongoing, and many questions remain about the long-term effects of concussions in youth sports. However, these concerns underscore the importance of proper concussion management and prevention strategies.

Strategies for Concussion Prevention in Youth Sports
How can we reduce the risk of concussions in youth sports? While it’s impossible to eliminate the risk entirely, several strategies can help minimize the occurrence of concussions:
- Proper technique: Teaching and emphasizing proper playing techniques, especially in contact sports
- Rule enforcement: Strict enforcement of rules designed to protect players from dangerous plays
- Equipment: Ensuring athletes use properly fitted, sport-appropriate protective equipment
- Strength and conditioning: Implementing neck and core strengthening exercises to help absorb impact
- Education: Providing comprehensive concussion education to athletes, parents, and coaches
These preventive measures, combined with prompt recognition and appropriate management of concussions when they do occur, can help create a safer environment for young athletes.
The Role of Technology in Concussion Management
How is technology advancing concussion management in sports? Recent years have seen significant technological advancements aimed at improving concussion detection, assessment, and management:

- Impact sensors: Wearable devices that measure the force of impacts to the head
- Virtual reality systems: Used for balance assessment and vestibular rehabilitation
- Mobile apps: Designed for sideline concussion assessment and symptom tracking
- Advanced neuroimaging techniques: Such as functional MRI and diffusion tensor imaging, which can detect subtle brain changes after concussion
While these technologies show promise, it’s important to remember that they are tools to assist in concussion management, not replacements for clinical judgment and comprehensive assessment by trained healthcare providers.
Limitations of Current Technology
Despite the advances in concussion-related technology, there are limitations to consider:
- Impact sensors cannot diagnose concussions and may provide false positives or negatives
- Mobile apps should not replace professional medical assessment
- Advanced neuroimaging techniques are not yet widely available or practical for routine use
As research continues, these technologies will likely become more refined and integrated into comprehensive concussion management protocols.

The Importance of a Multidisciplinary Approach to Concussion Management
Why is a multidisciplinary approach crucial in managing sports-related concussions? Concussions can affect various aspects of an athlete’s health and performance, necessitating input from different healthcare professionals:
- Sports medicine physicians: Provide overall management and return-to-play decisions
- Neurologists: Assess and manage neurological symptoms
- Neuropsychologists: Conduct and interpret neurocognitive testing
- Physical therapists: Address balance and vestibular issues
- Athletic trainers: Provide on-field assessment and ongoing monitoring
- School personnel: Assist with academic accommodations during recovery
This collaborative approach ensures comprehensive care, addressing all aspects of an athlete’s recovery and safe return to sports.
The Future of Concussion Research and Management in Sports
What does the future hold for concussion research and management in sports? As our understanding of concussions continues to evolve, several areas of focus are likely to shape the future of concussion management:

- Biomarkers: Research into blood or saliva biomarkers that could diagnose concussions or predict recovery time
- Genetic factors: Investigating genetic predisposition to concussion and its influence on recovery
- Personalized treatment: Developing individualized management plans based on specific symptoms and risk factors
- Advanced neuroimaging: Refining techniques to detect subtle brain changes and guide treatment
- Long-term effects: Continuing research into the long-term consequences of concussions and repetitive head impacts
These areas of research hold promise for improving our ability to diagnose, manage, and prevent concussions in sports at all levels.
Emerging Treatment Modalities
Several innovative treatment approaches are being explored for concussion management:
- Transcranial magnetic stimulation (TMS): Non-invasive brain stimulation to alleviate persistent symptoms
- Hyperbaric oxygen therapy: Breathing pure oxygen in a pressurized room to promote healing
- Vestibular rehabilitation: Specialized therapy to address balance and dizziness issues
- Cognitive rehabilitation: Targeted exercises to improve cognitive function
While these treatments show promise, more research is needed to establish their efficacy and determine the most appropriate applications in concussion management.

Balancing the Risks and Benefits of Sports Participation
How can we balance the risks of concussions with the benefits of sports participation? This question is at the heart of ongoing discussions about youth sports safety. While the potential risks of concussions and other injuries are concerning, it’s essential to consider the numerous benefits of sports participation:
- Physical health: Improved cardiovascular fitness, strength, and overall health
- Mental health: Reduced risk of depression and anxiety, improved self-esteem
- Social skills: Teamwork, leadership, and communication skills development
- Academic performance: Association with better grades and higher graduation rates
- Life skills: Time management, goal-setting, and perseverance
The key lies in implementing comprehensive safety measures, including proper concussion management protocols, while preserving the valuable aspects of sports participation.
Strategies for Safe Sports Participation
To maximize the benefits of sports while minimizing concussion risks, consider the following strategies:

- Comprehensive education: Ensure athletes, parents, and coaches understand concussion risks and proper management
- Proper technique: Emphasize safe playing techniques and sportsmanship
- Rule enforcement: Strictly enforce rules designed to protect players
- Appropriate equipment: Use properly fitted, sport-specific protective gear
- Balanced approach: Encourage participation in multiple sports to develop diverse skills and reduce repetitive strain
- Open communication: Foster an environment where athletes feel comfortable reporting symptoms
By implementing these strategies, we can create a safer sporting environment that allows young athletes to reap the benefits of sports participation while minimizing the risks of concussions and other injuries.
Play After a Concussion | Children’s Hospital Colorado
A concussion is a type of mild traumatic brain injury caused by a forceful blow or jolt to the head or body that disrupts how the brain normally works. A person does not need to be knocked out or lose consciousness to have a concussion.
Many parents wonder if it is safe for their young athlete to return to playing football, soccer, lacrosse or other sports after a concussion. An appropriately trained healthcare provider can answer these questions and provide guidance on when it is safe and sensible for an athlete to return to sports.
The importance of concussion recovery
Athletes should not be allowed to continue playing sports, including practices and conditioning, while recovering from a concussion for a variety of reasons:
- Recovery time: In one study among high school athletes, athletes who were immediately removed from play after a concussion recovered twice as fast as athletes who continued to participate.

- Worsening symptoms: Strenuous activity soon after a concussion has been associated with worsening symptoms.
- Increased risk: Parents and young athletes should be aware that a second head injury while an athlete is recovering from a concussion can increase the risk of complications, including the potential for worsening symptoms and longer recovery.
Catastrophic brain injuries, such as those that result in death or permanent neurologic injury, are extremely rare in youth sports. Nevertheless, it’s important to understand that they can happen so that they can be identified immediately and appropriately managed.
What laws govern concussion return to play?
The youth sports concussion law (Senate Bill 40, or the “Jake Snakenberg Youth Concussion Act”) took effect in 2012 and puts safety measures in place to help young athletes who suffer from a head injury while playing sports.
- Coaches need to complete a concussion recognition training annually.
 This includes all organized youth sports for kids 11 to 18 years old. This training may be completed through a free online course or through an in-person training by a healthcare professional with expertise in managing concussions.
This includes all organized youth sports for kids 11 to 18 years old. This training may be completed through a free online course or through an in-person training by a healthcare professional with expertise in managing concussions. - Coaches must immediately remove an athlete with a suspected concussion from play. If an athlete has been taken out of a game for a possible concussion, they should not be allowed to return to the game or practice the same day. The athlete will need to sit out of further practices/games until cleared by a healthcare professional.
- Coaches should always notify a parent of any athlete they remove from play due to a suspected concussion. Coaches should also give information to the parents regarding the signs and symptoms of concussion so they can monitor their child at home.
- A healthcare provider must evaluate a player with a suspected concussion and give written clearance for return to play, including practices and games.
How do multiple concussions affect return to play?
Concussion symptoms typically resolve within a few days to a few weeks, and generally there are no long-term problems. Most young athletes can return to sports once a medical provider has cleared them. There is no definite number of concussions that requires retirement or disqualification from sports, as each case should be considered individually. When an athlete has sustained multiple concussions, many factors are considered in the decision to return an athlete to competitive sports, including:
Most young athletes can return to sports once a medical provider has cleared them. There is no definite number of concussions that requires retirement or disqualification from sports, as each case should be considered individually. When an athlete has sustained multiple concussions, many factors are considered in the decision to return an athlete to competitive sports, including:
- Number of concussions
- Timing of concussions (interval between injuries)
- Duration of recovery and required treatment
- Presence of complications or incomplete recovery
- Injury threshold (level of force required to cause injury)
- Injury risk of desired activity
- Athlete and family priorities including the benefits of sports participation
We recommend consulting with a concussion specialist to help weigh the factors above so the parent and athlete can make the best decision for their situation.
What is second impact syndrome?
The idea that two closely spaced concussions results in a devastating brain injury has become known as “second impact syndrome.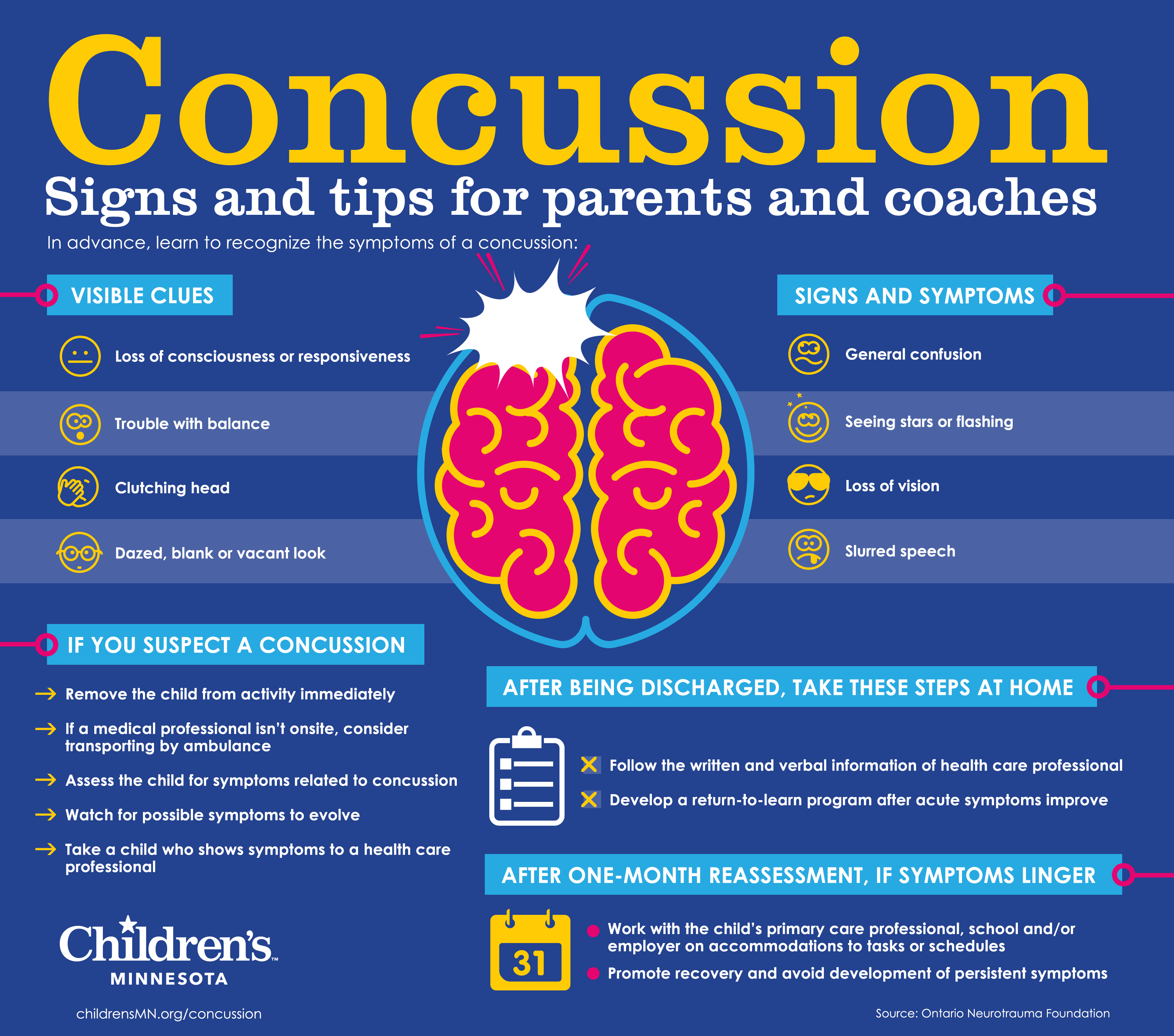 ” However, this phenomenon has come into question because research has not found that back-to-back concussions cause severe brain injury.
” However, this phenomenon has come into question because research has not found that back-to-back concussions cause severe brain injury.
It is important to note that catastrophic outcomes can happen after sport-related head injuries. Fortunately, these outcomes in sports are extremely rare, occurring much less frequently than from activities we let our children do every day, such as riding in motor vehicles or biking. It’s also important to remember that there are many scientifically known benefits to participation in sports including benefits for physical health, academic achievement, and social and emotional functioning.
Determining whether an athlete is ready to return to play
There is no single test that can definitively determine whether an athlete has had a concussion and when they are ready to return to play. Your healthcare provider should determine if the athlete is functioning at their typical level in all areas of life prior to clearance for sports. It can also be helpful to receive information from the athlete, their parents and teachers, as well as peers and coaches if possible.
Our providers typically consider clearance once the athlete is:
- Free of concussion symptoms for at least 24 hours
- Off any medications started for concussion symptoms
- Attending full days of school and tolerating a full academic workload (if applicable, depending on the time of year)
What are baseline cognitive tests?
Certain athletic programs require athletes to take a computerized baseline test before competing on a sport’s team. These tests evaluate the athlete’s cognitive functions to establish a baseline in the event of a concussion during the season. If an athlete is suspected of having a concussion during the season, a second test can be administered and compared to the baseline test. Unfortunately, these tests may not be as reliable or useful as originally thought, and should not be used in isolation to diagnose or manage a concussion.
Theoretically, these tests are appealing because they have the potential to provide additional information about an athlete’s thinking, memory and response speed after a concussion. However, at present, the value of baseline testing remains scientifically questionable, especially for younger athletes.
However, at present, the value of baseline testing remains scientifically questionable, especially for younger athletes.
Returning to school after a concussion
Athletes who have had a concussion should undergo a thorough medical examination soon after injury. After an injury, a brief period of reduced activity and rest may be beneficial (ex. a day or two), but most children won’t need to miss many days of school. For students who could benefit from a gradual transition, returning for partial school days may be worthwhile before advancing to full days.
Learn more about returning to school after a concussion and how to create a concussion comeback plan for students.
Leading the way in concussion care
Children’s Colorado’s Concussion Program is committed to evidence-based, interdisciplinary care tailored to the individual patient, as well as to partnering with referring providers, school personnel and athletic clubs. Our team of board-certified pediatric experts in emergency medicine, sports medicine, rehabilitation, neuropsychology and neurosurgery are joined by certified athletic trainers, psychologists, physical therapists, nurses and other support.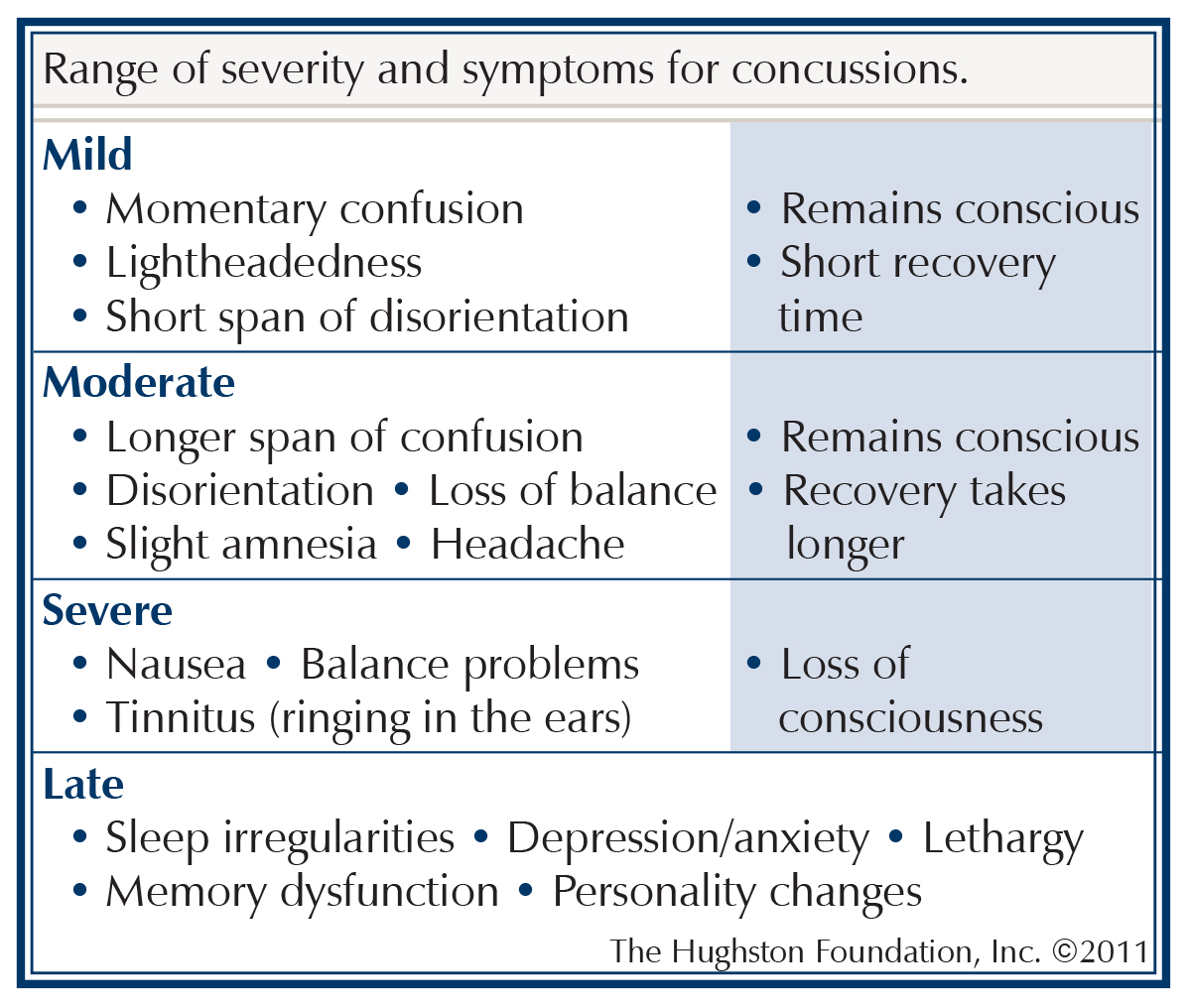 The entire team has special training in concussion to offer a streamlined, comprehensive approach to concussion.
The entire team has special training in concussion to offer a streamlined, comprehensive approach to concussion.
To schedule an appointment or get more information about our Concussion Program, please call 720-777-2806. We are happy to consult with parents or referring providers before a patient is seen at Children’s Colorado.
When Is It Safe to Return to Sports After a Concussion?
Whether you’re a professional or recreational athlete, it can be tough to watch from the sidelines while you heal after a concussion. However, taking time off from your sport is critical to your recovery — and returning to competition too soon can have serious consequences.
According to Christine Greiss, D.O., a physical medicine and rehabilitation specialist and director of the Concussion Program at JFK Johnson Rehabilitation Institute, physicians follow a progression of steps to ensure that athletes are ready to return to post-concussion play.
“We carefully assess each athlete’s physical, cognitive and mental readiness before returning them to play,” says Dr.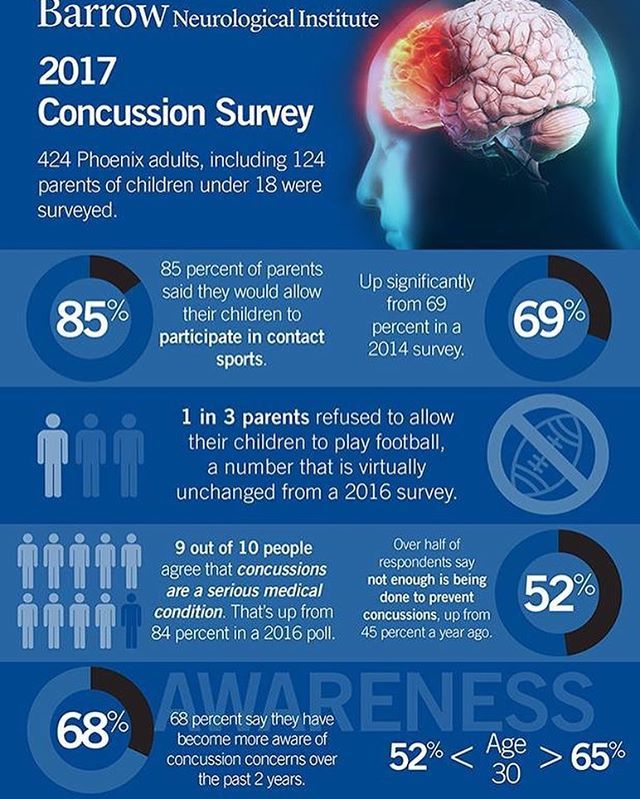 Greiss.
Greiss.
How to Safely Resume Normal Activities and Exercise
Dr. Greiss says that athletes must complete a series of “steps” before returning to competition in their sport. The concussion rehabilitation team at JFK Johnson Rehabilitation Institute follows HEADS UP concussion recovery guidance from the U.S. Centers for Disease Control and Prevention. HEADS UP is a national initiative to raise awareness about brain injuries, including how to recognize, respond to, recover from and reduce the risk of concussion.
A patient’s recovery is typically coordinated by a team that includes:
- A physical medicine and rehabilitation specialist
- A physical therapist
- An occupational therapist
- A speech-language therapist
- A neuropsychologist
- Athletic trainers and coaches
- The patient’s family
Steps in the recovery process typically include:
- Rest. After 1-3 days of rest, the athlete can slowly resume normal activities.

- Monitoring symptoms during routine activities. If symptoms do not worsen with everyday activities, such as school, work, walking or driving, patients move on to a graduated exercise protocol.
- Resuming moderate activity. Starting with light aerobic exercise, athletes progress to moderate activity that involves more body or head movement.
- Resuming heavy activity. Eventually, athletes progress to heavy activity, such as running, weightlifting and non-contact drills.
Throughout the graduated exercise protocol, patients and their care team watch for a return of symptoms and adjust the recovery plan accordingly.
“If an athlete notices that they experience symptoms after their heart rate rises beyond a certain level or they run for a certain period, we will ask them to back off slightly and exercise at a sub-maximum threshold,” shares Dr. Greiss. “Eventually, an athlete can move on to full-contact practices followed by competition as symptoms subside. ”
”
Assessing Cognitive and Mental Recovery
A concussion can cause a range of cognitive symptoms, including problems with memory, attention, concentration and processing. Dr. Greiss says that a neuropsychological evaluation is the gold standard to assess cognitive recovery.
“Before returning to play, we want to make sure our patients are at baseline,” comments Dr. Greiss. “They should have the same grades or work performance, and be able to engage in the same amount of social activity, reading, and studying as they did before their injury.”
Dr. Greiss says that patients also need to demonstrate improvement in mental symptoms, including mood or coping disorders and sleep disturbances. Other symptoms, such as difficulty with social interaction or headaches caused by exertion, can also lead to symptoms of depression or anxiety.
“The brain is the maestro of the body, and when it is injured, it goes into alert,” says Dr. Greiss. “This can induce an anxious state, so we follow up with patients every two weeks to make sure these symptoms are improving.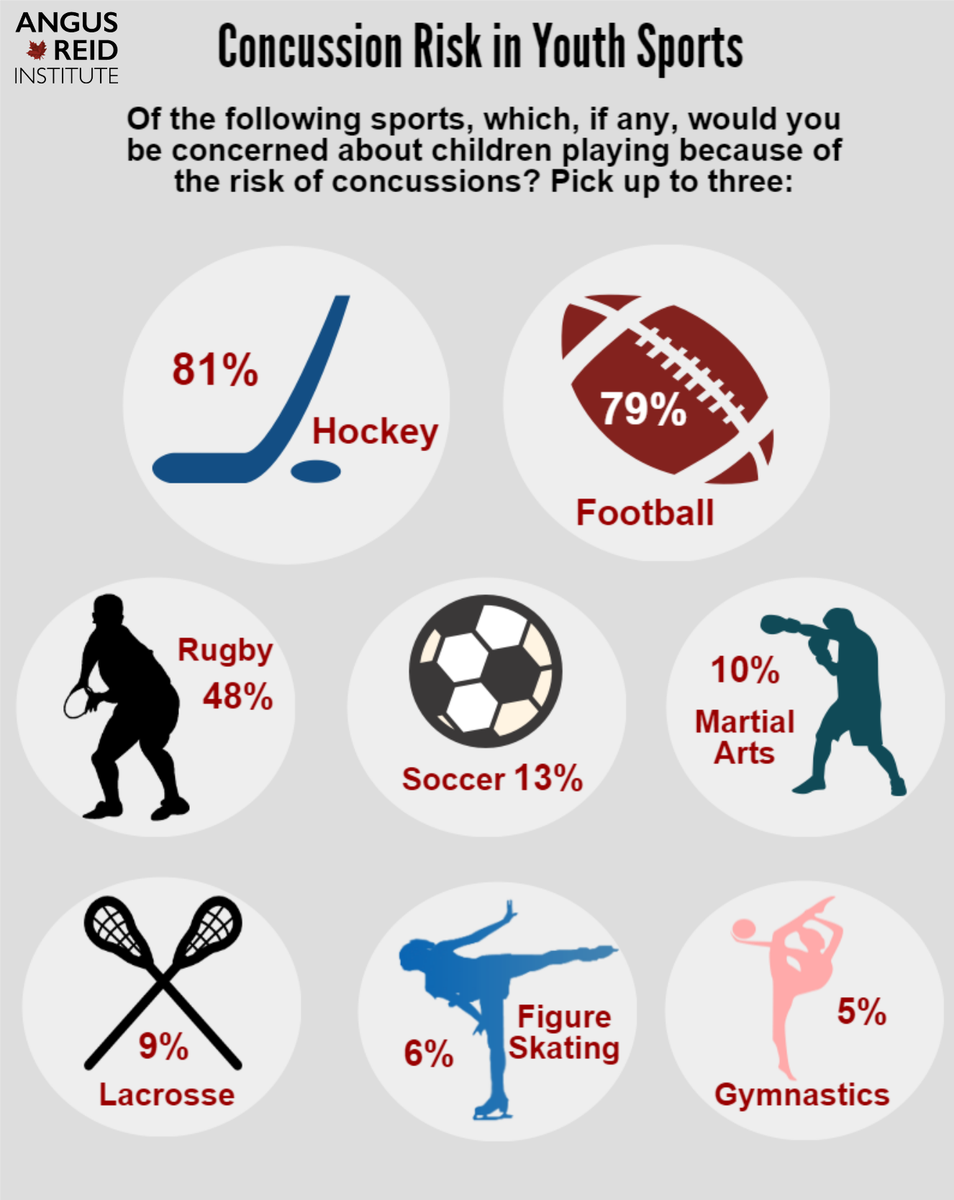 ”
”
Patience Pays Off
Recovering from a concussion isn’t always a quick process, and it can be difficult for athletes to be patient when they want to get back in the game. However, Dr. Greiss says that concussion recovery is one situation where patience pays off.
Returning to sport too early can increase the risk of experiencing a condition called “second impact syndrome,” which occurs when someone sustains a second concussion before symptoms from an earlier concussion have gone away. Second impact syndrome can cause rapid, severe brain swelling that can lead to paralysis and death.
“Even if a patient wouldn’t sustain another concussion, returning to play too early could prolong their recovery,” shares Dr. Greiss.
When the time comes for the patient to return to the sport they love, Dr. Griess says that doing a few things could help prevent future concussions.
“Strengthening and stretching the neck muscles can help the body absorb blows better,” continues Dr.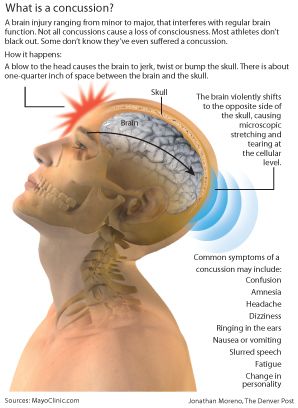 Greiss. “Nutrition and supplementation, protein intake, and getting your body in optimal shape can all help to create a physical and molecular barrier that reduces concussion risk.”
Greiss. “Nutrition and supplementation, protein intake, and getting your body in optimal shape can all help to create a physical and molecular barrier that reduces concussion risk.”
Next Steps & Resources:
- Meet our source: Christine Greiss, D.O. To make an appointment with Dr. Greiss or a doctor near you, call 800-822-8905.
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.
Concussion – causes, symptoms, diagnosis and treatment
- INVITRO
- Library
- Directory of diseases
- Concussion .
 ..
..
Vomiting
Traumatic brain injury
Ringing in the ears
Vertigo
Nausea
Double vision
1298
05 August
Concussion: causes, symptoms, diagnosis and treatment.
Definition
A concussion is a functionally reversible form of a closed craniocerebral injury without organic damage to the brain, caused by a bruise, blow and, in rare cases, as a result of a sudden movement of the head.
Causes of concussion
Concussion can be the result of a traffic accident, a fall, domestic, sports and industrial injuries, as well as injuries resulting from street fights and collisions during mass events, exposure to a blast wave. Even a seemingly minor head injury can lead to a concussion.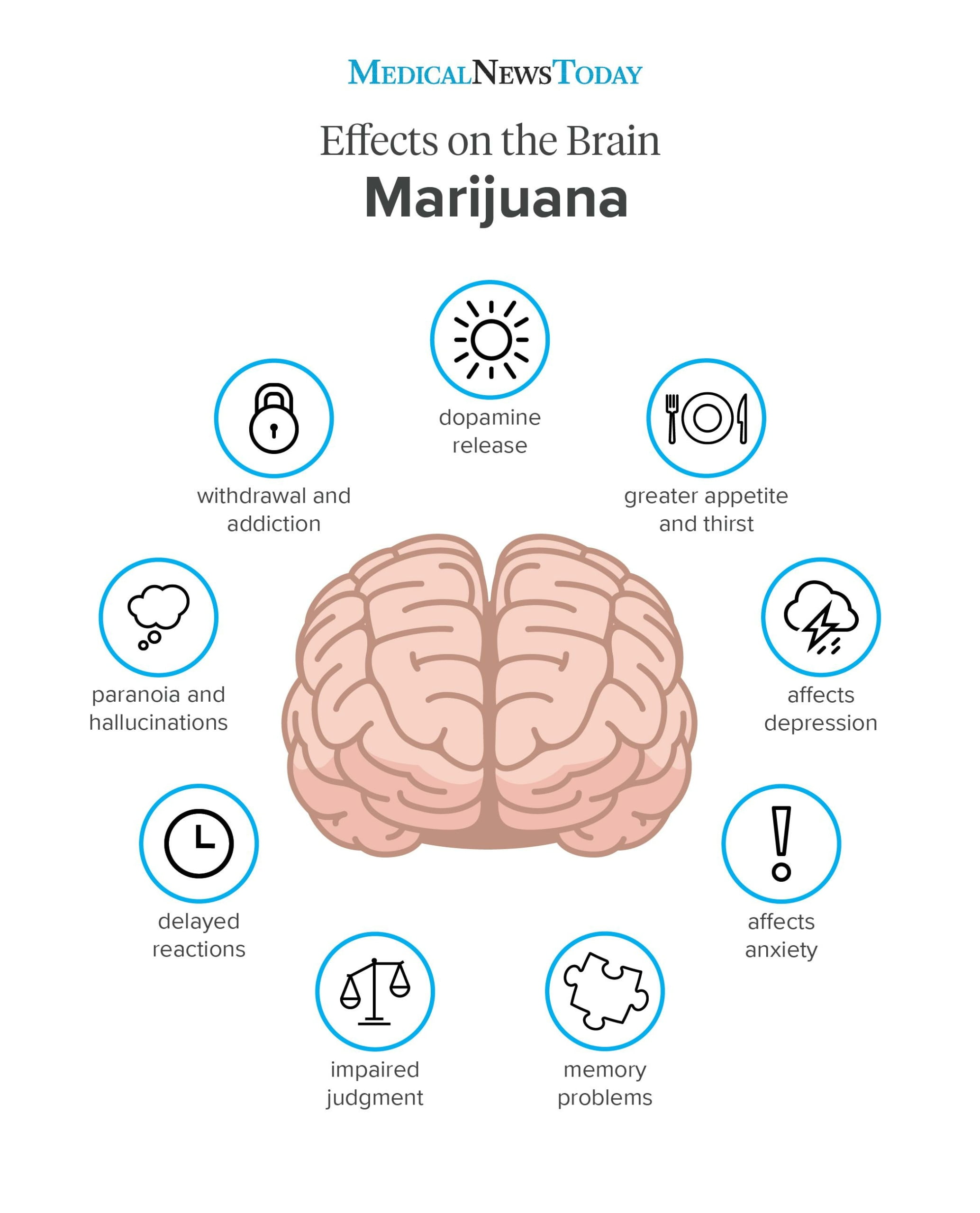 Thus, the fact of the presence of an injury may already indicate a possible concussion.
Thus, the fact of the presence of an injury may already indicate a possible concussion.
The mechanism of concussion is not exactly known. Most likely, as a result of an injury, certain problems arise with the work of nerve cells in the brain (neurons). It is assumed that there is a functional disconnection between the brain stem and hemispheres. It is believed that due to concussion there is a temporary disruption of interneuronal connections. A slight displacement of the layers of the brain tissue may appear, their nutrition may worsen, and the connection between some brain centers will go wrong, which contributes to the development of functional disorders. At the same time, macroscopic and histological changes in the brain tissue are not detected.
Among all brain injuries, concussion ranks first in frequency. Most patients recover within 1-2 weeks.
If over time the patient’s condition continues to deteriorate, and more severe forms of traumatic brain injury are excluded, then it is necessary to look for other causes of the existing symptoms – psychological problems, mental illness, side effects of drugs or other concomitant diseases.
Disease classification
According to the International Classification of Diseases (ICD-10), concussion has the code S06.0. This nosology is one of the clinical forms of traumatic brain injury.
Depending on the severity of the patient’s condition and clinical symptoms, there are three degrees of concussion.
Mild concussion . The victim has no impairment of consciousness, but disorientation, headache, dizziness, nausea may occur during the first 20 minutes after the injury. Then the general state of health returns to normal. Perhaps a short-term increase in body temperature (37.1-38 ° C).
Moderate concussion . Although the victim does not lose consciousness, pathological symptoms such as headache, nausea, dizziness, and disorientation may be observed. All of them last more than twenty minutes. There may be short-term memory loss (amnesia), most often retrograde amnesia with loss of several minutes of memories preceding the injury.
Severe concussion . Necessarily accompanied by loss of consciousness for a short period of time, usually from several minutes to several hours. The victim does not remember what happened – retrograde amnesia develops. Pathological symptoms bother a person for 1-2 weeks after the injury (headache, dizziness, nausea, fatigue, disorientation, impaired appetite and sleep).
Symptoms of the concussion of the brain
Physical (somatic) symptoms :
- Dizziness, which, when changing the body position, turning or tilting of the head, is intensified – this is explained by a violation of blood circulation in the vestibular apparatus;
- throbbing headache;
- nausea;
- single vomiting;
- rapid breathing, tachycardia;
- blurred vision or double vision;
- flashing flies or stars before the eyes;
- imbalance;
- hypersensitivity to light or noise;
- ringing, tinnitus.

Behavioral, emotional symptoms :
- drowsiness;
- increased fatigue or general weakness;
- irritability;
- depression;
- anxiety;
- excessive hours of sleep;
- difficulty falling asleep.
Cognitive symptoms :
- lethargy and incoordination;
- short-term confusion;
- slow incoherent speech;
- difficulty concentrating;
- memory difficulties.
Diagnosis of concussion
Diagnosis of concussion is established on the basis of history, examination and exclusion of more severe traumatic brain injury.
The doctor examines the entire body of the patient for abrasions, bruises, joint deformities, changes in the shape of the chest and abdomen, and bleeding.
In the first hours after a concussion, the victim’s pupils are dilated or constricted – a traumatic brain injury of any severity leads to disruption of the nerve pathways responsible for the functioning of the eyes. Pupillary reaction to light is normal. The victim complains of pain when moving the eyes to the sides, there is a small horizontal nystagmus (involuntary tremulous movements of the eyeballs), if the eyes are taken to the most extreme positions. There may be slight asymmetry of tendon reflexes, unsteadiness in the Romberg position (legs together, straight arms extended forward to a horizontal level, eyes closed). The level of consciousness is assessed on the Glasgow Coma Scale and is 14-15 points.
Pupillary reaction to light is normal. The victim complains of pain when moving the eyes to the sides, there is a small horizontal nystagmus (involuntary tremulous movements of the eyeballs), if the eyes are taken to the most extreme positions. There may be slight asymmetry of tendon reflexes, unsteadiness in the Romberg position (legs together, straight arms extended forward to a horizontal level, eyes closed). The level of consciousness is assessed on the Glasgow Coma Scale and is 14-15 points.
The list of laboratory tests includes:
- complete blood count;
Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram.
Brief description of the study CBC: general a…
Up to 1 business day
Available with house call
RUB 810
Add to cart
General urinalysis (Urine analysis with sediment microscopy)
Method of determination
Determination of physical and chemical parameters is carried out on an automatic analyzer using the “dry chemistry” method.
Hardware microscope…
Up to 1 working day
Available with house call
410 RUB
Add to cart
Specific changes in the blood, urine and cerebrospinal fluid during concussion should be absent.
Instrumental diagnostics includes:
- x-ray of the skull – no skull fractures in concussion;
X-ray of the skull
X-ray examination of the skull to detect structural and integrity disorders of the skull bones of various nature.
RUB 2,290
Sign up
CT scan of the brain and skull
Scanning of the brain, skull and surrounding tissues, which allows diagnosing various pathologies.
RUB 4,890
Sign up
MRI of the brain
Safe and informative scanning of brain structures for the diagnosis of its pathologies.
RUB 5,640
Sign up
Electroencephalography (EEG)
EEG is a safe and painless method for studying the functional state of the brain.
RUB 3,090
Sign up
Transcranial Doppler Ultrasound
Ultrasound scanning to assess the consistency of cerebral blood flow.
RUB 2,690
Sign up
An MRI of the spine may be needed to rule out spinal problems.
MRI of the cervical spine
Examination to assess the condition of the cervical spine.
RUB 5,990
Sign up
Differential diagnosis is carried out with a brain contusion, asthenic condition of the patient, psychoemotional lability, alcohol intoxication, vegetovascular dystonia, postconvulsive syndrome.
Which doctors to contact
If you have a concussion, you need to contact a traumatologist. He examines the patient, collects an anamnesis, checks reflexes, prescribes an x-ray of the skull, and if a more complex brain injury is suspected, he sends him for a consultation to
neurologist or neurosurgeon.
Indication for specialist consultation:
- consultation
otorhinolaryngologist to exclude pathologies of the ear, throat, nose; - consultation of an ophthalmologist in order to exclude or confirm violations of the visual apparatus;
- consultation
therapist for the purpose of correcting the treatment of concomitant pathology; - consultation
surgeon, maxillofacial surgeon and other narrow specialists according to indications.
Treatment of a concussion
If a concussion is suspected, first aid must be given to the victim, providing him with complete rest. It is necessary to lay a person in a quiet darkened room, it is better to raise his head slightly. It is very useful to apply cold compresses to the head. Patients with a concussion should remain in bed for at least a few days.
If you have a concussion, you can not read, listen to loud music and watch TV. It is not recommended to drink a lot. Alcohol is strictly prohibited!
Within 12 weeks after the injury, the patient should be under the supervision of a doctor in order to assess their condition and fully return to daily activity. To date, there are no effective drugs that accelerate the recovery period.
Non-narcotic analgesics, tranquilizers, hypnotics, sedatives are used as medicines. As a rule, this is enough.
In some cases, drugs are used to relieve cerebral edema, suppress the gag reflex, as well as antihistamines. If any vegetative symptoms are excessively expressed, then, for example, b-blockers may be required (with severe tachycardia and hypertension). Conduct courses of nootropic and metabolic therapy.
If any vegetative symptoms are excessively expressed, then, for example, b-blockers may be required (with severe tachycardia and hypertension). Conduct courses of nootropic and metabolic therapy.
Hospitalization is indicated within three days after injury. The indication for emergency hospitalization is the fact of injury or the presence of severe cerebral and autonomic symptoms.
Complications
It must be remembered that a person who has suffered even a mild concussion may develop post-traumatic neurosis or other more serious complications, such as epilepsy. Approximately 3% of patients experience complications in the form of persistent asthenic syndrome, insomnia, migraines, intracranial hypertension and other conditions. Therefore, some time after recovery, you should definitely visit a neurologist and perform electroencephalography.
The consequences of a concussion of the brain can appear in a few years, significantly complicating the usual life.
The hardest thing is for those who, for one reason or another, did not seek medical help in time for the timely diagnosis of the problems that have arisen.
Concussion prevention
Concussion prevention consists of following the following rules: sports games;
Sources:
- Big Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 24.
- Mild traumatic brain injury: clinical guidelines / Potapov A.A., Likhterman L.B., Kravchuk A.D. etc. – M.: Association of Neurosurgeons of Russia, 2016. – 23 p.
- Golovacheva V.A., Evzikov G.Yu. Management of a patient with a concussion. iDoctor 2014; 10(29): 60-63.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment.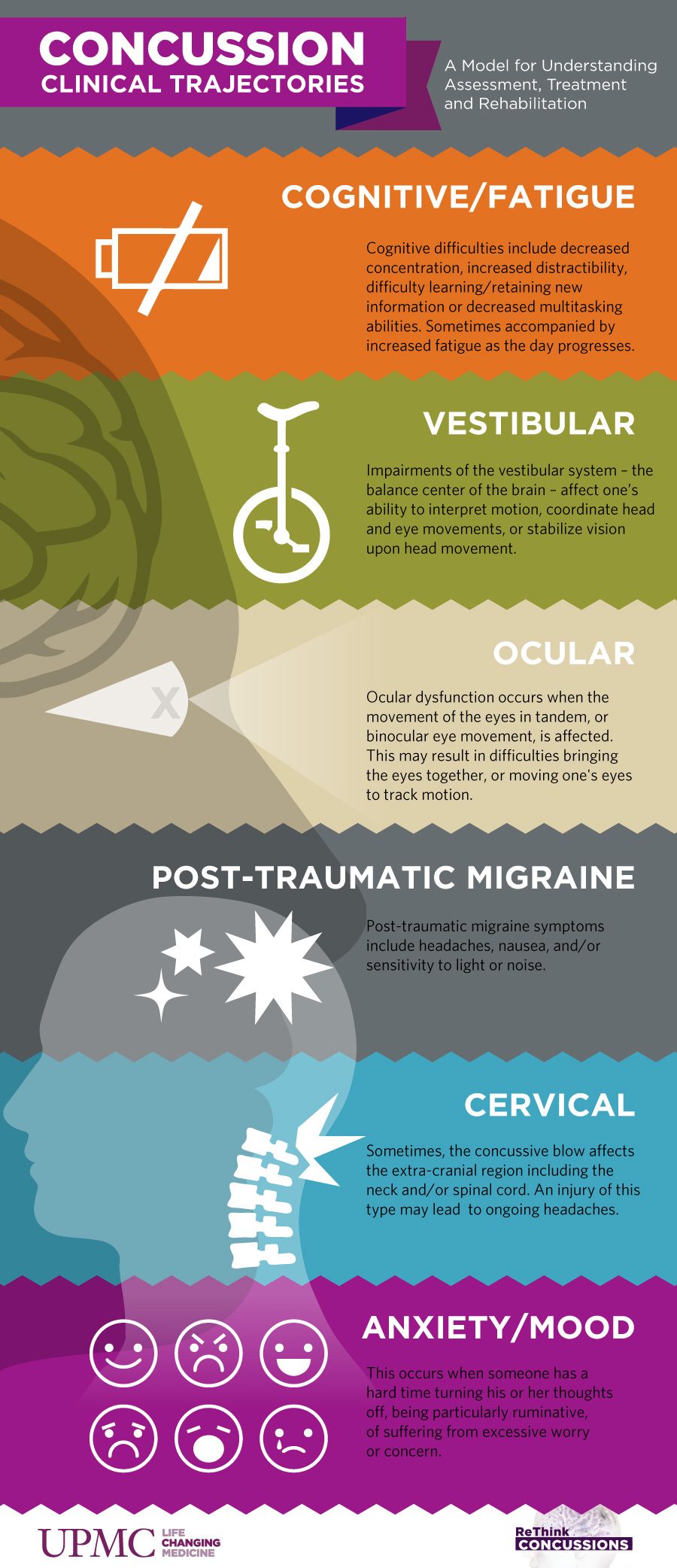 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories can use different research methods and units of measurement to perform the same analyzes.
Recommendations
Chronic cerebral ischemia
770
July, 12
Hemoblastoses (malignant diseases of the hematopoietic system, blood cancer)
768
08 July
Achalasia cardia (achalasia of the esophagus, spasm of the esophagus)
767
07 July
Show more
Meningomyelitis
Meningitis
Tabes dorsalis
Paralysis
Photophobia
Confusion
Convulsions
Violation of urine emissions
Neurosyphilis
Neurosyphilis: causes, symptoms, diagnosis and treatment.
More
Jaundice
Encephalitis
Diarrhea
Leptospirosis
Leptospirosis: causes, symptoms, diagnosis and treatment.
More
Pharyngitis
Angina
Gastroenteritis
Enteritis
Lymphadenitis
Lymphangitis
Allergy
9001 2 Toxins
Jaundice
Toxic hepatitis
Nausea
Pseudotuberculosis
Pseudotuberculosis: causes, symptoms, diagnosis and treatment.
More
Diabetes mellitus
Optic nerve atrophy
Hyperopia
Iridocyclitis
Blindness
Glaucoma
Glaucoma: causes, symptoms, diagnostics and methods of treatment.
More
Diarrhea
Intoxication
Paralysis
Facial nerve paresis
Botulism
Botulism: causes, symptoms, diagnosis and treatment.
More
Nothing found
Try editing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select
doctor from list
Medical office not found
Try changing your query or select
medical office from the list
Therapist
Traumatologist-orthopedist
Endocrinologist
Urologist
Gynecologist
Ultrasound doctor
Cardiologist
Pediatrician
Nothing found
Please try editing your query
Thank you!
You have successfully made an appointment
Detailed information was sent to your e-mail
Physical activity as an aid in the treatment of concussions
ARTICLE
Sports injuries with concussions in adolescence are a serious health and education problem. The reason is the lack of effective mechanisms for the treatment and rehabilitation of such children: more than 30% of adolescents report negative symptoms a month after such injuries.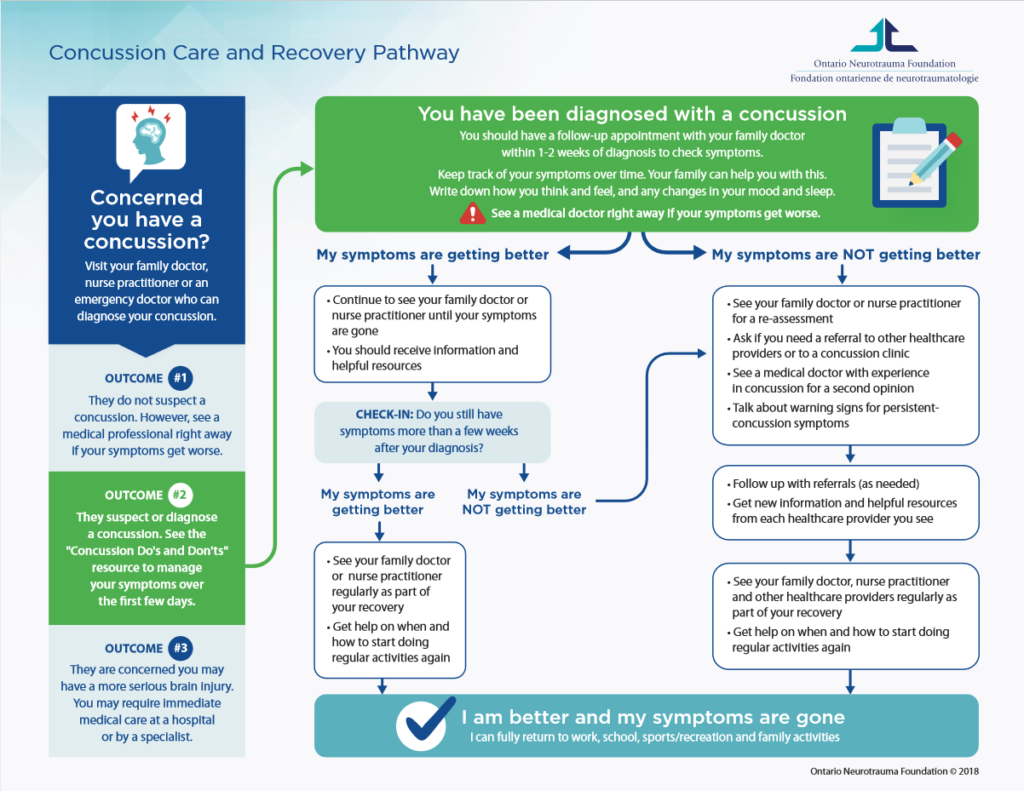 In this regard, the earliest possible restoration of physical conditions allows patients to resume sports activities as soon as possible.
In this regard, the earliest possible restoration of physical conditions allows patients to resume sports activities as soon as possible.
The generally accepted standard of care for patients with concussion is minimal activity until complete regression of symptoms.
However, some recent studies have shown that moderate physical activity or aerobic exercise (again, not maximally strenuous) does not cause harm and even benefits in allowing adolescents to return to their usual physical activity more quickly after a sports concussion.
To see this, let’s compare the effectiveness of subthreshold aerobic exercise with a placebo-like stretching program among traumatized adolescents.
Background
Randomized clinical trial conducted by UBMD Orthopedics & Sports Medicine, a division of the State University of New York. The study included 103 adolescents aged 13 to 18 who had a sports concussion during the last week. Participants were taken into the study from September 2015 to June 2018.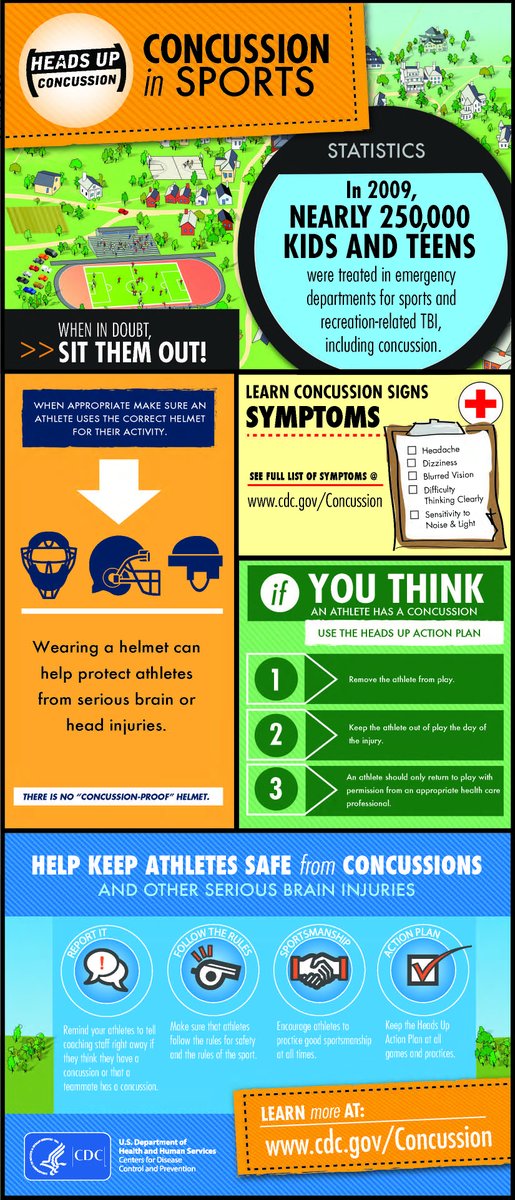 All of them were diagnosed with mild concussion according to the International Concussion in Sport Group criteria.
All of them were diagnosed with mild concussion according to the International Concussion in Sport Group criteria.
Groups were formed randomly, without reference to gender. In the group for aerobic exercises with subthreshold load, 52 people were selected, for stretching exercises (placebo-like), 51 teenagers were selected.
Organization of the study
Those who fell into the first group took classes on a treadmill or exercise bike with dosed loads. Used fitness trackers and were instructed not to do any other exercise.
Both groups (both exercise and stretching), for the duration of the training sessions, were fitted with heart rate monitors. For both groups, the same conditions of rest were created.
Results of the study
Statistical analysis of the collected data showed that adolescents from the first group recovered in 13 days, while in the stretching group, the recovery lasted 17 days. After 30 days from the moment of injury, delayed symptoms persisted in 7 children from the stretching group and only 2 from the main group receiving aerobic exercise.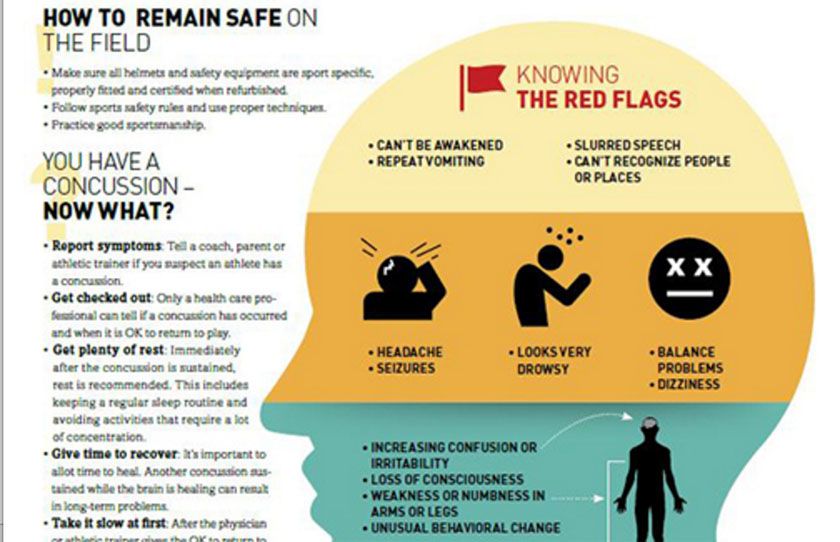

 This includes all organized youth sports for kids 11 to 18 years old. This training may be completed through a free online course or through an in-person training by a healthcare professional with expertise in managing concussions.
This includes all organized youth sports for kids 11 to 18 years old. This training may be completed through a free online course or through an in-person training by a healthcare professional with expertise in managing concussions.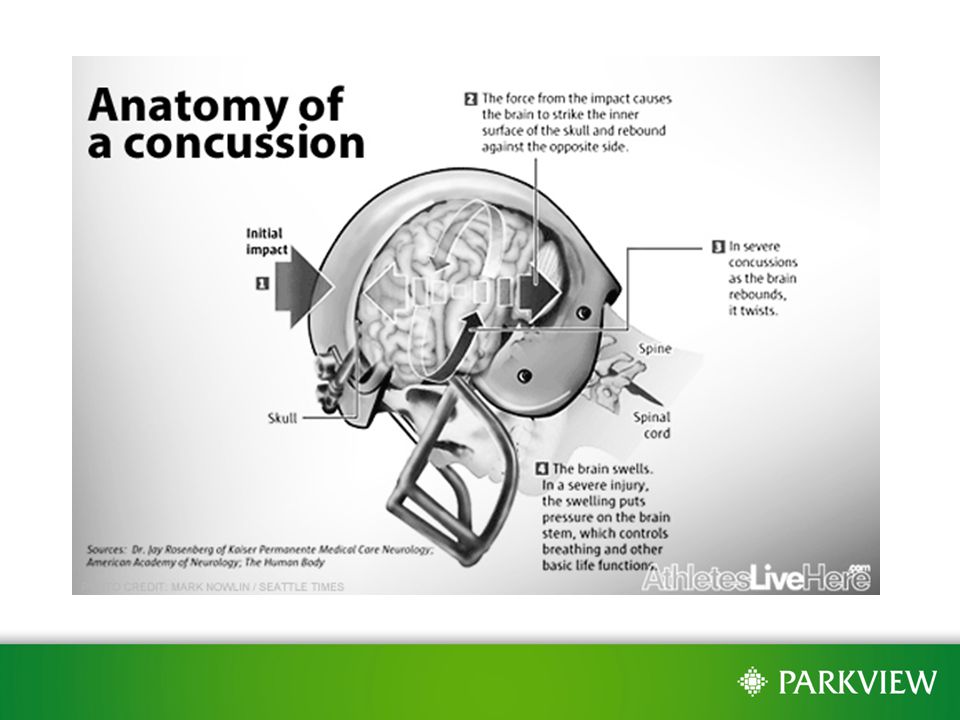
 ..
..